Hong Kong Med J 2015 Aug;21(4):333–8 | Epub 17 Jul 2015
DOI: 10.12809/hkmj144397
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Efficacy and outcomes of transobturator tension-free
vaginal tape with or without concomitant
pelvic floor repair surgery for urinary stress
incontinence: five-year follow-up
Tracy SM Law, MB, ChB;
Rachel YK Cheung, FHKCOG, FHKAM (Obstetrics and Gynaecology);
Tony KH Chung, MD;
Symphorosa SC Chan, FHKCOG, FHKAM (Obstetrics and Gynaecology)
Department of Obstetrics and Gynaecology, The Chinese University of
Hong Kong, Prince of Wales Hospital, Shatin, Hong Kong
This paper was presented at the 4th Annual Scientific Meeting of the Obstetrical and Gynaecological Society of Hong Kong (ASM OGSHK), 25 May 2014, Hong Kong
Corresponding author: Dr Tracy SM Law (tracylaw@cuhk.edu.hk)
Abstract
Objectives: To compare the 5-year subjective and
objective outcomes of transobturator tension-free
vaginal tape alone versus the same procedure
with concomitant pelvic floor repair surgery for
pelvic organ prolapse in women with urinary stress
incontinence.
Design: Prospective cohort study.
Setting: Urogynaecology unit at a university hospital
in Hong Kong.
Patients: Of 218 women, 96 (44%) received
transobturator tension-free vaginal tape alone and
122 (56%) received transobturator tension-free
vaginal tape with concomitant pelvic floor
repair surgery from September 2004 to December
2009. The women were followed up annually for up
to 5 years after the operation.
Main outcome measures: The 5-year subjective and
objective cure rates were assessed. Subjective cure
was defined as no urine loss during physical activity
and objective cure was defined as no urine leakage
on coughing during urodynamic study.
Results: Overall, 88 women receiving transobturator
tension-free vaginal tape alone and 101 women
receiving transobturator tension-free vaginal
tape with concomitant pelvic floor repair surgery
were followed up for 5 years after operation. The
subjective and objective cure rates of the two groups
were 70.5% versus 94.1% (P<0.01) and 80.3% versus
85.7% (P=0.58), respectively.
Conclusions: Transobturator tension-free vaginal
tape is an effective treatment for urinary stress
incontinence in women who received it alone or
with concomitant pelvic floor repair surgery for
pelvic organ prolapse, providing high subjective and
objective efficacy for up to 5 years after operation.
Transobturator tension-free vaginal tape with
concomitant pelvic floor repair surgery achieved
similar, if not better, long-term outcome compared with
transobturator tension-free vaginal tape alone.
New knowledge added by this study
- Transobturator tension-free vaginal tape (TO-TVT) is an effective treatment for urinary stress incontinence in women who received it alone or with concomitant pelvic floor repair surgery for pelvic organ prolapse (POP).
- TO-TVT can be performed along with pelvic floor repair surgery in women with POP, with a high cure rate.
Introduction
Urinary stress incontinence (USI) is a common
distressing problem affecting women worldwide.
The prevalence of USI ranges from 19% to 55%
for different age-groups and communities with
a prevalence of 33.8% in Hong Kong.1 2 3 4 It has a
significant adverse impact on quality of life for
12% of women with the condition in Hong Kong.3 4 5
Surgical treatment with tension-free vaginal tape
(TVT) is a known effective and durable procedure
for patients in whom conservative treatment with
pelvic floor exercises is unsuccessful.6 Retropubic
TVT was first introduced in 1996 and long-term
follow-up success rates of up to 77% have been
reported 11 years after the procedure.6 However,
TVT is associated with risk of bladder, urethra
and vessel injuries, and voiding dysfunction.7 The
development of transobturator TVT (TO-TVT)
reduced the rate of complications with comparable
efficacy to retropubic TVT in the short term.8 Such
technique is now the first choice for the surgical
treatment of USI.
