Hong Kong Med J 2015 Jun;21(3):208–16 | Epub 9 Apr 2015
DOI: 10.12809/hkmj144304
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Effectiveness of a discharge planning and community support programme in preventing readmission of high-risk older patients
Francis OY Lin, MB, BS, MRCP (UK);
James KH Luk, FHKCP, FHKAM (Medicine);
TC Chan, FHKCP, FHKAM (Medicine);
Winnie WY Mok, FHKCP, FHKAM (Medicine);
Felix HW Chan, FHKCP, FHKAM (Medicine)
Department of Medicine and Geriatrics, TWGHs Fung Yiu King Hospital, 9 Sandy Bay Road, Pokfulam, Hong Kong
Corresponding author: Dr James KH Luk (lukkh@ha.org.hk)
Abstract
Objective: To examine the effectiveness of Integrated
Care and Discharge Support for elderly patients
in reducing accident and emergency department
attendance, acute hospital admissions, and hospital
bed days after discharge. Factors that compromise
its effectiveness were investigated and cost analysis
was performed.
Design: Cohort prospective study.
Setting: Integrated Care and Discharge Support for elderly patients in Hong Kong West Cluster.
Participants: Home-dwelling patients recruited between April 2012 and March 2013 into Integrated Care and Discharge Support for elderly patients in Hong Kong West Cluster.
Results: A total of 1090 older patients were studied.
The Integrated Care and Discharge Support for
elderly patients programme reduced accident and emergency department attendance
by 40% (P<0.001), acute hospital admissions by
47% (P<0.001), and hospital bed days by 31%
(P<0.001) at 6 months after implementation. Improvements in Barthel Index 20
(P<0.001) and Modified Functional Ambulation
Category scale (P<0.001) were observed. Of the patients,
85 (7.8%) died within 6 months of initiation of the
programme. Only 26 (2.4%) older patients required
institutionalisation in residential care homes
within 6 months after the programme. Increasing
age (P=0.025) and high Charlson Comorbidity
Index score (P=0.001) were positive predictors for
accident and emergency department attendance.
A high albumin level (P=0.001) and living alone
(P=0.033) were negative predictors for accident and
emergency department attendance. Of the patients,
310 (28.4%) had no reduction in bed days after the
programme. Increasing age (P=0.025) and number of
medications (P=0.003) were positive predictors for
no reduction in bed days; while higher haemoglobin
level (P=0.034) was a negative predictor. There was
a potential annual cost-saving of HK$22.5 million (approximately US$2.9 million).
Conclusion: The Integrated Care and Discharge
Support for elderly patients programme reduced
accident and emergency department attendance,
acute hospital admissions and hospital bed days,
and was potentially cost-saving. Age, Charlson
Comorbidity Index, albumin level, and living
alone were factors associated with accident and
emergency department attendance. Age, number of
medications, and haemoglobin level were associated
with no reduction in bed days. Further study of the
cost-effectiveness of such programme is warranted.
New knowledge added by this
study
- Integrated Care and Discharge Support for elderly patients (ICDS) reduced accident and emergency department (AED) attendances, acute hospital admissions, and hospital bed days.
- ICDS service was potentially cost-saving and might minimise institutionalisation.
- Age, Charlson Comorbidity Index, albumin level, and living alone were associated with AED attendance.
- Age, number of medications, and haemoglobin levels were associated with no reduction in bed days.
- ICDS programme should be continued in Hong Kong to face the challenges of an increasing older population.
- Further studies are suggested to examine whether AED attendance, acute hospital admissions, and hospital bed days among high-risk older patients can be further reduced by modifying some of the predictive factors identified in this study.
- A more detailed auditing is warranted to show its value in reducing health care costs.
Introduction
‘Revolving door syndrome’ was a phrase coined
by Gordon1 in 1995 to describe the problem of
recurrent return of older people to hospital shortly
after discharge. Readmission is common among
medical patients, especially the elderly population,
and is a poor outcome for the health care system.2 3 A retrospective analysis in 2007 showed the overall
30-day unplanned readmission rate of medical patients was 16.7%.4 A study in Hong Kong West Cluster (HKWC) showed the 28-day readmission
rate for elderly patients discharged from a geriatric
convalescent hospital to be 21.6%.5
To date, different programmes and strategies
have been described to reduce hospital readmission.
These include comprehensive geriatric assessment,
discharge planning, adopting a case manager
approach, post-discharge support services, early
intervention for ad-hoc medical problems, and use of
telephone nursing services.6 7 8 9 10 11 It has been advocated
that in order to achieve better efficacy, any programme
that aims to prevent hospital readmission should
focus on patients at high risk.12 In Hong Kong, the
Hospital Authority (HA) has developed a validated
prediction model named “Hospital Admission Risk
Reduction Program for the Elderly” (HARRPE) to
identify older people at high risk of readmissions.13
The HARRPE score comprises 14 predictors that
are categorised into socio-demographic data, prior
utilisation of accident and emergency department
(AED) and medical ward admission in the past 1
year, co-morbidity, and current index admission. The
higher the HARRPE score (ranges from 0 to 1), the
higher the readmission risk.
