Hong Kong Med J 2015 Aug;21(4):304–9 | Epub 9 Apr 2015
DOI: 10.12809/hkmj144350
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Pain management programme for Chinese patients: a 10-year outcome review
MC Chu, FFPMANZCA1;
Rainbow KY Law, MPhil2;
Leo CT Cheung, MSc3;
Marlene L Ma, MNurs4;
Ewert YW Tse, MSc5;
Tony CM Wong, PhD6;
PP Chen, FFPMANZCA7
1 Department of Anaesthesia, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
2 Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
3 Department of Physiotherapy, Alice Ho Miu Ling Nethersole Hospital, Tai Po, Hong Kong
4 Pain Management Centre, Alice Ho Miu Ling Nethersole Hospital, Tai Po, Hong Kong
5 Department of Occupational Therapy, Alice Ho Miu Ling Nethersole Hospital, Tai Po, Hong Kong
6 Department of Clinical Psychology, United Christian Hospital, Kwun Tong, Hong Kong
7 Department of Anaesthesiology and Operating Services, Alice Ho Miu Ling Nethersole Hospital, Tai Po, Hong Kong
Corresponding author: Dr MC Chu (chu0079@cuhk.edu.hk)
Abstract
Objectives: To review the clinical and social benefits
of a pain management programme in Hong Kong.
Design: Prospective cohort study.
Setting: Tertiary out-patient clinic, Hong Kong.
Participants: Patients with chronic non-cancer pain and prolonged (mean, 46 months) psychosocial disability who joined the Comprehensive Outpatient Pain Engagement programme between 2002 and 2012.
Intervention: A structured 6-week out-patient pain rehabilitation course designed to improve function and reduce disability, regardless of the cause or severity of pain.
Main outcome measures: Social outcomes included return-to-work rate, hospital admissions, and out-patient visits. Physical outcomes included tolerance to sitting and standing. Psychological constructs such as mood, catastrophisation, self-efficacy, quality of life, and perceived performances were used. Each measure was taken before and 1 year after the programme.
Results: There was significant increase in return-to-work rate 1 year after commencement of the programme (35% after vs 17% before the programme; odds
ratio=3.01), reduction in medical utilisation, and improvement in all physical and psychological
measures. Pain intensity, psychological distress, and history of work-related injuries were not related to
the likelihood of return to work. Shorter duration of pain and higher physical functioning score in
36-Item Short-Form Health Survey were prognostic indicators.
Conclusions: Patients with chronic pain who joined the Comprehensive Outpatient Pain Engagement programme showed significant functional
improvement despite the long history of pain.
New knowledge added by this
study
- A programme of pain management based on cognitive behavioural principles is an effective treatment with potentially significant social savings for sufferers of chronic non-cancer pain in Hong Kong.
- The pain programme is an effective treatment, and shall be a significant part of chronic pain rehabilitative services in Hong Kong.
Introduction
Chronic pain is a common condition that affects
about 10% of the population in Hong Kong.1 Patients
with chronic pain suffer a variety of physical and
psychological co-morbidities, become medically
dependent, and have significant loss of quality of life
and work capacity.2
Pain management programmes based
on cognitive behavioural principles have been
recognised as an effective treatment for various
chronic pain conditions.3 Such programmes are
structured to incorporate a variety of rehabilitative
strategies, with clearly defined physical,
psychological, and social outcomes. Such concepts
and practices are, however, largely unknown to the
Chinese community.
In 2002, the Comprehensive Outpatient Pain
Engagement (COPE) programme was established
at the Alice Ho Miu Ling Nethersole Hospital,
Hong Kong, with reference to the model of the
Active Day Patient (ADAPT) programme at the
University of Sydney, Australia.4 This is a 14-day out-patient
rehabilitation programme with 100 hours
of clinical time per course. Core topics included
education about pain pathophysiology, behavioural
training with graded activities and exercises, pacing,
relaxation, strengthening and stretching exercises,
thought management, communication, as well as
activity planning and appropriate use of medication.