Nearly 40% of women with pelvic organ
prolapse (POP) have symptoms of USI and they
often receive both continence surgery and pelvic
floor repair (PFR) surgery at the same time. Yip and
Pang9 compared women who underwent retropubic
TVT with or without concomitant PFR surgery and
concluded that TVT was equally effective with or
without concomitant surgery for treatment of USI
in women in Hong Kong. There is, however, little
information on the efficacy of TO-TVT in this group
of women.
The primary outcome of this study was to
assess the objective and subjective cure rates at 1
and 5 years after operation in women with USI who
received TO-TVT performed alone versus those
who received TO-TVT with concomitant PFR surgery
for POP. The secondary outcome was to compare
any long-term complications of TO-TVT in both
groups of women.
Methods
This was a prospective study involving all women
with USI presenting to the out-patient clinic of a university
hospital. All data were collected
prospectively and input to a database established
in 1996. There were 218 women with USI who
received TO-TVT between 1 September 2004 and
31 December 2009. Ethics approval was obtained
from the Institutional Review Board to conduct
multifaceted analysis of this database (Clinical
Research Ethics: CRE-2009.080).
Demographic information was obtained
from all women with USI, followed by physical
examination, including the standard POP
quantification assessment, in the out-patient
clinic. All women underwent standard urodynamic
investigation, including uroflowmetry and filling and
voiding cystometry following standards published by
the International Continence Society10 with a Dantec
Menuet (from 2004-2009; Dantec Medical A/S, Skovlunde, Denmark) or Maquet Radius (from 2009-2013; Maquet GmbH & Co. KG, Rastatt, Germany) multichannel urodynamic machine.
Women with USI who did not improve after
pelvic floor exercise were offered TO-TVT.5 Women
who had USI only underwent TO-TVT surgery, while
women with both USI and POP received TO-TVT
and concomitant PFR surgery. Vaginal hysterectomy
and anterior or posterior colporrhaphy were
performed accordingly as PFR surgery. Women with
a history of predominant detrusor overactivity (DO),
previous continence procedures, or transvaginal
mesh repair for POP were excluded from the study.
Women with mental incapacity were also excluded.
Women had either TOT (outside-in technique;
Monarc Subfascial Hammock, American Medical
Systems Inc., Minnetonka [MN], US) performed
from September 2004 to June 2006 or TVT-O
(inside-out technique; Gynecare TVT obturator
system, Ethicon Inc [NJ], US) performed from July
2006 to December 2009 in the same urogynaecology
centre. The change from TOT to TVT-O was
because TVT-O was becoming available. In this
study, 124 women underwent TOT and 94 women
underwent TVT-O. Cheung et al11 reported TOT
and TVT-O had high and similar subjective and
objective efficacy (81%-84%). All procedures were
performed or supervised by a urogynaecologist
according to the original techniques.12 13 Cystoscopy was performed after the procedure to identify any
bladder or urethral injury. The urinary catheter was
removed the next day, voiding volume and pattern
was reviewed, and post-voiding residual urine was
measured. Women were discharged if residual urine
was less than 100 mL.
Women were followed up 2 months after
operation and then reviewed annually for 5 years.
They were assessed subjectively by asking whether
their USI symptoms became ‘better’, ‘same’, or ‘worse’.
If there was no urine leakage when performing
physical activities, the women were regarded as
having ‘subjective cure’ of the USI. Those who
responded ‘better’ but had persistent or recurrent
USI symptoms were regarded as ‘subjective better’,
irrespective of the frequency and amount of urinary
leakage. Patients were asked whether they had
voiding difficulty, urgency, groin or vaginal pain, or
dyspareunia. Physical examination was conducted to
check for POP and vaginal tape erosion. Urodynamic
study was repeated at 1 and 5 years to assess the
objective outcome. Severity of USI was classified
according to the degree of urine leakage in the
cough stress test: mild (following a series of coughs),
moderate (with a few coughs), and marked (with a
single cough). Objective cure was defined as no urine
leakage upon coughing during urodynamic study.