In Hong Kong, a pilot Integrated Discharge
Support Program for Elderly Patients (IDSP) was
launched in three hospitals, namely the United
Christian Hospital in 2008, Princess Margaret
Hospital in 2008, and Tuen Mun Hospital in 2009.
The programme targeted patients aged ≥60 years
admitted to these hospitals with a HARRPE score of
≥0.2. It aimed to reduce the risk of AED attendance
and hospital readmission through better discharge
planning and post-discharge support. Preliminary
results showed it successfully reduced AED
attendance, emergency admission, and hospital bed
days.14
In view of the positive results of IDSP and
based on the recommendation of the Elderly
Commission, the Financial Secretary of the Hong
Kong SAR announced in the 2011/2012 budgets that
the Government would allocate additional recurrent
funding to make it a regular service to all districts.
In addition, a new case management approach,
Integrated Care Model (ICM), was added. Such new
programme has been renamed Integrated Care and
Discharge Support for elderly patients (ICDS).
Integrated Care and Discharge Support for
elderly patients in Hong Kong West Cluster
In January 2012, HKWC launched the ICDS and
involves hospital and community components (Fig).
For the hospital component, risk stratification,
comprehensive geriatric assessment, and discharge
planning are performed. Link nurses (who serve
as ‘link’ between in-patients and community
services) work with geriatricians to perform multidimensional
assessments for home-dwelling older
patients aged ≥60 years admitted to medical wards
with HARRPE score of ≥0.2. They also assess elderly
patients by proactive screening. In addition, patients
can be referred to link nurses using a standardised
clinical referral form. The form can be completed
by any member of the clinical team, including
doctors, nurses, pharmacists, and any allied health care
professional. The criteria for clinical referral include
items such as frequent readmission, poor social
support, inadequate care at home, deterioration
in memory, drug compliance problems, repeated
falls, mobility, and functional impairment. Referrers
can also comment about any problem not listed
in the referral form. In HKWC, case recruitment
and discharge planning take place in the medical
wards of the acute hospital, Queen Mary Hospital
(QMH), and three convalescent hospitals, namely
the Fung Yiu King Hospital (FYKH), Grantham
Hospital (GH), and Tung Wah Hospital (TWH).
After assessment, link nurses will, according to need,
allocate patients to either ICM Case Management or
Home Support Team (HST) services (see below). In
order to enhance the care of high-risk older patients
in QMH, a Comprehensive Care Program for the Elderly
(CCPE) area has been established. There are 12 beds
designated as CCPE (6 male and 6 female beds) in
paired wards of QMH. Case recruitment for CCPE
is mainly from the AED. Patients in CCPE are under
the care of the regular medical team with proactive
ICDS multidisciplinary input including geriatric
assessment and discharge planning for appropriate
community support services.
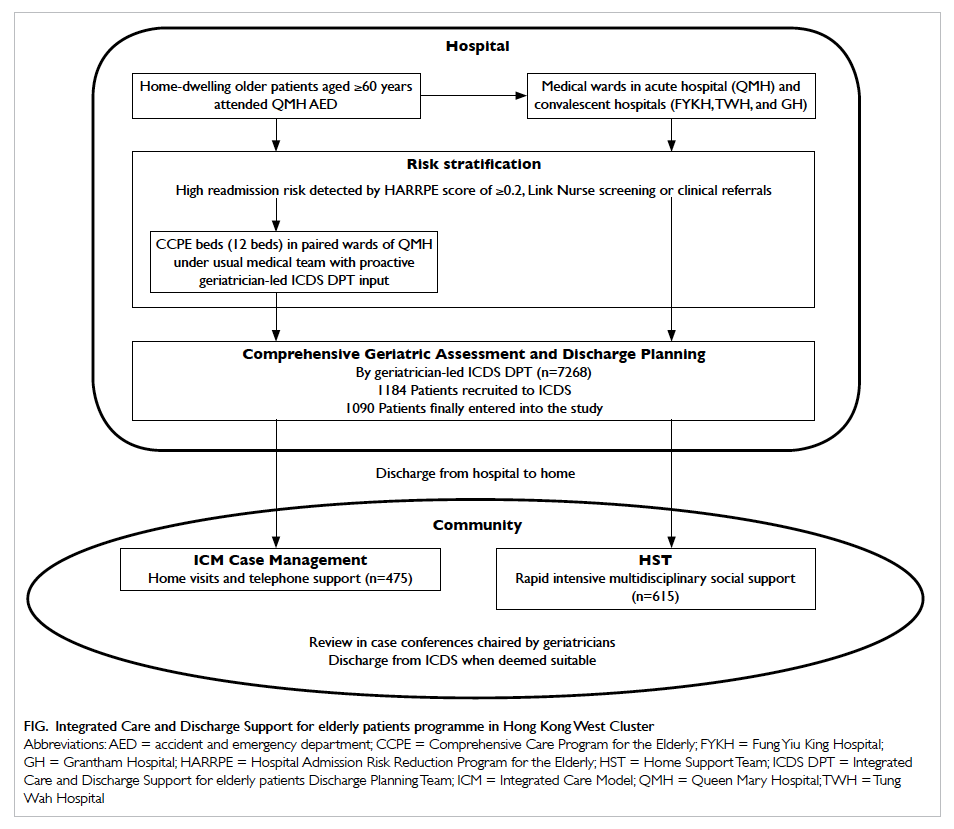
Figure. Integrated Care and Discharge Support for elderly patients programme in Hong Kong West Cluster
In the community component, there are
two important streams, namely the ICM Case
Management and HST service. In ICM Case
Management, each high-risk older patient is
followed up by a case manager for a period of around
3 months following hospital discharge. In HKWC, in
terms of full-time equivalence, two social workers,
one physiotherapist (PT), one occupational therapist
(OT), and half a nurse (advanced practice nurse) take
turns to be a case manager. Case managers provide
post-discharge support to older patients by home
visits and telephone support. They are responsible
for community service coordination and ensuring
patient compliance with planned services and
management. The second stream is the HST service
and is the responsibility of a non-governmental