Individuals from multiple disciplines participated in
the programme, including pain specialists, clinical
psychologists, physiotherapists, occupational
therapists, pain nurses, medical social workers,
and hospital chaplains. To ensure consistency,
all staff members were trained at the same Pain
Management and Research Centre at the University
of Sydney, and all courses were conducted according
to a standardised timetable and protocol5 in use
since its inception. From 2002 to 2012, 20 courses
were conducted, with one to three courses per year,
and eight to 12 participants per course.
An interim review in 20075 demonstrated
improved physical, psychological, and social
functioning among participants up to 1 year after
the programme. The major limitation of that report
was the small number of subjects (n=49). This
report is an extended outcome study of the pain
management programme. With more subjects,
statistical significance should be improved.
Methods
All participants were recruited from the Pain
Management Centre at the Alice Ho Miu Ling
Nethersole Hospital, a tertiary referral centre in
Hong Kong. They were patients with chronic non-cancer
pain, irrespective of site and diagnosis.5
They were assessed by the clinical psychologist,
pain nurse, and pain specialist for eligibility to join
the programme as a possible pain management
option. Those with untreated psychiatric conditions,
significant suicidal or homicidal risk, illiterate (either
written or spoken Cantonese), and non-acceptance
to the therapy were not included in the study
or the programme. Once recruited, prospective
participants gave written informed consent for data
collection and research, and agreement that medical
treatment for pain control would remain unchanged
until the programme commenced. On completion of
the programme, routine follow-ups were arranged
for up to 1 year.
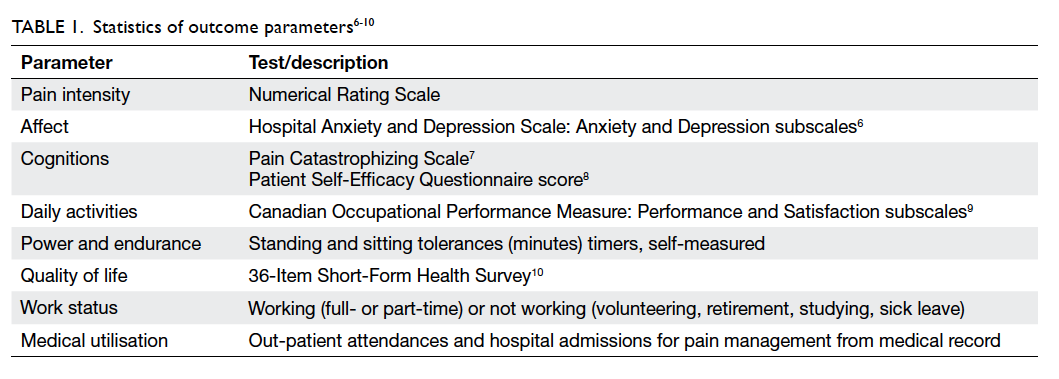
A standardised set of measurements (Table
16 7 8 9 10) was used to assess the physical, psychological, and social functioning on the first day of the
programme, and 12 months after each course. These
measurements were self-reporting, self-administered
questionnaires commonly used among pain clinics
in Hong Kong and staff were familiar with the
measurement tools. All measurements were made
in Chinese and were validated in the local setting.
Medical records of every participant were reviewed
1 year before and after the programme for history of
injury, work status, pain-related admissions, or out-patient
consultations.
Demographic and pain information were
presented as descriptive statistics. Paired t test,
Wilcoxon signed rank test, and contingency table
with Fisher’s exact test were used to evaluate the
overall effectiveness of the programme. Logistic
regression predicting 12-month return-to-work
status was performed with a history of injury at
work, age, duration of pain, and the 36-Item Short-Form Health Survey (SF36) physical functioning as
covariates using the ‘enter’ regression method. The
Statistical Package for the Social Sciences (Windows
version 10.0; SPSS Inc, Chicago [IL], US) was used
for the calculations. A level of significance of P or
Z<0.05 was accepted for the study.
This study was approved by the local ethics
committee (Joint CUHK-NTEC Clinical Research
Ethics Committee CREC2013.205).
