Bone health status of postmenopausal Chinese women
Hong Kong Med J 2015 Dec;21(6):536–41 | Epub 16 Oct 2015
DOI: 10.12809/hkmj154527
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Bone health status of postmenopausal Chinese women
Sue ST Lo, MD, FRCOG
The Family Planning Association of Hong Kong, 10/F, Southorn Centre, 130 Hennessy Road, Wanchai, Hong Kong
Corresponding author: Dr Sue ST Lo (stlo@famplan.org.hk)
Abstract
Objectives: To evaluate the prevalence of
osteoporosis in treatment-naïve postmenopausal
women, their treatment adherence, and the risk
factors for osteoporosis.
Design: Cross-sectional study of bone density
reports, a self-administered health checklist, and
computerised consultation records.
Setting: Primary care sexual and reproductive health
service in Hong Kong.
Participants: Postmenopausal Chinese women
who had never received osteoporosis treatment or
hormone replacement therapy.
Intervention: Each woman completed a checklist of
risk factors for osteoporosis, menopause age, history
of hormone replacement therapy, and osteoporosis
treatment prior to undergoing bone mineral density
measurement at the postero-anterior lumbar spine
and left femur. The consultation records of those
with osteoporosis were reviewed to determine their
treatment adherence.
Main outcome measures: T-score at the spine
and hip, presence or absence of risk factors for
osteoporosis, and treatment adherence.
Results: Between January 2008 and December
2011, 1507 densitometries were performed for
eligible women; 51.6% of whom were diagnosed with
osteopenia and 25.7% with osteoporosis. The mean
age of women with normal bone mineral density,
osteopenia, and osteoporosis was 57.0, 58.0, and
59.7 years, respectively. Approximately half of them
had an inadequate dietary calcium intake, performed
insufficient weight-bearing exercise, or had too little
sun exposure. Logistic regression analysis revealed
that age, body mass index of <18.5 kg/m2, parental
history of osteoporosis or hip fracture, and duration
of menopause were significant risk factors for
osteoporosis. Among those with osteoporosis, 42.9%
refused treatment, 30.7% complied with treatment,
and 26.3% discontinued treatment or defaulted
from follow-up. Those who refused treatment were
significantly older.
Conclusions: Osteoporosis is prevalent in
postmenopausal women. Only 50% adopted primary
prevention strategies. Almost 70% refused treatment
or stopped prematurely.
New knowledge added by this study
- Osteoporosis affects one in four postmenopausal Chinese women in Hong Kong.
- Age, body mass index of <18.5 kg/m2, a positive parental history of osteoporosis or hip fracture, and duration of menopause are significant risk factors for osteoporosis.
- Only 31% of osteoporotic women complied with the treatment protocol.
- This study showed that osteoporosis is prevalent in Hong Kong Chinese postmenopausal women. Doctors should encourage postmenopausal women to have an adequate calcium intake, perform sufficient weight-bearing exercise, and have enough sun exposure. Those with risk factors should also undergo dual-energy X-ray absorptiometry to ascertain their bone status.
- Drug compliance is a problem in those with osteoporosis. Patient education should be provided to help them understand the importance of treatment compliance, the risk of fracture, and osteoporosis-associated morbidity and mortality.
Introduction
Osteoporosis is a major health problem in the elderly
causing significant morbidity, mortality, and socio-economic
burden. Women are more vulnerable to
osteoporosis than men because they have smaller
and thinner bones. In addition, the sudden drop in
ovarian oestrogen production around menopause
causes women to lose bone rapidly. Accelerated bone
loss begins about 2 to 3 years before the last menses
and continues until 3 to 4 years after menopause.
There is 2% bone loss annually around menopause,
slowing to 1% to 1.5% annually thereafter.1 2 Bone mineral density (BMD) measurement by central
dual-energy X-ray absorptiometry (DXA) is the gold
standard for diagnosing osteoporosis. Bone mineral
density is compared with the mean peak BMD
for young adults of the same sex and ethnicity to
calculate a T-score. The World Health Organization
(WHO) defines osteoporosis as a BMD 2.5 standard
deviations (SDs) below that of young-adult BMD and
osteopenia as a BMD 1.0 to 2.5 SD below.3 A meta-analysis
of prospective and case-control studies of
BMD and fracture risk showed that the predictive
value of BMD for fracture is at least as good as that
of blood pressure for stroke.4 In a recent prospective
study of postmenopausal Chinese women, the
relative risk of fracture increased 2-fold (95%
confidence interval [CI], 1.6-2.5) for each decrease
in SD of mean femoral-neck BMD.5
With urbanisation and adoption of a more
sedentary lifestyle, the age-specific incidence of hip
fracture in Hong Kong women increased by 300%
between 1966 and 1985.6 The incidence levelled off
between 1985 and 1995.7 Between 1995 and 2004,
the incidence declined by 50% in those aged 50 to
59 years but remained stable for other age-groups.8
Although the age-specific incidence rates stabilise,
the absolute number of hip fractures will continue
to increase because of the ageing population. It has
been estimated that in Hong Kong, 5293 women
will have a hip fracture in the year 2015.9 The local
prevalence of vertebral fracture in women has
been estimated to be 30%.10 Osteoporotic fractures
increase the morbidity and mortality of individuals
and are a considerable burden on the health-care
system. After the first fracture, the risk of subsequent
fracture of an individual is 2.2 times higher than
that of an individual without a prior fragility
fracture (95% CI, 1.9-2.6).11 Primary care physicians
play a pivotal role in preventing this fracture
cascade in postmenopausal women. They can help
postmenopausal women improve bone health by
encouraging them to adopt primary prevention
strategies for osteoporosis and fall that may cause
fracture; increasing their awareness of their personal
risk for osteoporosis and taking action to minimise
those risks; providing DXA assessment when
indicated; and treating women who are diagnosed
with osteoporosis.12 Pharmacological treatment can
reduce the risk of osteoporotic fractures by 30% to
70%. Treatment failure is partly due to poor drug
compliance with treatment. In a systematic review
of osteoporosis treatment with bisphosphonates,
the yearly drug compliance rate was only 42.5% to
54.8%.13
The objectives of this study were to evaluate
the prevalence of osteoporosis in treatment-naïve
postmenopausal Chinese women, and determine
the risk factors associated with osteoporosis and
treatment compliance in those diagnosed with
osteoporosis. These results will help physicians
understand the bone health status of postmenopausal
Chinese women.
Methods
Postmenopausal women who attend the Women’s
Health Service in Hong Kong for menopause assessment are
offered DXA testing of the spine and hip. Since
a charge is made for the test, it is not universally
accepted. The number of women who refused
DXA was not captured. Prior to undergoing DXA,
women completed a checklist of risk factors that
included a history of parental osteoporosis or hip
fracture, personal low trauma fracture, smoking
habit, drinking habit, calcium intake, exercise
habit, sun exposure, use of medication or presence
of disease that causes bone loss, number of falls
in the past 12 months, previous use of hormone
replacement therapy, previous use of osteoporosis
drugs, and current osteoporosis treatment. The
BMD at the postero-anterior lumbar spine (L1-L4)
and left femur (total hip, trochanter, Ward’s triangle,
and femoral neck) was measured using a Hologic
QDR4000 machine (Hologic Inc, Bedford [MA],
US) and performed by a single operator. The DXA
report provided data on age, menopause age, body
mass index (BMI), BMD, T-score, and Z-score. The
checklist and DXA report were filed together by date.
This analysis was conducted by searching
through paper records completed between January
2008 and December 2011. The research protocol
was approved by the Ethics Panel of the Family
Planning Association of Hong Kong. Non-Chinese
women and those previously or currently prescribed
hormone replacement therapy or osteoporosis
treatment were excluded. The computerised
consultation records of those with osteoporosis were
searched to obtain treatment history. Our clinic only
provides oral osteoporotic drugs (raloxifene, weekly
alendronate, monthly ibandronate and strontium
ranelate). The treatment plan, risks, and benefits
of each drug, specific prescription required of each
drug, and contra-indications are discussed with the
patient before deciding the drug therapy. Patients
are involved in decision making and must pay for
treatment.
Descriptive statistics for basic demographic
factors, risk factors for osteoporosis, T-score
distribution, and treatment adherence were
presented. Women were categorised into three
subgroups according to their T-score and based on
WHO recommendations3: normal BMD (T-score
≥-1.0 at either the hip or spine), osteopenia (T-score
between <-1.0 and -2.5), and osteoporosis (T-score
<-2.5). The Chi squared test was used to test
for a significant association between categorical
risk factors and osteoporosis. Stepwise binomial
logistic regression analysis using factors found to
have a significant correlation with BMD of T-score
of <-2.5 was performed to identify risk factors that
best predict osteoporosis. Analysis of variance was
used to analyse the difference between group means.
Level of significance was set at alpha = 0.05 for the
two-tailed tests. Data analyses were performed
using the Statistical Package for the Social Sciences
(version 23.0; IBM, New York, US).