organisation (NGO) partner. In HKWC, the NGO partner is Aberdeen Kai-fong Association (香港仔坊會). This HST includes nurses, PT, OT, and other allied
health members. They provide rapid and intensive
community support for discharged patients, offering
services such as meal delivery, household cleaning,
respite care, and home assessment and modification.
Case selection and allocation to ICM Case
Management or HST is performed by link nurses
under the supervision of an ICM geriatrician.
Link nurses apply standardised selection criteria
for case allocation. In general, patients with more
complex medical and social problems who require
multidisciplinary intervention by nurses, PT, and/or OT will be allocated to ICM Case Management.
Those who require urgent social services are recruited
into HST. Link nurses, ICM case managers, and the
HST hold weekly multidisciplinary case conferences
chaired by an ICM geriatrician. If needed, referral
for rehabilitation in a geriatric day hospital, fast
track clinic, or early specialist clinic follow-up can
be offered to patients.
Knowledge gaps
The ICDS programme that started in HKWC in 2012
is unprecedented and deserves a large-scale study to
demonstrate its efficacy. Although the aim of ICDS
is not to reduce costs, its value and sustainability can
nonetheless be better justified if this can be achieved.
The objectives of this prospective cohort study
were to investigate whether the ICDS can reduce AED
attendance, acute hospital admissions, and hospital
bed days (acute and convalescence), and to identify
the independent factors that predict its efficacy. In
addition, we wished to determine whether there is
potential for ICDS to reduce health care costs.
Methods
Design and setting
This was a prospective cohort study performed in
four hospitals of HKWC, namely the QMH, FYKH,
GH, and TWH. The study protocol was approved by
the Institutional Review Boards of the University of
Hong Kong and HA HKWC.
Subjects
Our subjects were home-dwelling older patients aged
≥60 years admitted to the general medical wards of
QMH and were recruited into the ICDS programme
by link nurses from 1 April 2012 to 30 March 2013.
Patients were excluded from the analysis if they
died, entered residential care homes for the elderly
(RCHEs), moved out of the cluster, or refused ICDS
services before their first home visit.
Variables
Baseline data included demography, HARRPE score
(if available), mode of feeding, continence status,
presence of pressure sores, and use of an indwelling
urinary catheter, nasogastric tube, or long-term
oxygen. The chief problems at index admission of
ICDS recruitment were noted. In addition, data on
co-morbidities, number of medications, and baseline
blood tests including haemoglobin, albumin, and
creatinine levels were retrieved from the HA
Clinical Management System (CMS). The Charlson
Comorbidity Index (CCI) was used to quantify the
burden of co-morbid diseases,15 and quantified
according to International Classification of Diseases
(ICD) coding in CMS.
Cognitive status was assessed on entry to and
discharge from the ICDS programme using the
Abbreviated Mental Test (AMT).16 The patients’
Modified Functional Ambulation Category scale
(MFAC) and Barthel Index 20 (BI-20) status
were also recorded.17 The mortality rate and
institutionalisation rate of patients within 6 months
of intake were calculated.
Outcome measurement
We compared the number of AED attendances,
unplanned acute hospital admissions, and length of
stay (LOS) in both acute and convalescent hospitals
6 months before and 6 months after recruitment.
The index AED attendance and hospital admissions
were counted as pre–6-month outcome. Any
subsequent AED attendance and hospital admission
was included in the post–6-month data. Two
specific outcomes were identified, namely any
AED attendance 6 months after ICDS recruitment,
and no reduction in hospital bed days (acute and
convalescence) 6 months after ICDS. The potential
cost-saving of ICDS was calculated using the existing
cost of AED attendances as well as bed day cost in
acute and convalescent hospitals in HKWC.