The cough stress test is a well-established test for
USI with sensitivity of 98% and specificity of 100%.14
However, there was no standard set to categorise
the severity of USI during urodynamic study. Thus,
cough stress test was used to further categorise the
severity of USI. Detrusor overactivity was defined as
occurrence of involuntary detrusor contractions of
>15 cm H2O during filling cystometry. Overactive
bladder (OAB) was defined as urinary urgency,
usually accompanied by frequency and nocturia,
with or without urgency urinary incontinence, in the
absence of urinary tract infection or other obvious
pathology.10 Patients who did not return for follow-up
were contacted and offered another appointment.
If they defaulted again, they were interviewed over
the telephone using the same set of questions to
assess subjective outcome. Follow-up would be ceased if there was no significant problem after the 5-year follow-up.
Data were analysed using the Statistical
Package for the Social Sciences (Windows version
17.0; SPSS Inc, Chicago [IL], US). Descriptive
statistics of data were presented as mean ± standard
deviation or number (%). Categorical variables were
compared using Chi squared test or Fisher’s exact
test. Continuous variables were compared using
independent sample t test. A P value of <0.05 was
considered statistically significant.
Results
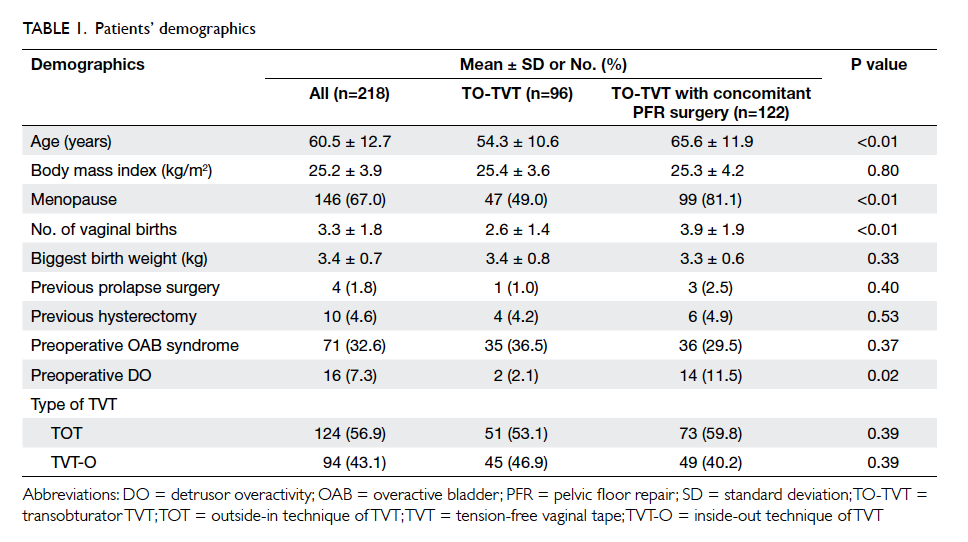
Of 218 women who underwent TO-TVT between
1 September 2004 and 31 December 2009, 96 (44%)
women had USI only and underwent TO-TVT
alone, while 122 (56%) had USI and POP and
underwent TO-TVT with concomitant PFR surgery.
The PFR surgery was usually vaginal hysterectomy
with anterior colporrhaphy. For preoperative data
(Table 1), women who underwent TO-TVT and PFR
surgery were older (mean, 65.6 vs 54.3 years; P<0.01), had
higher parity (mean, 3.9 vs 2.6; P<0.01), and had more DO
(11.5% vs 2.1%; P=0.02).