Results
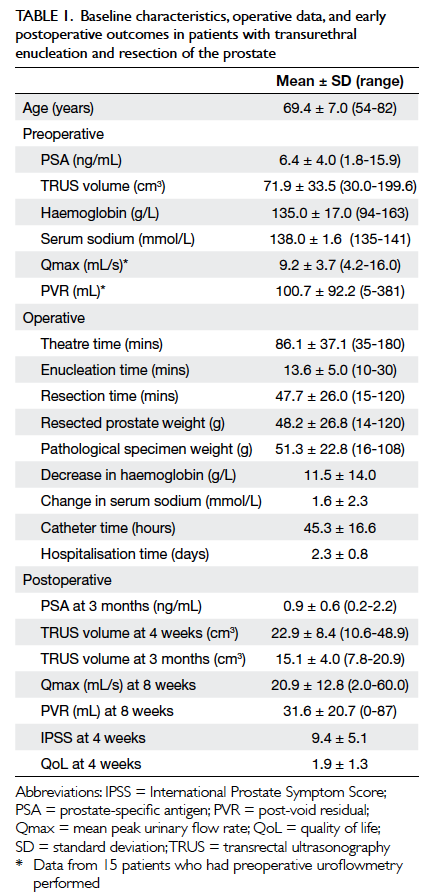
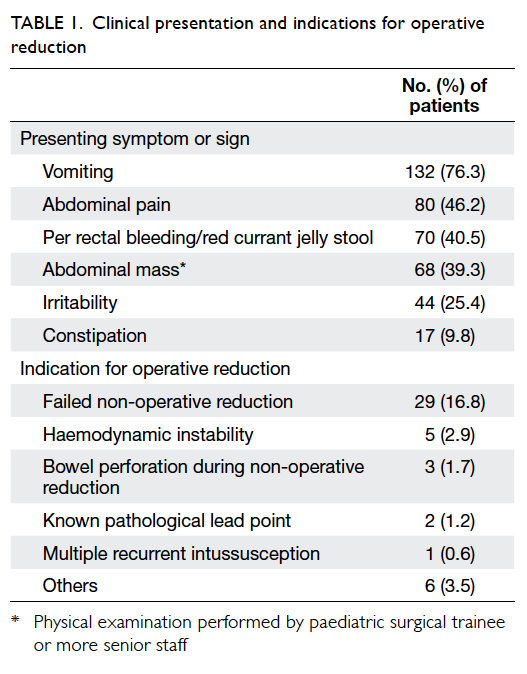
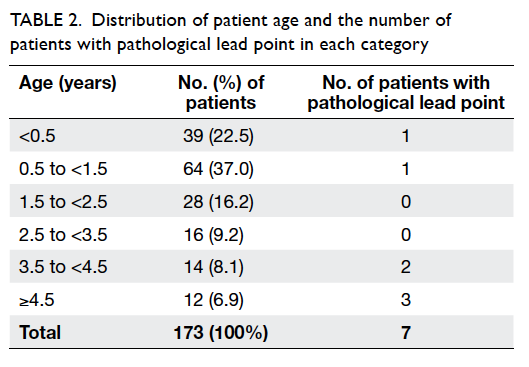
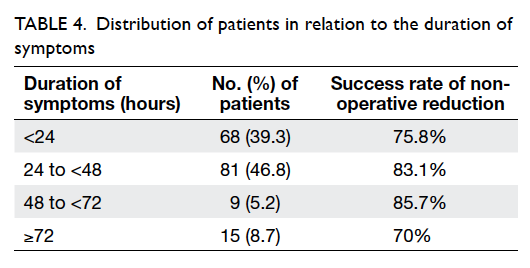
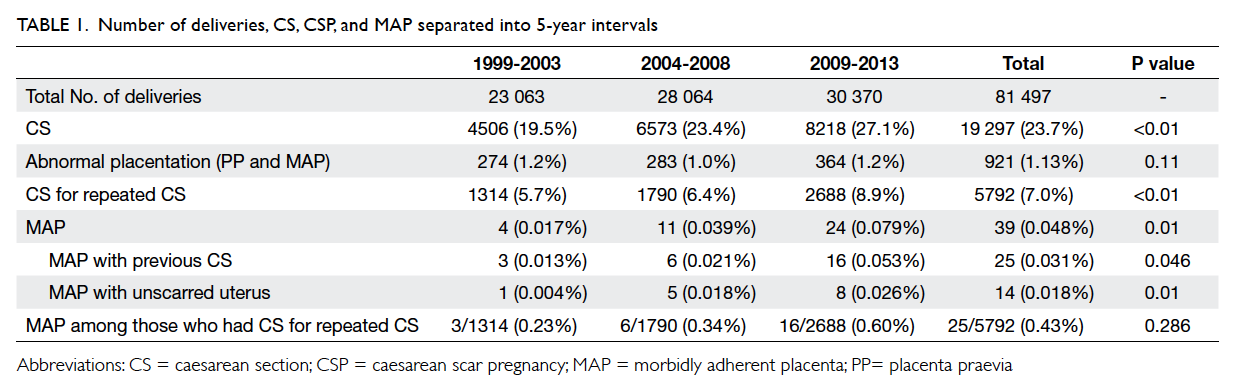
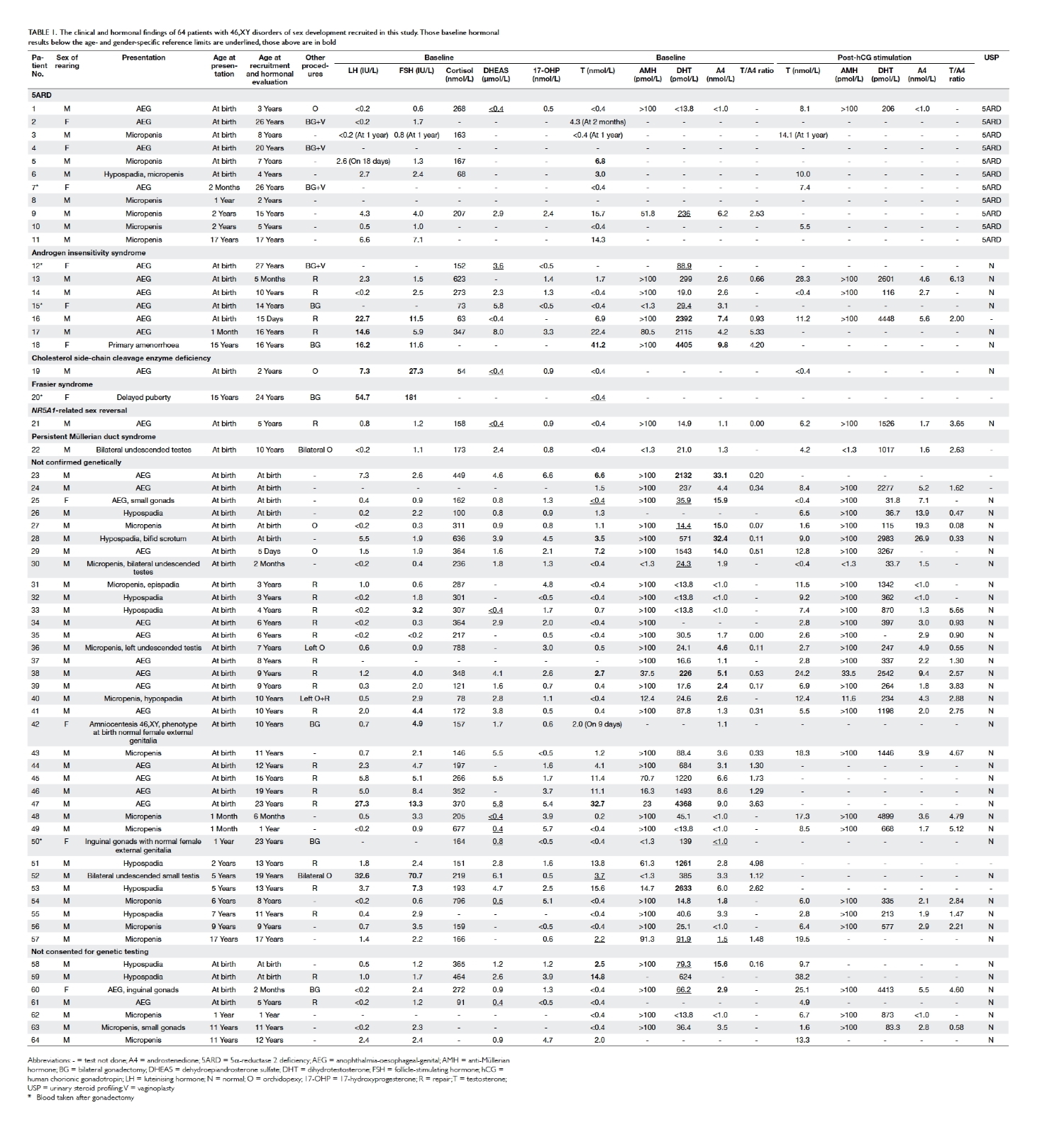
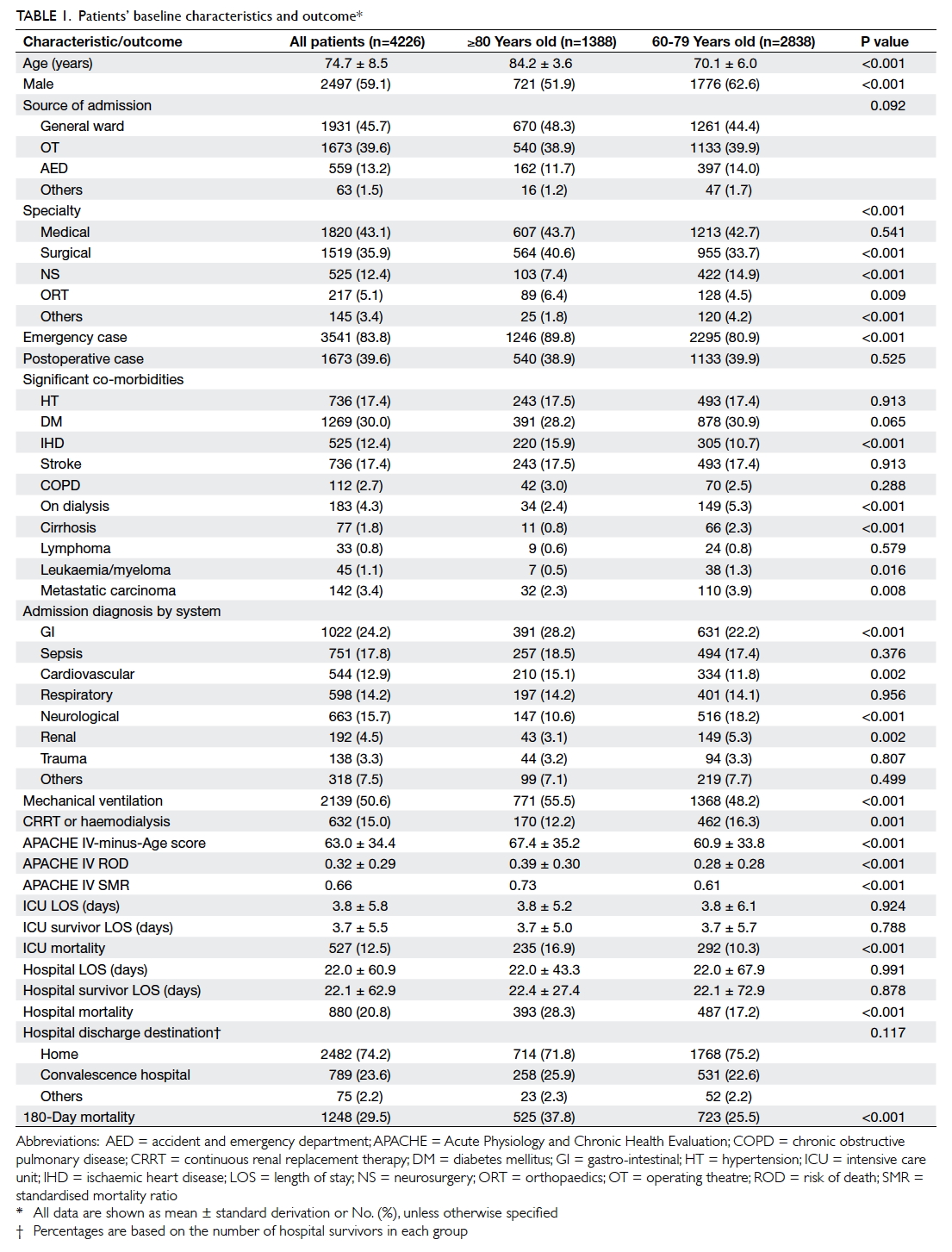
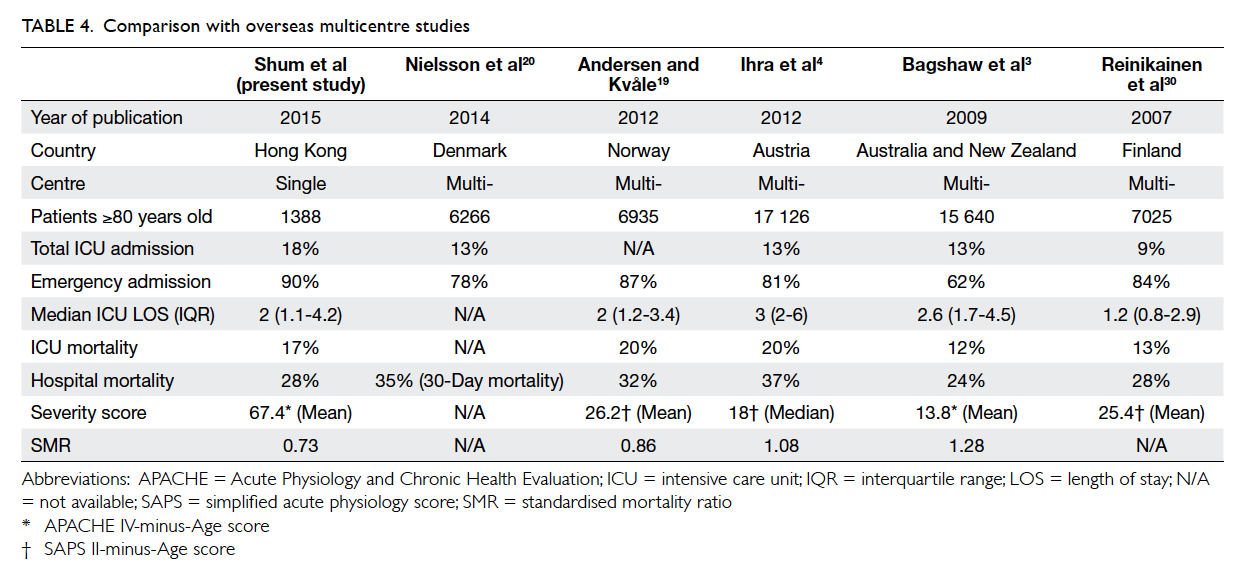
Between January 2008 and December 2011, 1507
DXA scans were performed for eligible women. Their
mean (± SD) age was 58.2 ± 6.4 years and the mean
age at menopause was 49.9 ± 4.0 years. The median