Statistical analyses
The Statistical Package for the Social Sciences
(Windows version 18.0; SPSS Inc, Chicago [IL],
US) was used in statistical analysis. Continuous
variables were expressed as mean ± standard
deviation. Independent t test was used to compare
continuous variables of two different groups. Paired
t test was used to compare the continuous variables
within groups. Mann-Whitney test and Wilcoxon
signed rank test were used when the continuous
variables could not be assumed to be in normal
distribution. Chi squared test and Fisher’s exact test
were employed to compare categorical variables.
The association between different variables with
any AED attendance and no reduction in bed days
was calculated using univariate logistic regression.
The variables were gender, programmes entered, use
of home oxygen, use of tube feeding, use of a Foley
catheter, presence of wound, BI-20, AMT, MFAC,
CCI, haemoglobin level, albumin level, creatinine
level, and number of medications. Significant factors
detected during univariate analysis were put into
multivariate stepwise backward logistic regression.
Statistical significance was inferred by a two-tailed
P value of 0.05.
Results
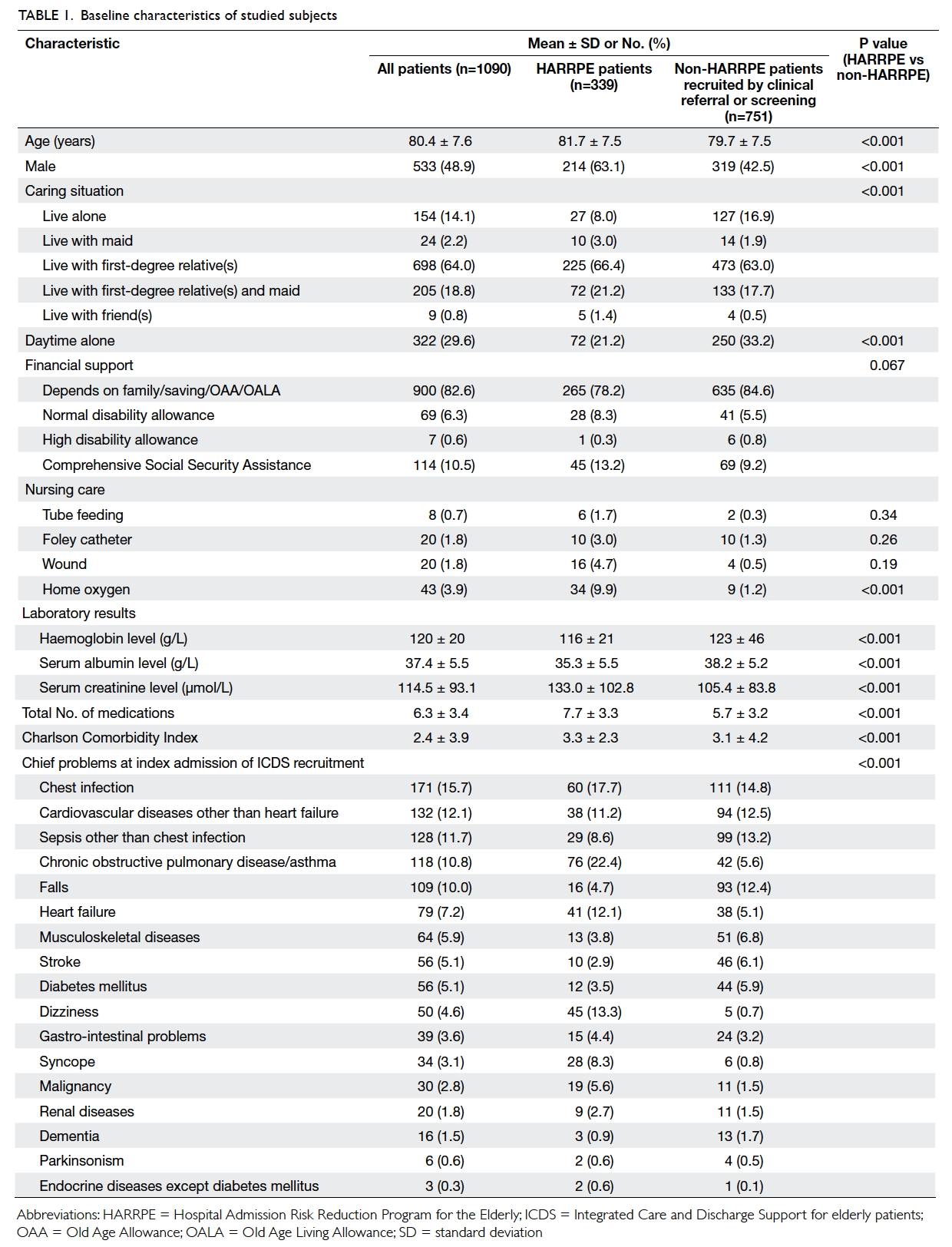
From 1 April 2012 to 30 March 2013, among 7268
hospital discharges, 1184 (16.3%) home-dwelling
older patients aged ≥60 years were recruited to the
ICDS in HKWC. Of these patients, 23 died, 32 were
institutionalised, and 39 refused to join the ICDS