Results
From 2002 to 2012, up to 4000 new cases of chronic
pain were assessed at the clinic, and 158 patients
were recruited. The exact number of patients for
each of the exclusion criterion was unknown. Over
the years, 14 participants withdrew during the
course, and two defaulted from post-programme
reviews. A total of 142 participants completed the
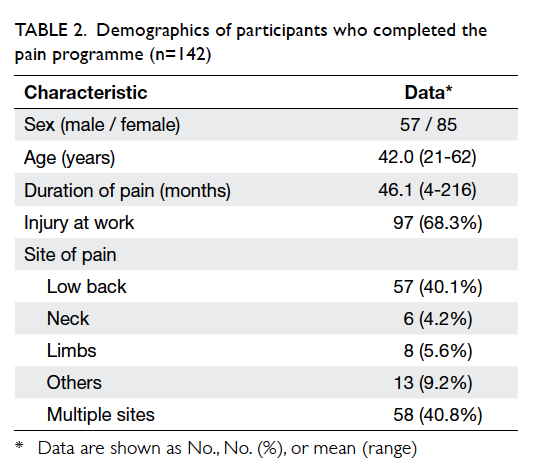
course (Table 2).
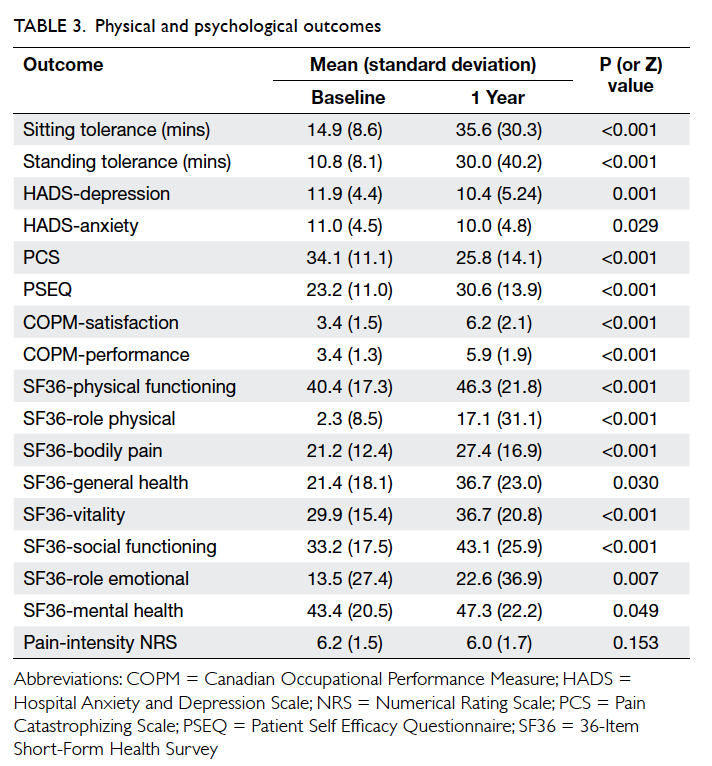
There was a significant improvement in all of
the physical and psychological parameters 1 year
after the programme despite a long history (mean,
46 months) of signs and symptoms before the
programme (Table 3). Despite similar pain-intensity
ratings, functional tolerance (such as sitting and
standing) had more than doubled. Depression,
anxiety, and catastrophisation (psychological
tendency to ruminate and magnify negative aspects
of pain and health) scores were reduced. Self-efficacy,
perceived performance and satisfaction with daily
activities, and quality-of-life scores had improved.
All changes were statistically significant (P<0.05).
There was also a considerable improvement
in work status (Table 4). Of the 142 participants,
only 24 (17%) were working before the programme.
The work statuses of 129 participants were known
after the programme, of whom 49 (35%) were in
work (including 28 who were not working before
the programme). The odds ratio (OR) of participants
working after the programme versus before was
3.01 (95% confidence interval, 1.71-5.30; P=0.0002).
Further analysis of the 106 patients who were
not working initially revealed that baseline pain
intensity was similar among those who returned to
work and those who did not (Table 5). There were
also no statistically significant differences in the
psychological and physical parameters except a
higher SF36 physical functioning score (47.5 vs 39.0).
Other significant differences included younger age
(39.1 vs 44.0 years) and shorter duration of pain (28.3
vs 50.5 months) among those who returned to work.
History of injury at work was also more common in
this group (OR=3.36, Table 4). Logistic regression on
these four significant variables predicting 12-month
return-to-work status showed that duration of pain
(OR=0.955, P=0.020) and SF36 physical functioning
(OR=1.041, P=0.002) were significant independent
predictors, while history of injury at work and age
were not (Table 6).