duration of menopause (years from menopause to
date of DXA) was 7 years (interquartile range, 3-11
years). The number of women with risk factors for
osteoporosis in the whole group and subgroups are
listed in Table 1. Only 1% of participants were unable
to recall whether or not there was a parental history
of osteoporosis or hip fracture.
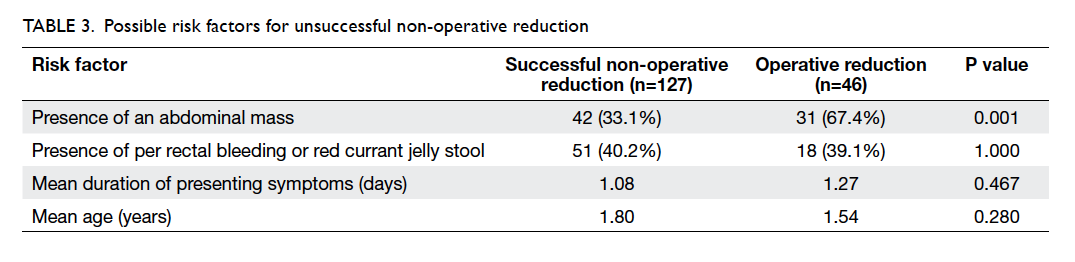
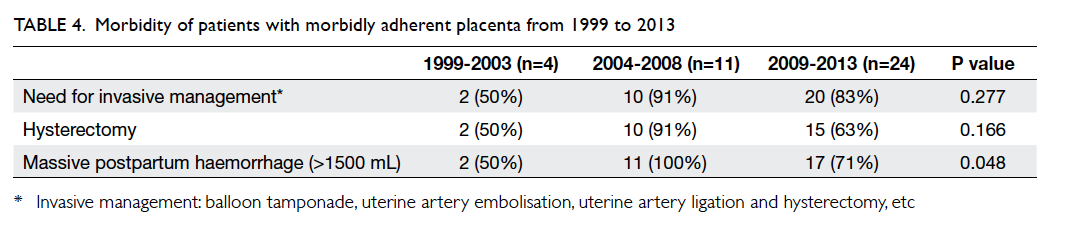
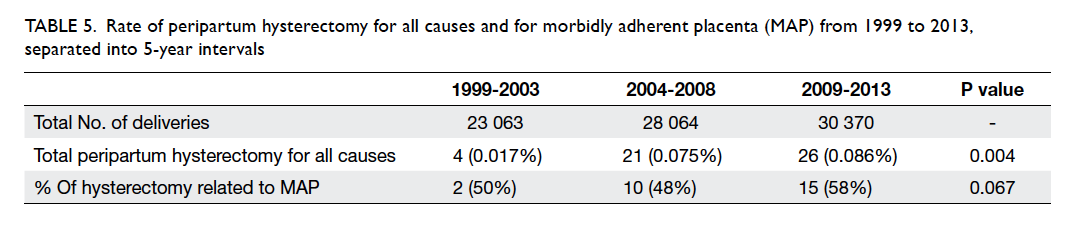
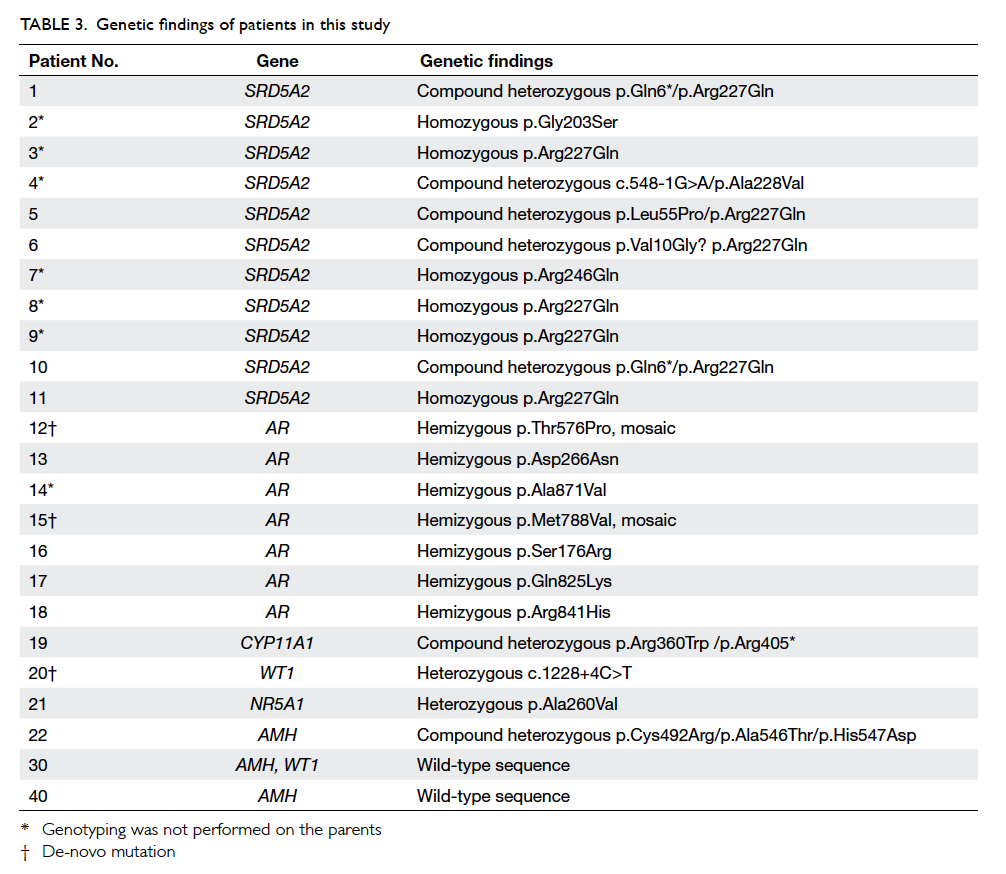