before the first home visit. A total of 1090 patients
entered into the study. The baseline characteristics,
demography, CCI, and chief problems at index
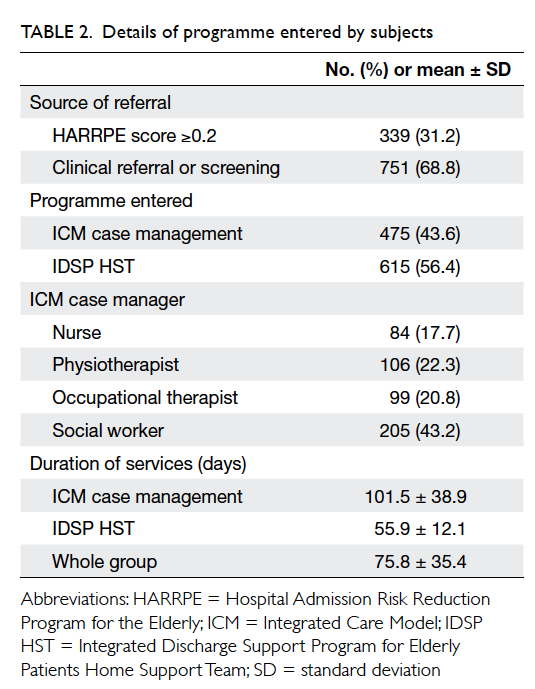
admission of ICDS recruitment are shown in Table 1. Details of the programme entered are shown
in Table 2. Table 3 illustrates the change in AED
attendances, acute hospital admissions, and bed days
(acute and convalescent hospitals) after joining the
ICDS. Within 6 months of ICDS service, 85 (7.8%)
patients died and only 26 (2.4%) older patients
required institutionalisation in RCHEs. We observed
a 40% reduction in AED attendances 6 months after
initiation of the ICDS compared with 6 months before
(mean, 1.2 vs 2.0 episodes; P<0.001). There was also
a 47% reduction in acute hospital admissions (mean,
0.9 vs 1.7 episodes; P<0.001), and a 31% reduction in
bed days (acute and convalescence) [mean, 11.1 vs
16.1 days; P<0.001] 6 months after joining the ICDS
(Table 3).
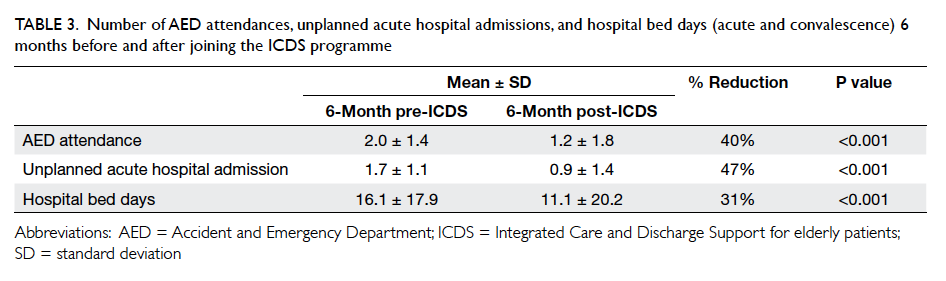
Table 3. Number of AED attendances, unplanned acute hospital admissions, and hospital bed days (acute and convalescence) 6 months before and after joining the ICDS programme
There was mild improvement in MFAC and
BI-20 on discharge from the ICDS compared with
the level at entry (MFAC, 6.3 ± 2.2 vs 5.7 ± 1.6,
P<0.001; BI-20, 17.6 ± 4.1 vs 16.5 ± 4.1, P<0.001).
There was no significant change in AMT (8.4 ± 1.7
vs 8.4 ± 2.1; P=0.831).