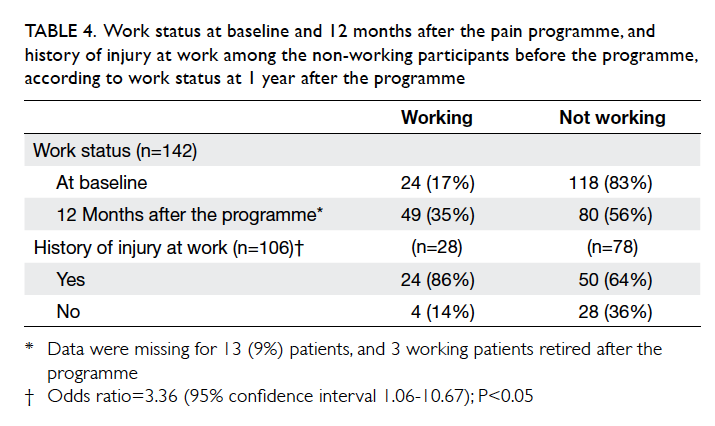
Table 4. Work status at baseline and 12 months after the pain programme, and history of injury at work among the non-working participants before the programme, according to work status at 1 year after the programme
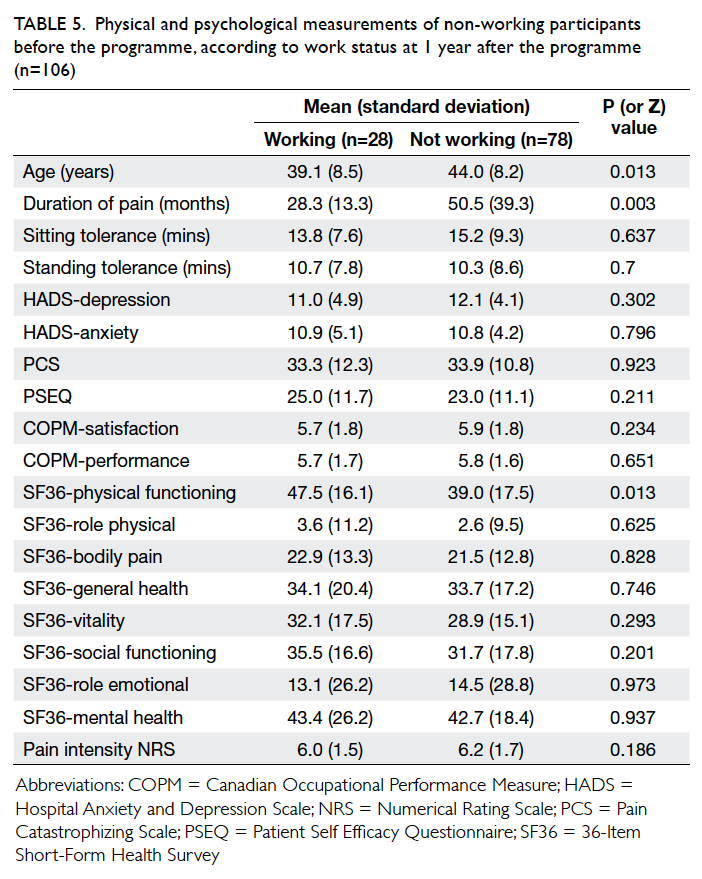
Table 5. Physical and psychological measurements of non-working participants before the programme, according to work status at 1 year after the programme (n=106)
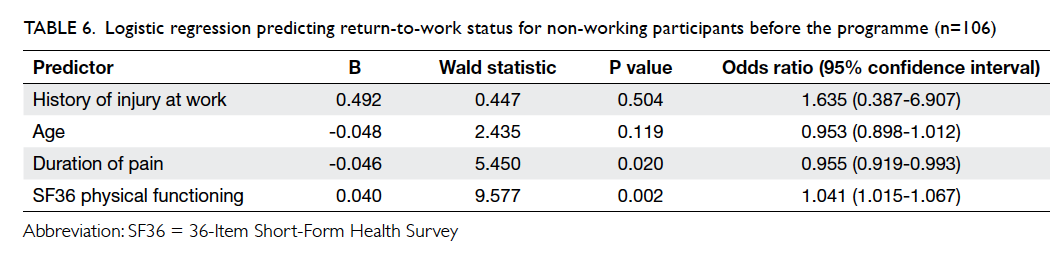
Table 6. Logistic regression predicting return-to-work status for non-working participants before the programme (n=106)
Utilisation of medical resources was also
significantly reduced after the programme: average
out-patient attendance (visits per person per year)
reduced from 7.95 to 6.39, and hospitalisation
(admissions per person per year) reduced from 0.59
to 0.21. All changes were statistically significant
(P<0.05).