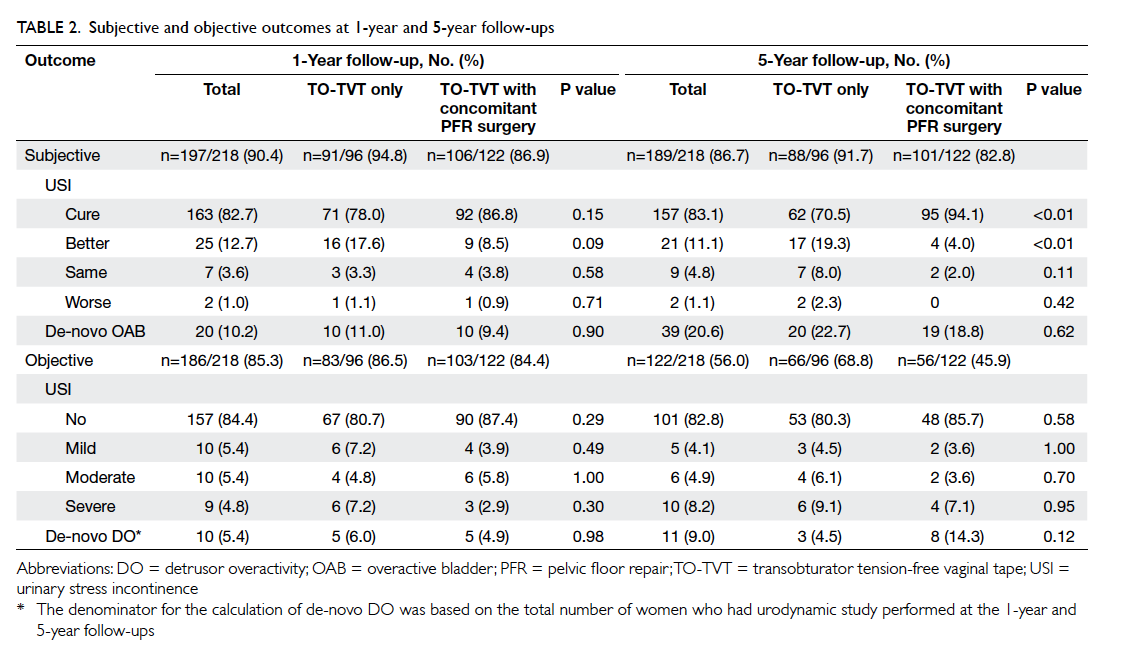
At 1 year after surgery, 197 (90.4%) women
were reviewed at follow-up and 186 (85.3%) had
urodynamic study. At 5 years, 189 (86.7%) women
were either reviewed at follow-up or contacted
by telephone (20 women) and 122 (56.0%) had
urodynamic study. The mean follow-up times
were similar: 59.3 ± 8.0 months for the TO-TVT
group and 58.6 ± 8.0 months for the TO-TVT with
concomitant PFR surgery group.
The subjective cure rate at 1 year was 78.0% for
the TO-TVT group and 86.8% for the TO-TVT with
concomitant PFR surgery group (Table 2); respective objective cure rate at 1 year was 80.7% and
87.4%. There was no statistical difference between
the two groups. At 5 years, the subjective cure rate
was 70.5% for the TO-TVT group and 94.1% for
the TO-TVT with concomitant PFR surgery group.
Women with TO-TVT with concomitant PFR
surgery had statistically higher satisfaction. There
was no difference in the objective outcome for the two
groups at 5 years (80.3% vs 85.7%). After combining
subjective cure and subjective better as one group
for overall improvement of USI after surgery, the
TO-TVT with concomitant PFR surgery group had
significantly higher subjective improvement at 5
years (P=0.04). None required second operation for
their USI during the 5-year follow-up.
In the study group, 10.2% and 20.6% had
de-novo OAB at 1 and 5 years, respectively, and
there was no statistical difference between the
TO-TVT group and TO-TVT with concomitant PFR
surgery group. More women developed de-novo
DO at 5 years in the TO-TVT with concomitant
PFR surgery group compared with TO-TVT group
(14.3% vs 4.5%; P=0.12), although it did not reach
statistical difference. Eight (8.3%) women in the
TO-TVT group with de-novo OAB required medical
treatment for their symptoms and five (4.1%) women
in the TO-TVT with concomitant PFR surgery group
required treatment (P=0.30).