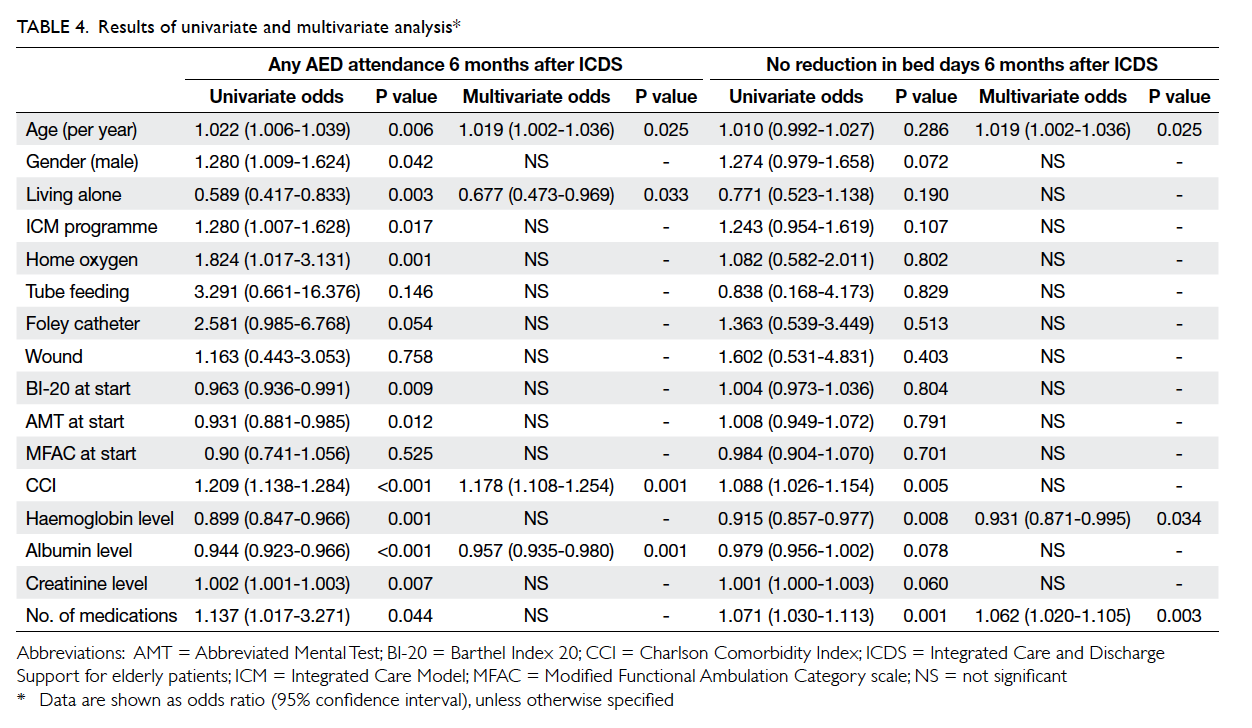
Among 1090 subjects included, 596 (54.7%)
required AED attendance within 6 months of joining
the ICDS. Increasing age (odds ratio [OR]=1.019;
confidence interval [CI], 1.002-1.036; P=0.025)
and high CCI score (OR=1.178; 95% CI, 1.108-1.254;
P=0.001) were independent positive predictors for
AED attendance. A high albumin level (OR=0.957;
95% CI, 0.935-0.980; P=0.001) and living alone
(OR=0.677; 95% CI, 0.473-0.969; P=0.033) were negative
predictors for AED attendance (Table 4). Overall,
310 (28.4%) subjects had no reduction in bed days
when comparing 6 months before and 6 months
after joining the ICDS. Increasing age (OR=1.019;
95% CI, 1.002-1.036; P=0.025) and increasing number of
medications (OR=1.062; 95% CI, 1.020-1.105; P=0.003)
were significant independent positive predictors of
no reduction in bed days; while higher haemoglobin
level (OR=0.931; 95% CI, 0.871-0.995; P=0.034) was a
negative predictor (Table 4).
In HKWC, the cost per patient day was
HK$4461 for an acute-hospital medical bed and
HK$2237 in a convalescent hospital. Each AED
attendance also incurred a cost of HK$877. The
average LOS in an acute medical ward at QMH was
2.4 days. The total number of bed days saved for
acute hospitals were (1.7–0.9) x 1090 x 2.4 = 2093
days. In terms of acute-hospital bed days, the total
cost-saving 6 months following ICDS compared with
6 months before was 2093 x $4461 = HK$9 336 873
(around HK$9.3 million). The total cost-saving for
convalescent-hospital bed days in 6 months was
([16–11] x 1090 – 2093) x $2237 = HK$7 509 609
(around HK$7.5 million). The cost-saving due to
reduced AED attendance was (2.0–1.2) x 1090 x
$877 = HK$764 744 (around HK$0.76 million). The
annual expenditure for the ICDS was HK$12.62
million in total, giving a net cost-saving over 6 months
of (9.3+7.5+0.76) – 12.62/2 = HK$11.25 million.
The potential annual cost-saving was thus HK$11.25
million x 2 = HK$22.5 million (approximately US$2.9
million).
Discussion
This study demonstrates that the present ICDS
in HKWC reduces AED attendance, hospital
admissions, and hospital bed days. A local study
has shown that medical patients are in general
prone to institutionalisation following discharge
from hospital.18 This programme appeared to keep
older patients at home as evidenced by the low
institutionalisation rate (2.4%). Nonetheless there
was selection bias as those who required RCHE
admission direct from hospital were excluded from
the study. Hence, ICDS provided intervention in a
group of older patients who had no imminent need of
institutionalisation at the time of hospital discharge.
Different strategies have been described to
reduce readmissions, namely geriatric assessment,
discharge planning, a case manager approach, post-discharge
support services, early intervention for
ad-hoc medical problems, and use of telephone
nursing services.6 7 8 9 10 11 One important element of
success is a targeted approach that provides services
to high-risk patients.12 In 2010, the Cochrane
Database of Systematic Reviews revealed that a
structured discharge plan tailored to the individual
patient was likely to reduce hospital LOS and
readmission rates for older people.19 The efficacy of a
post-discharge programme that comprises the above
elements was supported by another meta-analysis.20
The ICDS in HKWC comprises all the above elements
with a targeted approach that focuses on high-risk
older patients as identified by their HARRPE score.