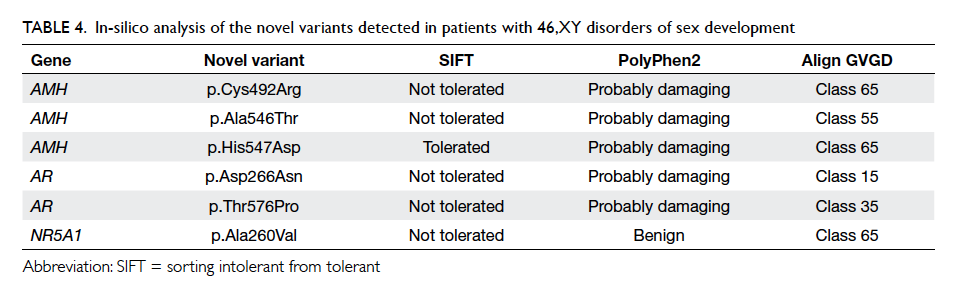
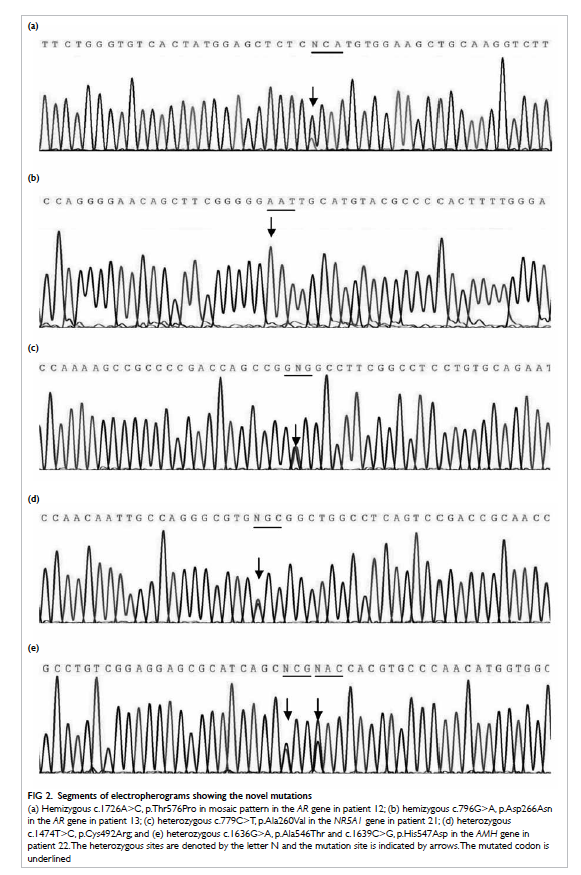
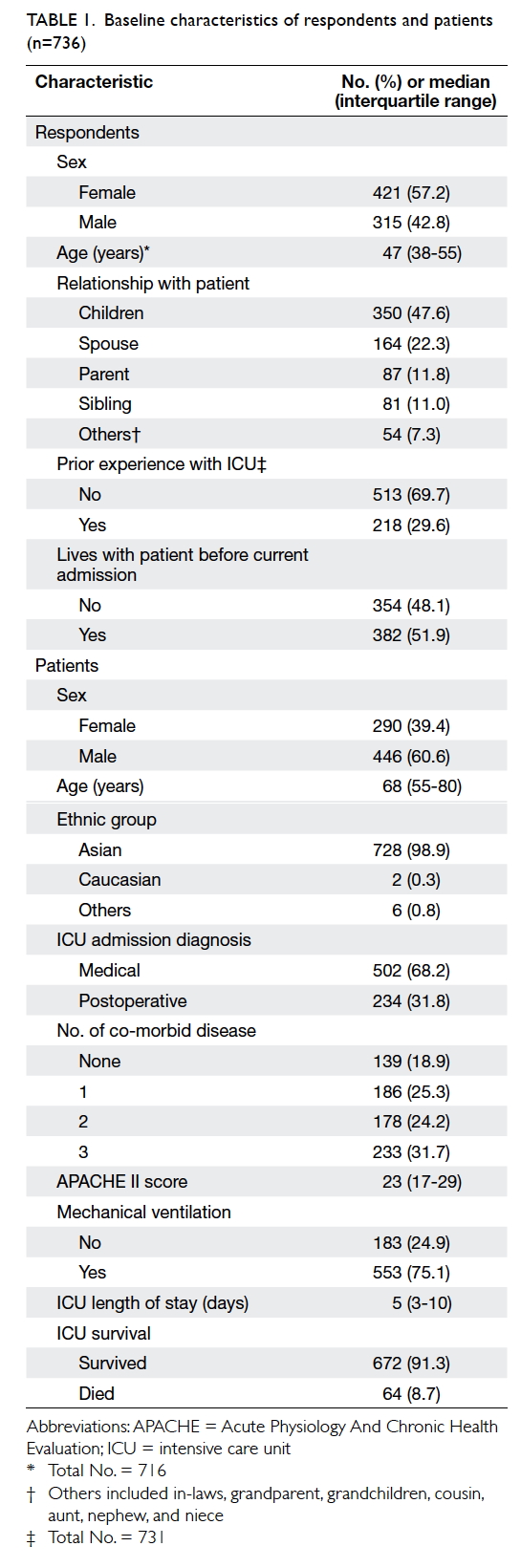
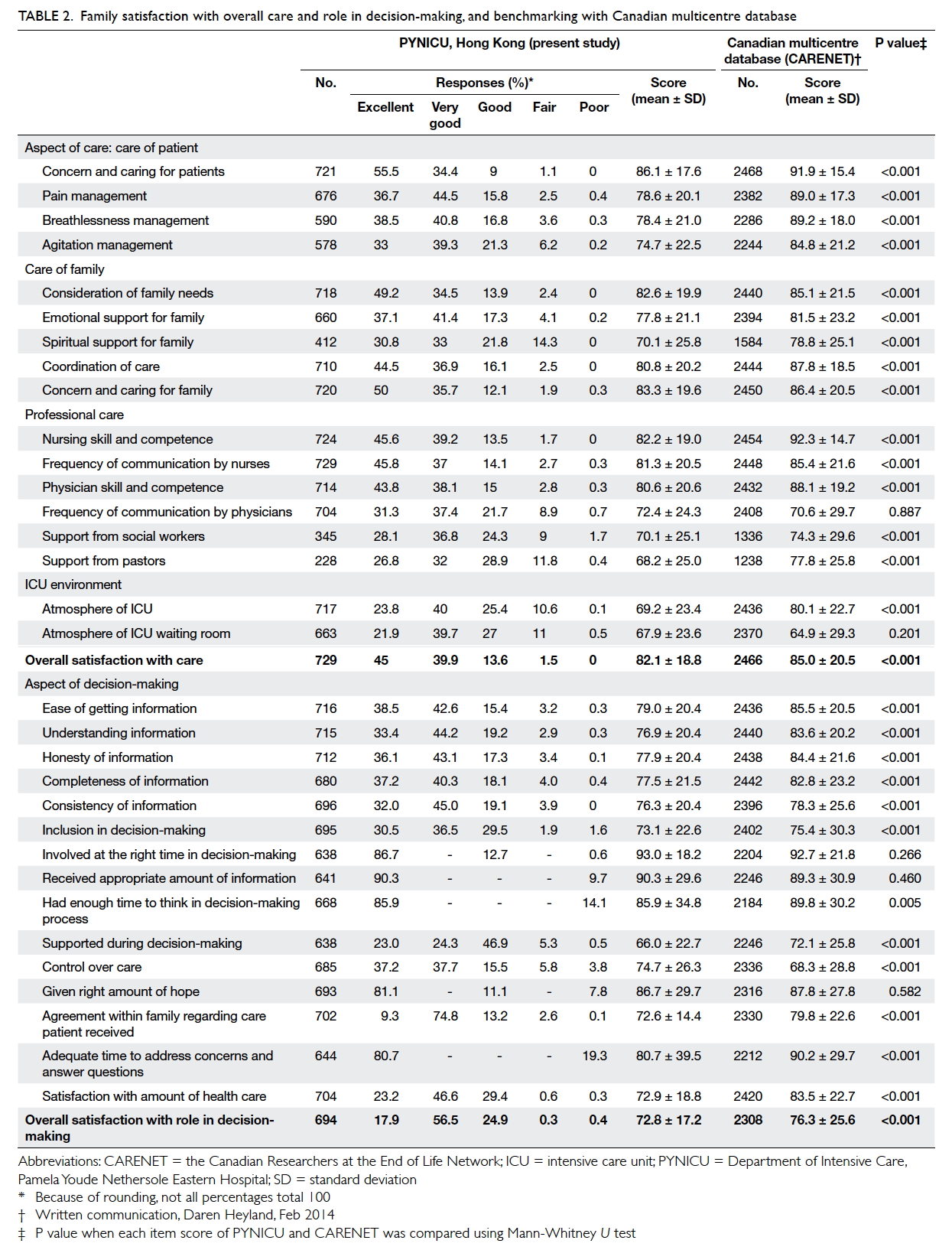
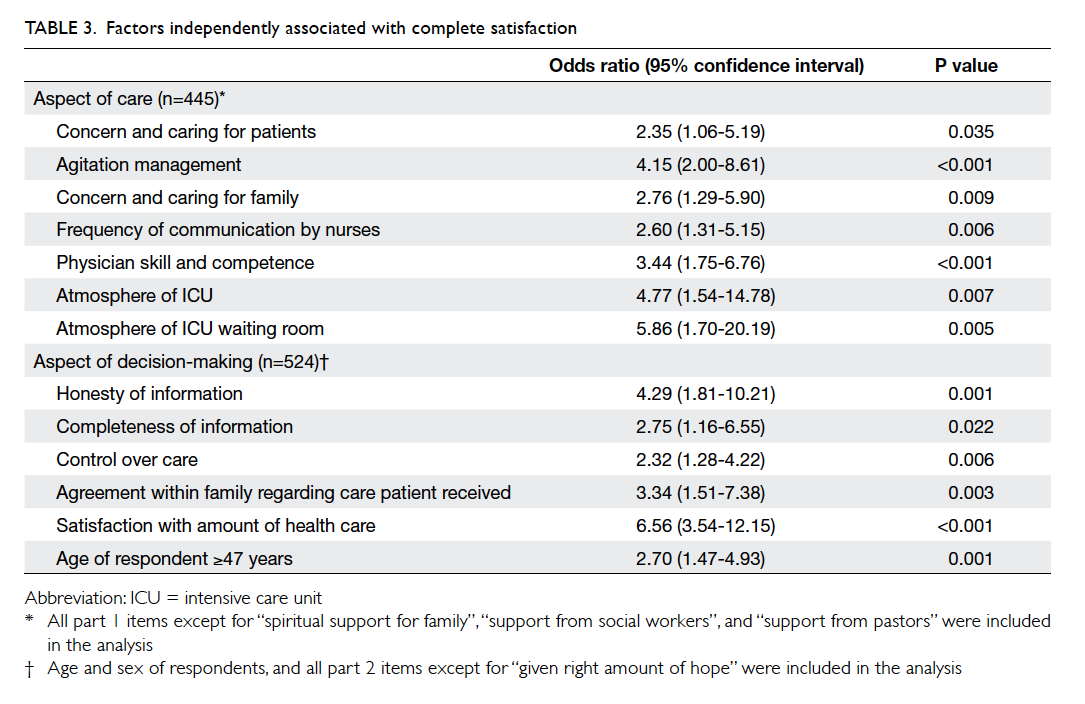
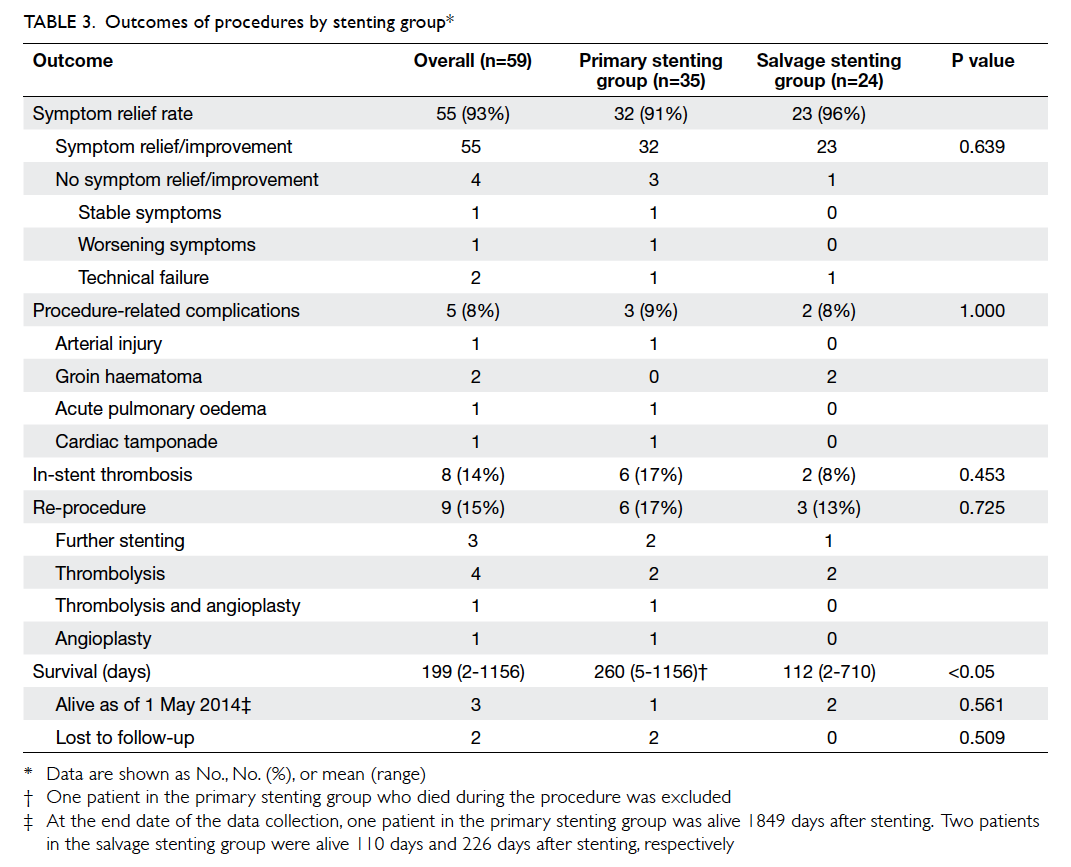
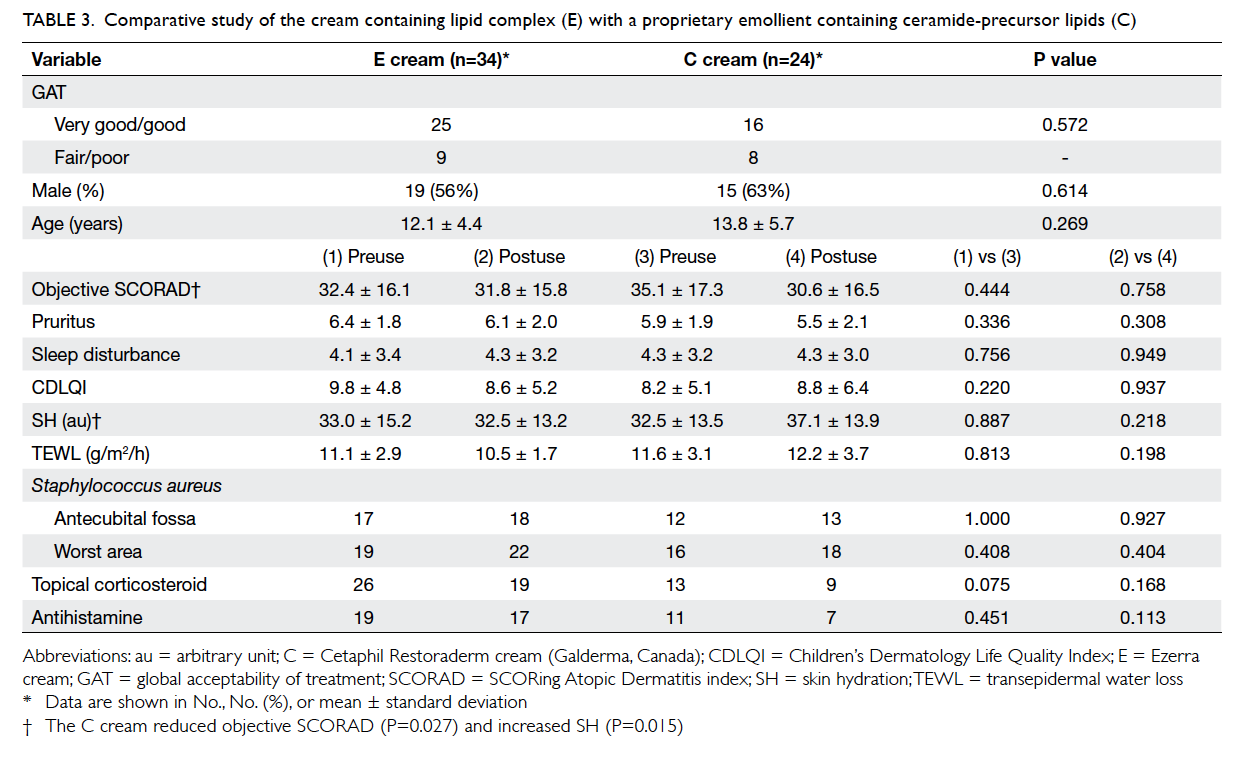
Osteoporosis was diagnosed in 25.7% of women
and osteopenia in 51.6%. The mean age of women
with normal BMD, osteopenia, and osteoporosis
was 57.0 ± 5.6 years, 58.0 ± 6.4 years, and 59.7 ±
6.8 years, respectively (P<0.001). The mean age at
menopause for each subgroup was the same: 50.0
years (P=0.441). Apart from age, BMI of <18.5 kg/m2
(P<0.001), duration of menopause (P<0.001),
parental history of osteoporosis or hip fracture
(P=0.024), and not doing 20 minutes of weight-bearing
exercise daily (P=0.033) were significant
risk factors for osteoporosis. Although smoking is a
significant risk factor for low bone mass, there were
too few smokers in this group to make any meaningful
comparison. The other risk factors did not show a
significant association with osteoporosis (Table 1).