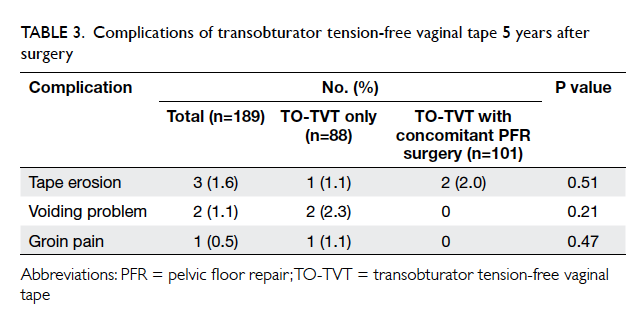
No neurological complications resulting from
the surgery were reported. Three women (two in
the concomitant PFR surgery group and one in the
TO-TVT alone group) had tape erosion requiring
excision of the exposed tape (Table 3). The patients
all presented with vaginal pain. The exposed tape
was cut and the vaginal skin was repaired under
local or regional anaesthesia. All three women
had no recurrence of USI after tape excision at the
5-year follow-up. Two women (both from TO-TVT
alone group) developed voiding difficulty with OAB
symptoms and the tape was cut at 4 months and 18
months after the operation, respectively. Their voiding problem
was resolved and both had no recurrence of USI
after tape release. One woman (in the TO-TVT alone
group) had groin pain 4 years after the operation and
was treated conservatively with analgesics.
Discussion
Transobturator TVT has been proven to be safe
and highly effective,11 15 and has become a standard treatment for USI. Pelvic floor repair surgery is
commonly performed at the same time as continence
surgery.16 However, there is limited information
comparing the long-term efficacy of TO-TVT in
women with or without concomitant PFR surgery.
This study evaluated 5-year subjective and objective
outcomes in the two treatment groups of women
with USI alone and those having USI and POP who
required treatment for both conditions.
Women in the TO-TVT with concomitant PFR
surgery group were older, had had a higher number
of vaginal births, and more were menopausal and
had DO. This observation is likely due to the age of
the women, as risk of DO also increases with age and
more women had pre-existing DO in this group.
Subjective cure in our study was defined as
feeling completely dry after TO-TVT operation. The
5-year subjective cure rate of the TO-TVT alone
group was 70.5%. Although this appears to be lower
than in the concomitant PFR surgery group of 94.1%,
the result is comparable to most of the published
data on long-term efficacy of TO-TVT. Angioli et
al17 showed a 62% patient satisfaction rate and 73%
objective success rate at 5 years. Abdel-Fattah et al18
also showed a 73% patient-reported success rate for
TO-TVT at 3-year follow-up in 238 women.
We hypothesised that women with
concomitant PFR surgery had a higher subjective
cure rate because anterior colporrhaphy added an
anti-incontinence effect. Furthermore, the main
symptoms for this group of women might be related
to POP so treating their POP could raise their
overall satisfaction. Recurrence of POP may mask
the symptoms of USI, but this hypothesis requires
further analysis, as the recurrence rate of POP was
not collected in this study. The above factors may
account for the higher subjective cure rate observed,
although the objective cure rates were high in both
groups.
The 5-year overall
subjective and objective cure rates were 83.1% and
82.8%, respectively, which are similar to international
figures.19 20 Athanasiou et al19 reported 7-year
overall subjective and objective cure rates of 83.5%
and 81.5%, which included women who received
TO-TVT alone or with concomitant PFR surgery,
but there was no statistical comparison between the
groups. Tsivian et al20 reported 82.9% versus 85.2%
continence rates in patients undergoing TO-TVT
alone versus those who received concomitant
vaginal surgery at a mean follow-up period of up to
3 years. These studies, however, were either small or
had short follow-up durations.