In addition, high-risk older patients who were not
identified by a HAPPRE score were recruited as a
result of link nurse screening and clinical referrals in
hospital.
Older patients recruited in the ICDS with
motor and functional problems underwent PT and
OT assessment during home visits. Home exercise
could be taught as appropriate with selected
patients referred to the geriatric day hospital for
rehabilitation. This may help explain why the ICDS
was able to improve the functional and ambulatory
status of patients. We observed no significant AMT
change in our recruited patients upon closure of
ICDS. The ICDS aims at maintaining older patients
in the community during the high-risk period rather
than improving their cognitive function.
Multivariate analysis revealed that increasing
age, low albumin level, and high CCI score were
associated with AED attendance 6 months after
joining the ICDS. This result was very similar to
that of a systematic review of the general risk factors
for preventable readmissions.21 It concluded that
increasing age and poor health as measured by CCI
were associated with high readmission risk.21 Low
serum albumin level is known to associate with
poorer clinical and rehabilitation outcomes in older
patients.22 In this study, patients with advanced
age, low albumin level, and high CCI score were
more likely to attend AED again, even after joining
the ICDS programme. Based on these results, we
may consider adjusting our programme to target
these ‘ultra high-risk’ groups. In this study, living
alone was a protective factor for AED attendance 6
months after joining the ICDS. Although previous
studies showed that living alone was a risk factor
for hospital admission, we found that this group of
patients had significantly fewer AED attendances
after ICDS.23 24 Indeed, age, albumin level and CCI
were all better in the living alone group compared
with those who were not. Living alone remained a
protective factor after multivariate analysis with the
above-mentioned factors adjusted, indicating that
it was an independent predictor by itself. There are
several possible explanations for this observation.
First, older people living at home alone belong to
a selected group who are usually more self-reliant.
With home visits and telephone support by ICDS
case managers or HST, together with geriatrician
backup, they have a dependable team from whom
advice can be sought for ad-hoc problems. On the
contrary, those living with their family might be
less independent. Their health-seeking behaviour is
strongly influenced by family members or carers at
home, who may prompt them or bring them to the
AED for urgent consultations.
In this study, there was a group of patients for
whom there was no reduction in bed days 6 months
after joining the ICDS. These patients were in
more advanced age, with a low haemoglobin level,
and prescribed an increasing number of drugs. It is
possible that the outcome of the ICDS may be further
improved by correcting the anaemia and reducing
polypharmacy in this group of older patients.
There were several limitations in this study. The
study was not a randomised controlled trial. The
ICDS programme is a government-funded service
provided to all suitable older patients in Hong
Kong. Hence, it was practically impossible to have
a control group in the study. Bias in determining
patients’ discharge time might occur as there was no
blinding of treating doctors in the programme. The
decision and time to discharge was subjective and
could have been affected by health care workers who
wanted the programme to demonstrate beneficial
results. The link nurses in the programme could not
perform discharge planning in 100% of the admitted
high-risk patients, as their service was limited on
public holidays and Sundays. In addition, only
16.3% of patients were recruited to the programme
after discharge planning. These factors might
have led to selection bias in the study. Seasonal
variation in hospital admissions among high-risk
older patients might also affect the validity of the
results. Nonetheless, our patients joined the ICDS
at different time points during recruitment and
this, to a certain extent, may minimise the seasonal
variation effect on hospital admission analysis.
Statistically, no adjustment was made for AED
attendance and hospital admissions for patients who
were institutionalised or who died during the post–6-month period. The reduced number of patients
due to deaths was also not considered during the
end of study analysis. The appropriate analysis
would use Cox’s regression, making use of the time
to event (AED attendance), and subjects who died
or were institutionalised during the follow-up period
would be censored and not just excluded from the
analysis. Since the index admission was counted as
the pre-ICDS period, unplanned admission during
the pre-ICDS period would start from ‘one’, putting
the performance during that period at a great
disadvantage when compared with the post-ICDS
period. This study only looked at patients admitted to
hospitals in HKWC. This limited the generalisability
of the results of ICDS in other clusters. The CCI
used in this study was quantified based on ICD
coding in CMS and might have led to undercoding and
consequent underestimation of CCI for patients.
Although there was a potential annual cost-saving
of HK$22.5 million with the ICDS, this was just a
crude calculation and saving based on reduced
bed days: reduced AED attendance provided a
nominal saving. There was no actual reduction in
staff requirements and other expenses as a result of
reduced admissions. In addition, we did not consider
planned readmissions that also contributed to
health care expenditure. The ICDS is designed to
prevent unplanned readmission. The ICM case
managers and HST rarely interfere with planned readmission
for patients, apart from reminding them
to follow the schedule. Thus analysis of the planned
readmissions might not have impacted greatly on our
study findings.