Discussion
The COPE programme is one of the first pain
programmes for psychosocial rehabilitation of
patients with chronic non-cancer pain in a Chinese
community. As the concepts of self-management,
active coping, and functional improvement
despite pain were new to the local patients and
staff, it took a considerable effort to train staff and
encourage local patients to join the programme.
The slow recruitment prevented the authors from
performing any randomised trial, and the sample
size was statistically unrepresentative of the
local chronic pain caseload (up to 400 new cases
per year, recruitment rate of approximately 4%).
Some important information, such as reasons for
exclusion from the programme, were not included in
the database. Selection bias might further limit the
usefulness of the information.
Despite the limitations, the results
demonstrated an all-round positive outcome for
patients who completed the programme. The
programme was not designed for pain reduction
and indeed the pain intensity never changed, yet
the participants became less fearful about pain and
movement, and were able to continue to function
despite the pain. The skills learnt in the programme
were simple, self-managing, did not require special
equipment or medications, and participants were
encouraged to solve problem and adopt these skills
in their own social setting. As the participants
managed to see the dissociation between pain and
disability, they become motivated to apply these
skills continuously. This may have contributed to the
lasting improvement.
The social improvement was very encouraging.
Not only was there a lasting reduction in utilisation
of medical resources, it came as a pleasant surprise
that about one quarter of non-working participants
were able to resume work. This is remarkable as this
was a cohort with very long duration of pain, with
most of the participants out of work for more than
2 years. It would also have been an unfavourable
course of prolonged work absenteeism for patients
with musculoskeletal pain and work-related
injuries.11 12 13 Our post-hoc analysis reconfirmed that it remained a significant prognostic indicator of
vocational outcome even after years of disability. As
work was such an important outcome for the patient
and the society, it would be useful to examine if early
intervention could generate better return-to-work
outcomes.
Another interesting finding was that most of
the biological and psychological parameters were
not associated with vocational outcome after the
programme. In other words, while the psychological
‘yellow flags’ might be useful in chronic pain and
disability prognosis,14 they might not be predictive of
vocational outcome among this cohort of subjects.
Apart from the long duration, our cohort of patients
was characterised by very low quality-of-life scores
in multiple domains. The poor psychological
profile might have rendered most psychological
measurements less discriminative than reported
elsewhere.15 The only significant psychological
prognostic indicator was a higher SF36 physical
functioning score. This domain was known to
have the strongest association with return-to-work
among all the SF36 domains for subjects with
chronic back pain,15 and stood out among other less
discriminative domains for predicting outcome.
Other prognostic factors, such as the patients’
expectation, social background, occupational ‘blue
flags’ and the contextual ‘black flags’, might be in
place and need further exploration.16 17 18 The economy
might have also contributed to the favourable
vocational outcome. However, the annual drop
in unemployment (approximately 1%) during the
period19 was much lower than the observed increase
in work rate at 1 year (18%), and was probably a
minor contribution to the overall improvement.
The relationship between compensable injuries and
return to work is much debated. Our data suggested
that history of injury at work might have been an
associating rather than independent variable in
vocational outcome, with other confounding factors
such as age or SF36. During each programme, the
long-term goal setting would include a discussion
on the impact of litigation and compensation on
returning to work and may have reduced their
potential detrimental effects.