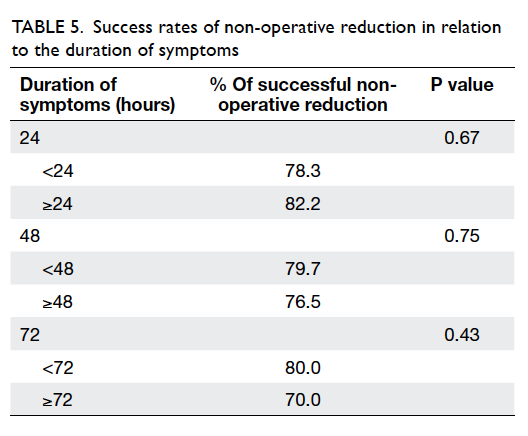
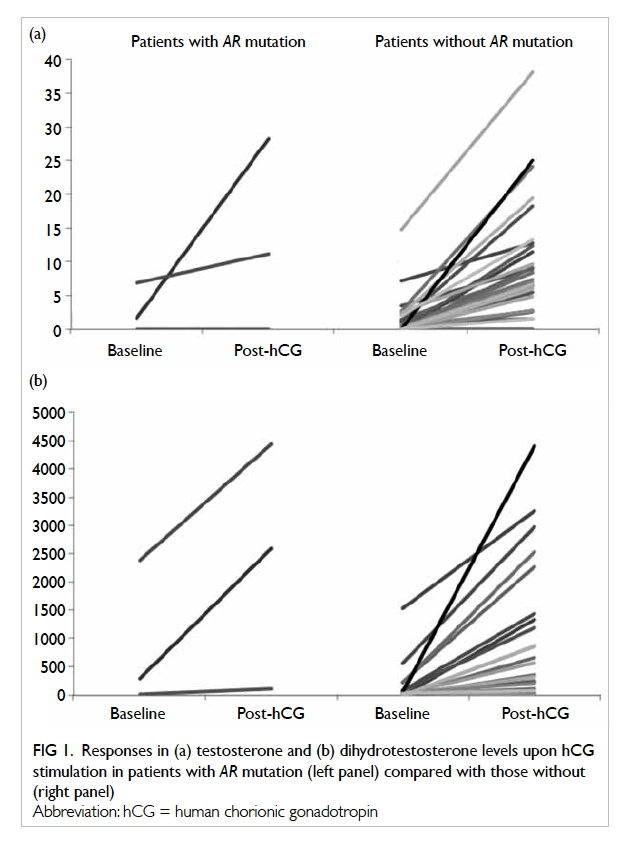
The proportion of women who had risk factors and
who had spine osteoporosis and hip osteoporosis is
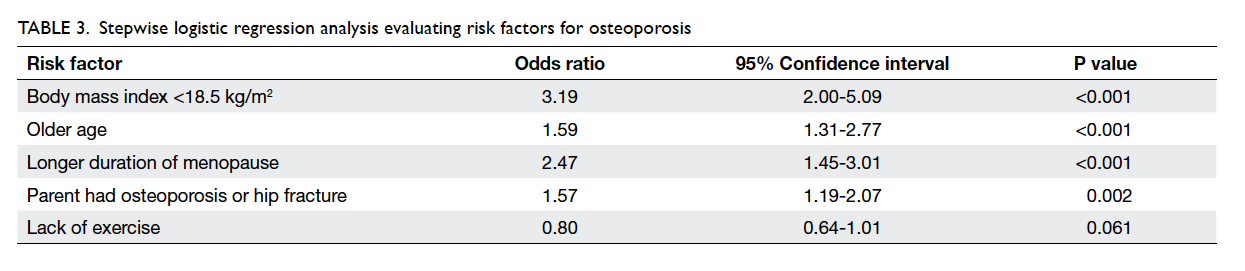
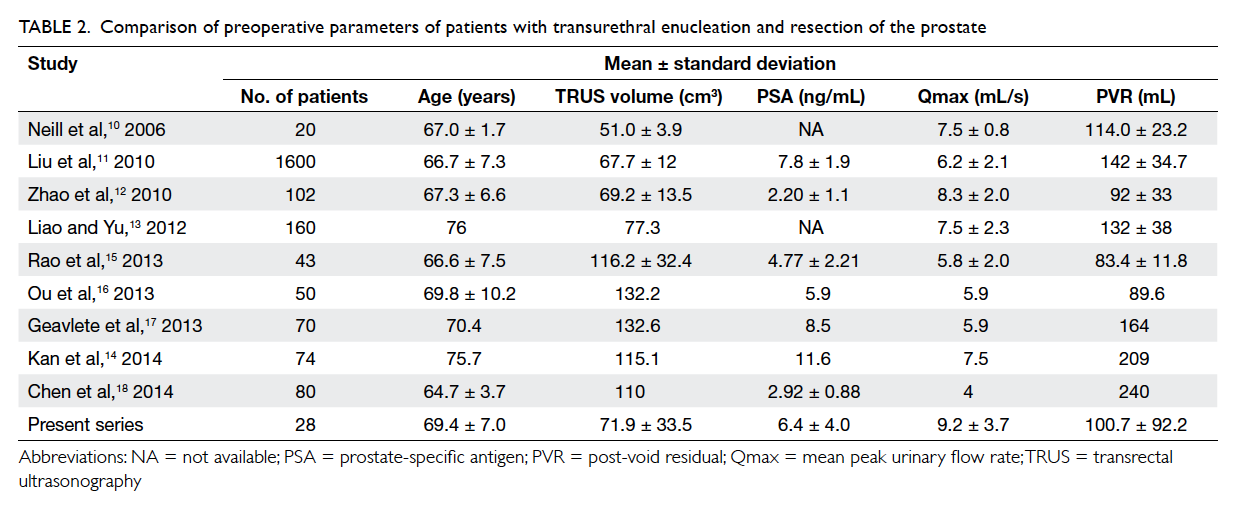
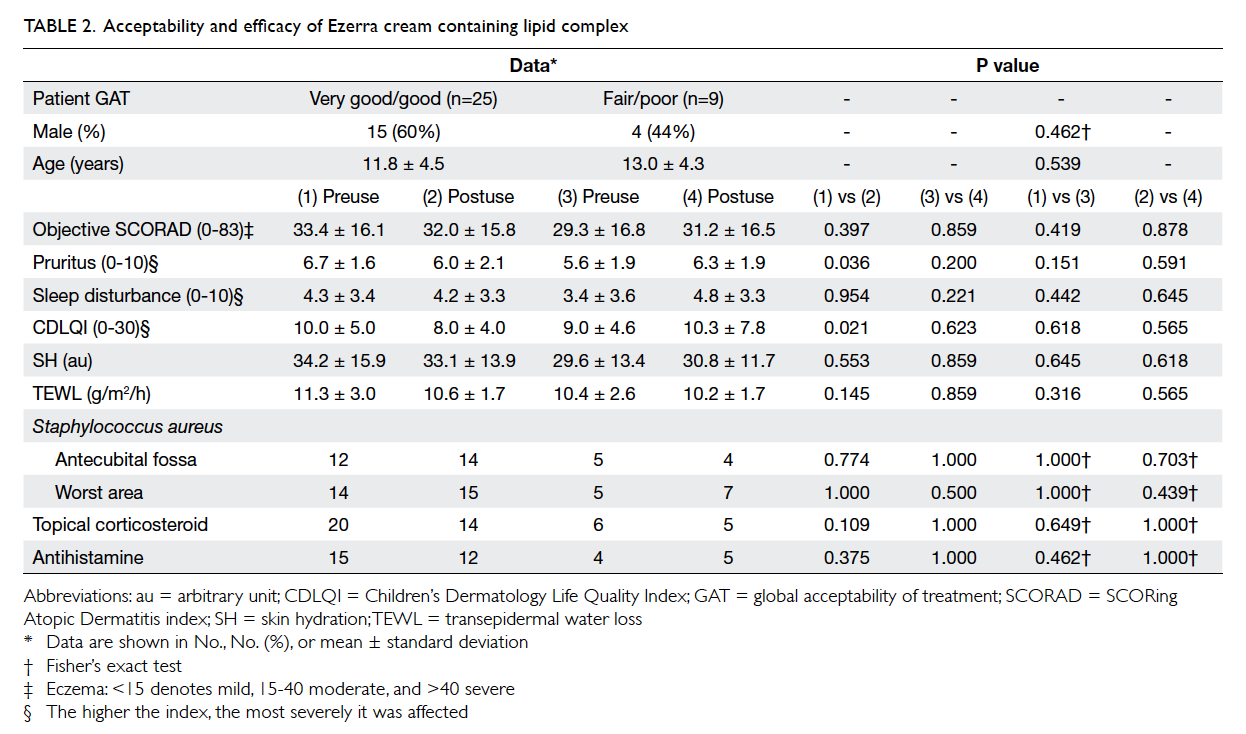
listed in Table 2. The results of the stepwise logistic
regression analysis are shown in Table 3—only older
age, low BMI, longer duration of menopause, and
parental history remained significant.