Conclusion
The ICDS reduces AED attendance, unplanned acute
hospital admissions, and hospital bed days in high-risk
older patients. Additional studies are suggested
to determine whether further reductions can be
achieved by modifying some of the predictive factors
identified in this study. A more detailed auditing is
also warranted to demonstrate the value of ICDS in
reducing health care costs.
References
1. Gordon A. ‘Revolving door syndrome’. Elder Care 1995;7:9-10,12.
2. Jencks SF, Williams MV, Coleman EA. Rehospitalizations
among patients in the Medicare fee-for-service program.
N Engl J Med 2009;360:1418-28. Crossref
3. Balla U, Malnick S, Schattner A. Early readmissions
to the department of medicine as a screening tool for
monitoring quality of care problems. Medicine (Baltimore)
2008;87:294-300. Crossref
4. Wong EL, Cheung AW, Leung MC, et al. Unplanned
readmission rates, length of hospital stay, mortality,
and medical costs of ten common medical conditions: a
retrospective analysis of Hong Kong hospital data. BMC
Health Serv Res 2011;11:149. Crossref
5. Luk JK, Tuet OS, Chan FH. Unplanned readmission among
older medical patients discharged from an extended care
hospital. International Hospital Federation Convention;
2001 May 15-18; Hong Kong.
6. Luk JK, Or KH, Woo J. Using the comprehensive geriatric
assessment technique to assess elderly patients. Hong
Kong Med J 2000;6:93-8.
7. Naylor MD, Brooten D, Campbell R, et al. Comprehensive
discharge planning and home follow-up of hospitalized
elders: a randomized clinical trial. JAMA 1999;281:613-20. Crossref
8. Hyde CJ, Robert IE, Sinclair AJ. The effects of supporting
discharge from hospital to home in older people. Age
Ageing 2000;29:271-9. Crossref
9. Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd
S, Rubin HR. Comprehensive discharge planning with
postdischarge support for older patients with congestive
heart failure: a meta-analysis. JAMA 2004;291:1358-67. Crossref
10. Steward S, Pearson S, Horowitz JD. Effects of a home-based
intervention among patients with congestive heart
failure discharged from acute hospital care. Arch Intern
Med 1998;158:1067-72. Crossref
11. Lim WK, Lambert SF, Gray LC. Effectiveness of case
management and post-acute services in older people after
hospital discharge. Med J Aust 2003;178:262-6.
12. Coleman EA, Parry C, Chalmers S, Min SJ. The care
transitions intervention: results of a randomized controlled
trial. Arch Intern Med 2006;166:1822-8. Crossref
13. Chan S, Kwong P, Kong B, et al. Improving Health of High
Risk Elderly in the Community—the HARRPE. Proceedings
of the Symposium on Community Engagement III “Creating a Synergy for Community Health” 2008; Hong Kong. Hong Kong: Hong Kong Hospital Authority; 2008.
14. Ng MF, Sha KY, Tong BC. Bridging the gap: win-win from
Integrated Discharge Support for Elderly Patients. HA Convention; 2011.
15. Chan TC, Luk JK, Chu LW, Chan FH. Validation study of
Charlson Comorbidity Index in predicting mortality in Chinese older adults. Geriatr Gerontol Int 2013;14:452-7. Crossref
16. Chu LW, Pei CK, Ho MH, Chan PT. Validation of the
Abbreviated Mental Test (Hong Kong version) in the elderly medical patients. Hong Kong Med J 1995;1:207-11.
17. Mahoney FI, Barthel DW. Functional evaluation: The
Barthel index. Md State Med J 1965;14:61-5.
18. Luk JK, Chiu PK, Chu LW. Factors affecting
institutionalization in older Chinese patients after recovery from acute medical illnesses. Arch Geront Geriatr
2009;49:e110-4. Crossref
19. Shepperd S, McClaran J, Phillips CO, et al. Discharge
planning from hospital to home. Cochrane Database Syst Rev 2010;(1):CD000313.
20. Fox MT, Persaud M, Maimets I, Brooks D, O’Brien K,
Tregunno D. Effectiveness of early discharge planning in acutely ill or injured hospitalized older adults: a systematic review and meta-analysis. BMC Geriatr 2013;13:70. Crossref
21. Vest JR, Gamm LD, Oxford BA, Gonzalez MI, Slawson KM.
Determinants of preventable readmissions in the United States: a systematic review. Implement Sci 2010;5:88. Crossref
22. Luk JK, Chiu PK, Tam S, Chu LW. Relationship between
admission albumin levels and rehabilitation outcomes in older patients. Arch Gerontol Geriatr 2011;53:84-9. Crossref
23. Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult
C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission
among community-dwelling Medicare beneficiaries. Gerontologist 2008;48:495-504. Crossref
24. Hanania NA, David-Wang A, Kesten S, Chapman
KR. Factors associated with emergency department dependence of patients with asthma. Chest 1997;111:290-5. Crossref