Our findings provide a comparison with
those from other non-cancer pain rehabilitation
programmes in Hong Kong. In 2010, Luk et al20
published their rehabilitation programme outcome
for patients with chronic low back pain. Following
almost 400 hours of physiotherapy and occupational
therapy, physical function improved although mood
remained unchanged at 6 months.20 Approximately
52% of the participants returned to work 6 months
after the programme.20 Those who returned to work
showed a reduction in perceived disability, pain
intensity, better physical performance, and similar
mood compared with those who did not.20 The
apparent discrepancy between Luk et al’s study20 and
our study was due to differences in patient cohort and
programme design. In Luk et al’s study,20 the average
pain history was 22 months. These parameters
compared favourably with our cohort of mean pain
history of 46 months. Patients were referred from
different sources (orthopaedics and pain clinics)
with a different demographic (predominantly male
in Luk et al’s group20 vs predominantly female in ours)
and disease profile (exclusively back patients in Luk
et al’s group20 vs heterogeneous in ours). The duration
of therapy was almost 4 times longer in Luk’s study,20
allowing ample time for work strengthening and
vocational training. On the contrary, our programme
was designed for general rehabilitation and offered no
vocational training. The comparison demonstrated
the wide variety of presentation of pain patients, and
the spectrum of therapies available in Hong Kong
with different objectives and emphasis. Nonetheless
both studies were in agreement that duration of
absence from work was unanimously identified as a
prognostic indicator for return to work.
In 2012, Tse et al21 published their outcome
report of a pain management programme for chronic
non-cancer pain among elderly home residents.
Over 290 elderly subjects enrolled in the 8-week
programme with physical exercises and multisensory
art and craft therapy, together with pain education
for their carer. The pain intensity in some areas (back
and multiple joints) was significantly reduced after
the programme, together with increased range of
motion in all joints, and improvement in selected
mood measurements. Perceived quality of life, as
measured by SF12, did not differ significantly after
the programme. There were no data on physical
function, pain cognition, and social consequences.
As the patient group and the programme design and
outcome measurements were radically different to
our study and that of Luk et al,20 results could not be
compared nor conclusions drawn.
The practice of a multidisciplinary pain
programme has also begun recently in Asia. In 2012,
Cardosa et al22 reported a series of 120 patients who
underwent the MENANG programme in Malaysia, a
programme based on the same model (the ADAPT
programme) as ours. Despite the differences in
ethnicity, language and religion, the physical and
psychological improvement was comparable to
that of patients from Australia and Hong Kong. The
efficacy was maintained despite the modifications
made in both Asian programmes to adapt to the local
culture and customs. The challenges of organising
a pain programme were clearly felt by both Asian
groups, as the small sample sizes suggest.
There are significant limitations to this study.
The small sample size recruited from one single
centre made it difficult to extrapolate the findings to
another local chronic pain population. This was also
an observational study although data were collected
prospectively, and there was no control therapy group
for comparison. The data set were primarily physical
and psychological constructs, and some important
social factors associated with return to work were
not collected (such as the ‘blue flag’ factors) and
included in the analyses, hence confounding was
possible. There was also a lack of information about
those who were excluded from the programme and
why, thus significant selection (and self-selection)
bias is present. Prospective randomised controlled
trials are needed to confirm the effectiveness of the
programme, or to compare the efficacy of different
programmes with different designs.
Conclusions
The cognitive behavioural–based pain management
programme improved quality of life and reduced
disability for selected patients with chronic non-cancer
pain in Hong Kong. More patients returned to
work after the programme, and they consumed less
medical resources, with potentially significant social
savings. The strongest association with returning
to work was a brief duration of pain rather than the
baseline intensity of pain, compensable injuries,
physical impairment, or psychological distress of the
subject.
Acknowledgements
The authors would like to thank the multidisciplinary
pain management team at the Alice
Ho Miu Ling Nethersole Hospital, and the Pain
Management and Research Centre at the University
of Sydney for their assistance in the development
of the COPE programme, data collection, and
manuscript preparation.
References
1. Ng KF, Tsui SL, Chan WS. Prevalence of common chronic
pain in Hong Kong adults. Clin J Pain 2002;18:275-81. Crossref
2. Blyth FM, March LM, Nicholas MK, Cousins MJ. Chronic
pain, work performance and litigation. Pain 2003;103:41-7. Crossref
3. Chou R, Huffman LH; American Pain Society; American
College of Physicians. Nonpharmacologic therapies for acute
and chronic low back pain: a review of the evidence for an
American Pain Society/American College of Physicians
clinical practice guideline. Ann Intern Med 2007;147:492-504. Crossref
4. Nicholas M, Molloy A. Manage your pain: practical and
positive ways of adapting to chronic pain. Australia: ABC
Books; 2001.