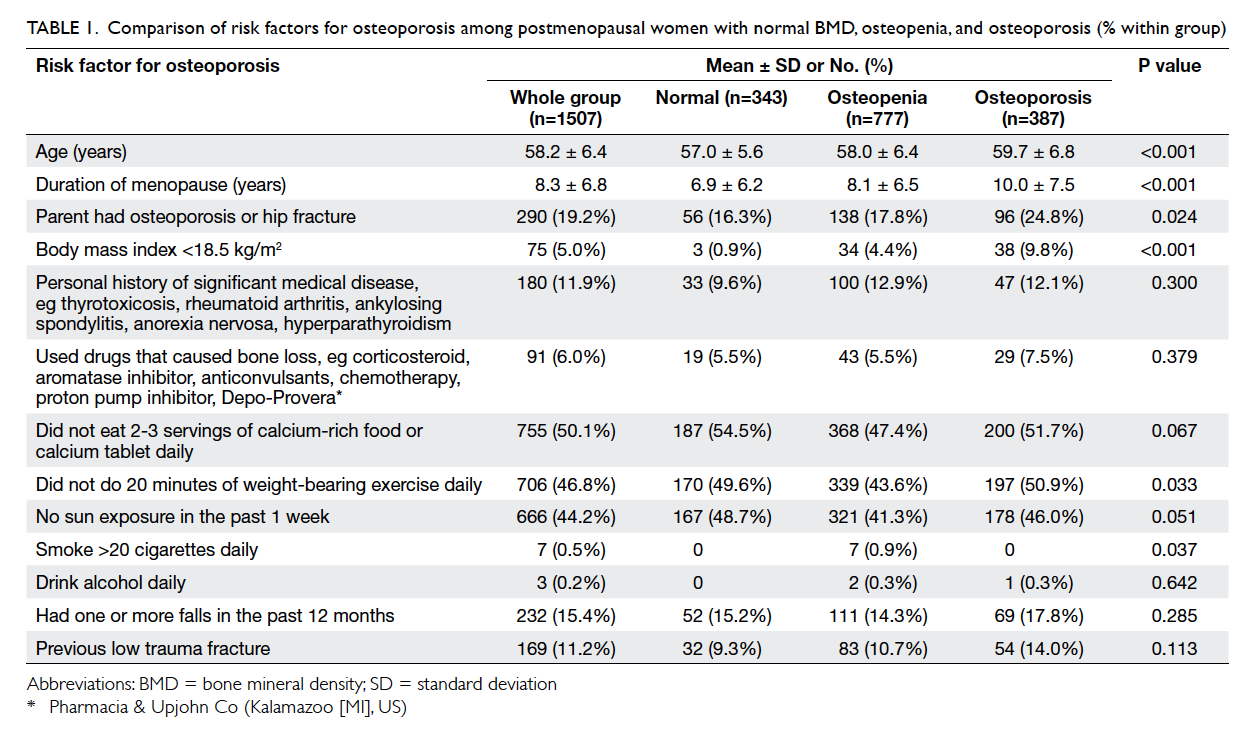
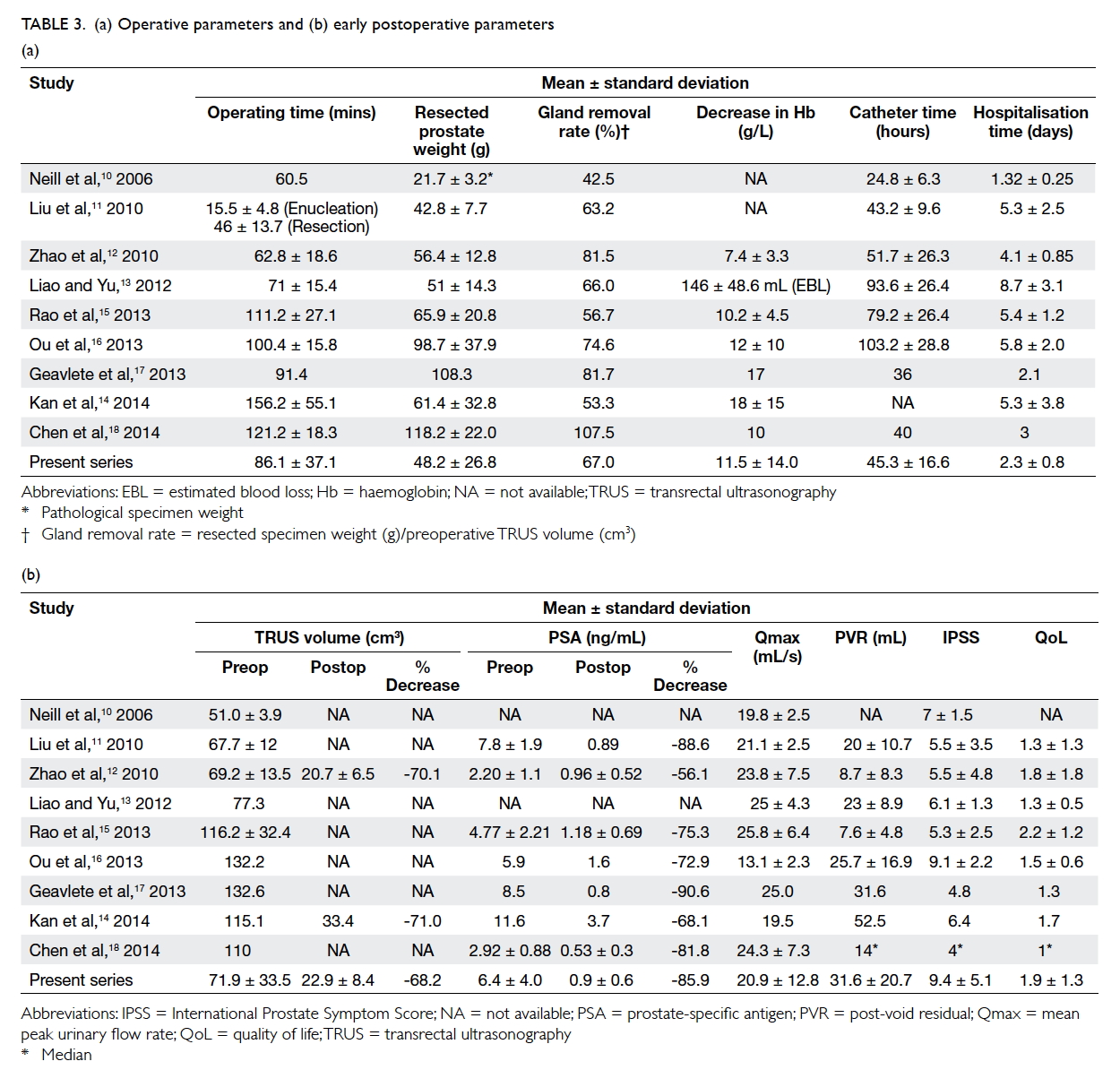
Table 1. Comparison of risk factors for osteoporosis among postmenopausal women with normal BMD, osteopenia, and osteoporosis (% within group)
Among the 387 women with osteoporosis, 166
(42.9%) refused treatment because they feared of
the side-effects of drugs, 119 (30.7%) complied with
the treatment provided, 45 (11.6%) discontinued
treatment due to side-effects or worry about side-effects,
and 57 (14.7%) has defaulted from follow-up by
March 2015. The common side-effects that concerned
patients included hot flushes with raloxifene, gastric
and musculoskeletal pain with bisphosphonates, and
loose stools and diarrhoea with strontium ranelate.
For major adverse events, patients were concerned
about atypical fracture and osteonecrosis of the jaw
with bisphosphonates and increased cardiac risk
with strontium ranelate. Among the 119 women who
complied with treatment, 20 were still on treatment
in March 2015 and 99 were taking a drug holiday
after 2 to 6 years’ treatment that brought BMD to the
osteopenic range. Those who refused treatment were
significantly older with a mean age of 61.2 ± 7.8 years
(P<0.001).
Discussion
Osteoporosis is estimated to affect 200 million
women worldwide, which is approximately one
tenth of women aged 60 years, one fifth of those
aged 70 years, two fifths of those aged 80 years, and
two thirds of women aged 90 years.14 It has been
estimated that approximately 30% of postmenopausal
American women15 and 23% of postmenopausal
Australian women have osteoporosis.16 The
prevalence of osteoporosis in postmenopausal
Indonesian women has been reported to be 20.2%
in the lumbar vertebrae.17 In Germany, 23.3% of
postmenopausal German women aged 50 to 64 years
had osteoporosis.18 The prevalence of osteoporosis
(25.7%) in this study was similar to the prevalence rate
of 24.9% reported by another local epidemiological
study.19 Because of the silent nature of osteoporosis,
most patients who do not undergo DXA are unaware
of the diagnosis. Realisation usually comes when a
fragility fracture occurs.
Screening DXA is recommended for women
aged 65 years and over as well as for at-risk younger
women.20 21 In our subjects, age, low BMI, positive parental history of osteoporosis or hip fracture, and
duration of menopause were significant risk factors.
The Osteoporosis Self-assessment Tool for Asians is a
simple validated tool that can determine the need for
DXA, based on age and body weight.22 Osteoporosis
has been shown by many studies to have a strong
genetic influence.23 24 25 A parental history of fracture,
particularly of the hip, confers an increased risk of
fracture that is independent of BMD.26 Most of our
patients could remember their menopause age and
provide a parental history of osteoporosis or hip
fracture for assessment.
Apart from delineating the magnitude of
osteoporosis among postmenopausal women, this
study also showed that almost half of them did
not have an adequate calcium intake, and did not
perform sufficient weight-bearing exercise or have
enough sun exposure. The National Osteoporosis
Foundation (NOF) recommends 1200 mg calcium
and 800 to 1000 IU vitamin D daily for women
aged 50 and beyond.21 Nearly all Asian countries
fall far below this recommendation. The median
dietary calcium intake for the adult Asian
population is approximately 450 mg/day.9 The recent
calcium calculator launched by the International
Osteoporosis Foundation (IOF) is a useful tool to
help women assess their daily calcium intake (http://www.iofbonehealth.org/calcium-calculator). Studies
carried out across different countries in South and
South-East Asia have shown, with few exceptions,
widespread prevalence of vitamin D deficiency and
insufficiency in both sexes and all age-groups of
the population.27 The IOF therefore recommends
800 IU/day vitamin D for everyone, even for those
with regular effective sun exposure.28 The NOF also
recommends regular weight-bearing and muscle-strengthening
exercise to improve agility, strength,
posture, and balance. This may reduce the risk of
falls and fractures.9 There is clear evidence that tai
chi is effective for fall prevention and improving
psychological health and is associated with general
health benefits for older people.29 Meta-analysis
of the effect of tai chi on osteoporosis or BMD is,
however, inconclusive as a result of many different
tai chi exercises being studied, and variable design
and different quality-rating instruments used in the
systematic reviews of tai chi literature.30 We were
unable to show a significant association of diet,
exercise, and sun exposure with osteoporosis in this
cohort, probably due to limitations in capturing
accurate information as discussed below. The
important message to emphasise is that, in this group
of self-selected clinic attendees who are in general
believed to be more health conscious, the proportion
of women adopting such healthy lifestyle strategies
was not high. The situation in the general population
might be worse. Since these are important lifestyle
strategies for osteoporosis prevention, clinicians
should encourage all postmenopausal women to
adopt them.