The long-term complication rate of TO-TVT is
low. The most commonly encountered morbidity was
de-novo DO after TO-TVT (9% at 5 years), which is similar to
that reported in the literature.17 19 Athanasiou et al19 reported 7% de-novo urgency 7 years after TVT-O
and Angioli et al17 found a 5-year de-novo urgency
rate of 6.4%. The higher percentage of women
developing de-novo DO at 5 years (9.0%) when
compared with 1 year (5.4%) could be attributed
to ageing. This difference also suggests that more
women had de-novo DO in the prolapse group
(14.3%) than in the TO-TVT alone group (4.5%)
as the mean age of the prolapse group was higher.
Our 5-year study also shows low rates of mesh
erosion and voiding dysfunction after operation,
and concomitant surgery does not impose higher
complication rates.
We recommend TO-TVT with concomitant
PFR surgery as the treatment of choice for women
with symptomatic POP and USI. A recent meta-analysis
showed a reduced risk of postoperative
USI after combination surgery (mid-urethral sling
with prolapse surgery) relative to prolapse surgery
alone (5% vs 23%) for women with prolapse and
symptomatic USI.21 In asymptomatic women with
prolapse, however, only 7% required subsequent
surgery for de-novo USI. Therefore, even with the
promising result of combination surgery, it should
only be performed in symptomatic incontinent
women instead of as routine surgery for all women
with prolapse because TO-TVT is not a risk-free
procedure. Thus, preoperative evaluation of urinary
symptoms and urodynamic study still plays a role in
individual treatment planning.
There are limitations in this study. This was not
a randomised controlled study and there was lack
of blinding when assessing the objective outcomes.
There were significant differences between the
characteristics of the two groups (Table 1), and
further randomised study is warranted to find out
whether those factors contribute to the differences
observed in subjective outcomes. We lacked a
detailed questionnaire to evaluate the subjective
cure rate and to assess quality-of-life aspect after the
operation. The validated questionnaires in Chinese
were only available after the study period.22 23 However, our previous study has confirmed the improvement in quality of life of women receiving
continence surgery with or without PFR surgery.24
Although the response rate for subjective outcome measure was high at 5 years (overall response, 86.7%),
fewer women (56.0%) returned for objective
assessment using urodynamic study at 5 years.
Conclusions
Transobturator TVT is an effective treatment for USI
in women who received it alone or with concomitant
PFR surgery. This technique provides high subjective
and objective efficacy for up to 5 years with a good
safety profile. Transobturator TVT with concomitant
PFR surgery achieved similar, if not better, long-term
outcomes when compared with TO-TVT alone.
References
1. Zhu L, Lang J, Liu C, Han S, Huang J, Li X. The
epidemiological study of women with urinary incontinence
and risk factors for stress urinary incontinence in China.
Menopause 2009;16:831-6. Crossref
2. Thom D. Variation in estimates of urinary incontinence
prevalence in the community: effects of differences in
definition, population characteristics, and study type. J Am
Geriatr Soc 1998;46:473-80. Crossref
3. Pang MW, Leung HY, Chan LW, Yip SK. The impact of
urinary incontinence on quality of life among women in
Hong Kong. Hong Kong Med J 2005;11:158-63.
4. Cheung RY, Chan S, Yiu AK, Lee LL, Chung TK. Quality
of life in women with urinary incontinence is impaired and
comparable to women with chronic diseases. Hong Kong
Med J 2012;18:214-20.
5. Fan HL, Chan SS, Law TS, Cheung RY, Chung TK. Pelvic
floor muscle training improves quality of life of women
with urinary incontinence: a prospective study. Aust N Z J
Obstet Gynaecol 2013;53:298-304. Crossref
6. Nilsson CG, Palva K, Rezapour M, Falconer C. Eleven years
prospective follow-up of the tension-free vaginal tape
procedure for treatment of stress urinary incontinence. Int
Urogynecol J Pelvic Floor Dysfunct 2008;19:1043-7. Crossref
7. Boustead GB. The tension-free vaginal tape for treating
female stress urinary incontinence. BJU Int 2002;89:687-93. Crossref
8. Agur W, Riad M, Secco S, et al. Surgical treatment
of recurrent stress urinary incontinence in women: a
systematic review and meta-analysis of randomised
controlled trials. Eur Urol 2013;64:323-36. Crossref
9. Yip SK, Pang MW. Tension-free vaginal tape sling procedure
for the treatment of stress urinary incontinence in Hong
Kong women with and without pelvic organ prolapse:
1-year outcome study. Hong Kong Med J 2006;12:15-20.