5. Man AK, Chu MC, Chen PP, Ma M, Gin T. Clinical
experience with a chronic pain management programme
in Hong Kong Chinese patients. Hong Kong Med J
2007;13:372-8.
6. Leung CM, Wing YK, Kwong PK, Lo A, Shum K. Validation
of the Chinese-Cantonese version of the hospital anxiety
and depression scale and comparison with the Hamilton
Rating Scale of Depression. Acta Psychiatr Scand
1999;100:456-61. Crossref
7. Yap JC, Lau J, Chen PP, et al. Validation of the Chinese Pain
Catastrophizing Scale (HK-PCS) in patients with chronic
pain. Pain Med 2008;9:186-95. Crossref
8. Lim HS, Chen PP, Wong TC, et al. Validation of the Chinese
version of pain self-efficacy questionnaire. Anesth Analg
2007;104:18-23. Crossref
9. Carpenter L, Baker GA, Tyldesley B. The use of the Canadian
occupational performance measure as an outcome of a
pain management program. Can J Occup Ther 2001;68:16-22. Crossref
10. Lam CL, Gandek B, Ren XS, Chan MS. Tests of scaling assumptions
and construct validity of the Chinese (HK) version
of the SF-36 Health Survey. J Clin Epidemiol 1998;51:1139-47. Crossref
11. Frank JW, Brooker A, DeMaio SE, et al. Disability resulting
from occupational low back pain: Part II: What do we know
about secondary prevention? A review of the scientific
evidence on prevention after disability begins. Spine (Phila
Pa 1976) 1996;21:2918-29. Crossref
12. Lötters F, Burdorf A. Prognostic factors for duration of
sickness absence due to musculoskeletal disorders. Clin J
Pain 2006;22:212-21. Crossref
13. Cheng AS, Hung LK. Socio-demographic predictors of
work disability after occupational injuries. Hong Kong J
Occup Ther 2007;17:45-53. Crossref
14. Buck R, Barnes MC, Cohen D, Aylward M. Common health
problems, yellow flags and functioning in a community
setting. J Occup Rehabil 2010;20:235-46. Crossref
15. Gatchel RJ, Mayer T, Dersh J, Robinson R, Polatin P. The
association of the SF-36 health status survey with 1-year
socioeconomic outcomes in a chronically disabled spinal
disorder population. Spine (Phila Pa 1976) 1999;24:2162-70. Crossref
16. Kuijer W, Groothoff JW, Brouwer S, Geertzen JH, Dijkstra
PU. Prediction of sickness absence in patients with chronic
low back pain: a systematic review. J Occup Rehabil
2006;16:439-67. Crossref
17. Iles RA, Davison M, Taylor NF. Psychosocial predictors
of failure to return to work in non-chronic non-specific
low back pain: a systematic review. Occup Environ Med
2008;65:507-17. Crossref
18. Buck R, Porteous C, Wynne-Jones G, Marsh K, Phillips CJ,
Main CJ. Challenges to remaining at work with common health
problems: what helps and what influence do organisational
policies have? J Occup Rehabil 2011;21:501-12. Crossref
19. Hong Kong unemployment rate. Available from: http://www.tradingeconomics.com/hong-kong/unemploymentrate.
Accessed 26 Sep 2014.
20. Luk KD, Wan TW, Wong YW, et al. A multidisciplinary
rehabilitation programme for patients with chronic low
back pain: a prospective study. J Ortho Surg (Hong Kong)
2010;18:131-8.
21. Tse MM, Vong SK, Ho SS. The effectiveness of an
integrated pain management program for older persons
and staff in nursing homes. Arch Gerontol Geriatr
2012;54:e203-12. Crossref
22. Cardosa M, Osman ZJ, Nicholas M, et al. Self-management
of chronic pain in Malaysian patients: effectiveness trial
with 1-year follow up. Transl Behav Med 2012;2:30-7. Crossref