It is of concern that in this study almost 43%
of women with osteoporosis refused treatment.
Among those who agreed to start treatment, only
half adhered to treatment. Some women decided
to stop treatment prematurely because they were
distressed by reports of major adverse events
such as atypical fracture and osteonecrosis of the
jaw. Some women read news articles that stated
treatment should not exceed 2, 3, or 5 years, then
refused to continue treatment beyond this time
frame. Although bisphosphonates are long-acting
drugs, extended dosing does not compensate for
poor drug compliance. A recent study showed that
64.0% of patients discontinued weekly alendronate,
66.4% discontinued weekly risedronate, and 68.2%
discontinued monthly ibandronate.31 Hence dosing
regimens are unlikely to be solely responsible
for poor compliance. Other factors that reduced
drug compliance included: cost of medication,
low motivation to take drug as patients were
asymptomatic, patients did not believe they were
at significant risk of fracture, some patients had
difficulty complying with the prescribed regimen
for bisphosphonates and strontium ranelate in the
context of their daily routine, the patient was already
on a number of medications for other illnesses
and refused more. Further research is needed to
understand patient decision-making models for
osteoporosis treatment and how health education
from various sources (health-care providers, family,
friends, and media) can modify their attitude
towards osteoporosis treatment.
The main limitations of this study are, first,
selection bias because some women refused to
have DXA. The study women were therefore self-selected,
hence the prevalence reported might not
be representative of the population. Second, the
information in the checklist was provided by patient
recall and their responses were not verified. Similarly,
the menopause age was provided by the patient and
could not be verified. Third, the monitoring period
was insufficient to provide fracture data that would
allow comparison of outcome in patients who
adhered to treatment and those who did not. Fourth,
drug compliance (whether the drug was taken
correctly), drug omission, stockpiling or transfer of
medicines between friends and relatives were not
assessed in detail.
Conclusions
Osteoporosis is prevalent in the local population,
affecting one in four postmenopausal women. Those
with risk factors such as low BMI, older age, longer
duration since menopause, and parental history of
osteoporosis or hip fracture, should undergo DXA.
In addition to prompt diagnosis and treatment of
osteoporosis, physicians should monitor patient
drug compliance at each follow-up. At the same
time, calcium intake, sun exposure, and exercise
pattern should also be evaluated to help optimise
their bone health.
References
1. Recker RR, Lappe J, Davies K, Heaney R. Characterization
of perimenopausal bone loss: a prospective study. J Bone
Miner Res 2000;15:1965-73. Crossref
2. Pouillès JM, Trémollières F, Ribot C. Vertebral bone loss in
perimenopause. Results of a 7-year longitudinal study [in
French]. Presse Med 1996;25:277-80.
3. Assessment of fracture risk and its application to screening
for postmenopausal osteoporosis. WHO Technical Report
Series 843. Geneva: World Health Organization; 1994.
4. Marshall D, Johnell O, Wedel H. Meta-analysis of how well
measures of bone mineral density predict occurrence of
osteoporotic fractures. BMJ 1996;312:1254-9. Crossref
5. Kung AW, Lee KK, Ho AY, Tang G, Luk KD. Ten-year risk of
osteoporotic fractures in postmenopausal Chinese women
according to clinical risk factors and BMD T-scores: a
prospective study. J Bone Miner Res 2007;22:1080-7. Crossref
6. Lau EM, Cooper C. The epidemiology of osteoporosis. The
oriental perspective in a world context. Clin Orthop Relat
Res 1996;323:65-74. Crossref
7. Lau EM, Cooper C, Fung H, Lam D, Tsang KK. Hip fracture
in Hong Kong over the last decade—a comparison with the
UK. J Public Health Med 1999;21:249-50. Crossref
8. Kung AW, Yates S, Wong V. Changing epidemiology
of osteoporotic hip fracture rates in Hong Kong. Arch
Osteoporos 2007;2:53-8. Crossref
9. The Asian Audit. Epidemiology, costs and burden of
osteoporosis in Asia 2009. International Osteoporosis
Foundation; 2009. Available from: http://www.iofbonehealth.org/sites/default/files/PDFs/Audit%20Asia/Asian_regional_audit_2009.pdf. Accessed 26 Jan 2015.
10. Lau EM, Chan HH, Woo J, et al. Normal ranges for vertebral
height ratios and prevalence of vertebral fracture in Hong
Kong Chinese: a comparison with American Caucasians. J
Bone Miner Res 1996;11:1364-8. Crossref
11. Center JR, Bliuc D, Nguyen TV, Eisman JA. Risk of
subsequent fracture after low-trauma fracture in men and
women. JAMA 2007;297:387-94. Crossref
12. International Osteoporosis Foundation. The Breaking
Spine. 2010. Available from: http://share.iofbonehealth.org/WOD/2010/thematic_report/2010_the_breaking_spine_en.pdf. Accessed 22 May 2015.
13. Cramer JA, Gold DT, Silverman SL, Lewiecki EM. A
systematic review of persistence and compliance with
bisphosphonates for osteoporosis. Osteoporos Int
2007;18:1023-31. Crossref
14. Kanis JA. Assessment of osteoporosis at the primary health
care level. Report of a WHO Scientific Group. Technical
Report. World Health Organization Collaborating Centre
for Metabolic Bone Diseases, University of Sheffield, UK;
2007. Available from: http://www.iofbonehealth.org/sites/default/files/WHO_Technical_Report-2007.pdf. Accessed
22 May 2015.
15. Melton LJ 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs
BL. Perspective: How many women have osteoporosis? J
Bone Miner Res 1992;7:1005-10. Crossref
16. Estimating the prevalence of osteoporosis in Australia. Cat.
no. PHE 178. Canberra: Australian Institute of Health and
Welfare (AIHW); 2014. Available from: http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129548481.
Accessed 22 May 2015.
17. Meiyanti. Epidemiology of osteoporosis in postmenopausal
women aged 47 to 60 years. Univ Med 2010;29:169-76.
Available from: http://www.univmed.org/wp-content/uploads/2011/02/Meiyanti.pdf. Accessed 22 May 2015.
18. Häussler B, Gothe H, Göl D, Glaeske G, Pientka L,
Felsenberg D. Epidemiology, treatment and costs
of osteoporosis in Germany—the BoneEVA Study.
Osteoporos Int 2006;18:77-84. Crossref
19. Lau EM, Chung HL, Ha PC, Tam H, Lam D. Bone mineral
density, anthropometric indices, and the prevalence of
osteoporosis in Northern (Beijing) Chinese and Southern
(Hong Kong) Chinese women—the largest comparative study
to date. J Clin Densitom 2015 Jan 13. Epub ahead of print. Crossref
20. 2013 Official Positions of the International Society for
Clinical Densitometry. Available from: http://www.iscd.org/documents/2014/02/2013-iscd-official-position-brochure.pdf. Accessed 26 Jan 2015.
21. National Osteoporosis Foundation. The clinician’s guide to
prevention and treatment of osteoporosis 2014. Available
from: http://nof.org/files/nof/public/content/file/2791/upload/919.pdf. Accessed 26 Jan 2015.
22. Koh LK, Sedrine WB, Torralba TP, et al. A simple tool to
identify Asian women at increased risk of osteoporosis.
Osteoporos Int 2001;12:699-705. Crossref
23. Pocock NA, Eisman JA, Hopper JL, Yeates MG, Sambrook
PN, Eberl S. Genetic determinants of bone mass in adults.
A twin study. J Clin Invest 1987;80:706-10. Crossref
24. Seeman E, Hopper JL, Bach LA, et al. Reduced bone mass
in daughters of women with osteoporosis. N Engl J Med
1989;320:554-8. Crossref
25. Thijssen JH. Gene polymorphisms involved in the regulation
of bone quality. Gynecol Endocrinol 2006;22:131-9. Crossref
26. Kanis JA, Johansson H, Oden A, et al. A family history
of fracture and fracture risk: a meta-analysis. Bone
2004;35:1029-37. Crossref
27. Mithal A, Wahl DA, Bonjour JP, et al. Global vitamin D
status and determinants of hypovitaminosis D. Osteoporos
Int 2009;20:1807-20. Crossref
28. Dawson-Hughes B, Mithal A, Bonjour JP, et al. IOF position
statement: vitamin D recommendations for older adults.
Osteoporos Int 2010;21:1151-4. Crossref
29. Lee MS, Ernst E. Systematic reviews of t’ai chi: an overview.
Br J Sports Med 2012;10:713-8. Crossref
30. Alperson SY, Berger VW. Opposing systematic reviews:
the effects of two quality rating instruments on
evidence regarding t’ai chi and bone mineral density in
postmenopausal women. J Altern Complement Med
2011;17:389-95. Crossref
31. Fan T, Zhang Q, Sen SS. Persistence with weekly and
monthly bisphosphonates among postmenopausal women:
analysis of a US pharmacy claims administrative database.
Clinicoecon Outcomes Res 2013;5:589-95. Crossref