10. Haylen BT, de Ridder D, Freeman RM, et al. An
International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the
terminology for female pelvic floor dysfunction. Neurourol
Urodyn 2010;29:4-20. Crossref
11. Cheung RY, Chan SS, Yiu KW, Chung TK. Inside-out
versus outside-in transobturator tension-free vaginal
tape: a 5-year prospective comparative study. Int J Urol
2014;21:74-80. Crossref
12. Jonsson Funk M, Levin PJ, Wu JM. Trends in the surgical
management of stress urinary incontinence. Obstet
Gynecol 2012;119:845-51. Crossref
13. Olsson I, Abrahamsson AK, Kroon UB. Long-term efficacy
of the tension-free vaginal tape procedure for the treatment
of urinary incontinence: a retrospective follow-up 11.5
years post-operatively. Int Urogynecol J 2010;21:679-83. Crossref
14. Swift SE, Yoon EA. Test-retest reliability of the cough
stress test in the evaluation of urinary incontinence. Obstet
Gynecol 1999;94:99-102. Crossref
15. Houwert RM, Renes-Zijl C, Vos MC, Vervest HA. TVT-O
versus Monarc after a 2-4-year follow-up: a prospective
comparative study. Int Urogynecol J 2009;20:1327-33. Crossref
16. Bai SW, Jeon MJ, Kim JY, Chung KA, Kim SK, Park KH.
Relationship between stress urinary incontinence and
pelvic organ prolapse. Int Urogynecol J Pelvic Floor
Dysfunct 2002;13:256-60; discussion 260. Crossref
17. Angioli R, Plotti F, Muzii L, Montera R, Panici PB, Zullo
MA. Tension-free vaginal tape versus transobturator
suburethral tape: five-year follow-up results of a
prospective, randomised trial. Eur Urol 2010;58:671-7. Crossref
18. Abdel-Fattah M, Mostafa A, Familusi A, Ramsay I, N’dow J.
Prospective randomised controlled trial of transobturator
tapes in management of urodynamic stress incontinence
in women: 3-year outcomes from the Evaluation of
Transobturator Tapes study. Eur Urol 2012;62:843-51. Crossref
19. Athanasiou S, Grigoriadis T, Zacharakis D, Skampardonis
N, Lourantou D, Antsaklis A. Seven years of objective and
subjective outcomes of transobturator (TVT-O) vaginal
tape: why do tapes fail? Int Urogynecol J 2014;25:219-25. Crossref
20. Tsivian A, Benjamin S, Tsivian M, et al. Transobturator
tape procedure with and without concomitant vaginal
surgery. J Urol 2009;182:1068-71. Crossref
21. van der Ploeg JM, van der Steen A, Oude Rengerink K, van
der Vaart CH, Roovers JP. Prolapse surgery with or without
stress incontinence surgery for pelvic organ prolapse: a
systematic review and meta-analysis of randomised trials.
BJOG 2014;121:537-47. Crossref
22. Chan SS, Cheung RY, Yiu AK, et al. Chinese validation of
Pelvic Floor Distress Inventory and Pelvic Floor Impact
Questionnaire. Int Urogynecol J 2011;22:1305-12. Crossref
23. Chan SS, Choy KW, Lee BP, et al. Chinese validation of
Urogenital Distress Inventory and Incontinence Impact
Questionnaire short form. Int Urogynecol J 2010;21:807-12. Crossref
24. Chan SS, Cheung RY, Lai BP, Lee LL, Choy KW, Chung TK.
Responsiveness of the Pelvic Floor Distress Inventory and
Pelvic Floor Impact Questionnaire in women undergoing
treatment for pelvic floor disorders. Int Urogynecol J
2013;24:213-21. Crossref