Hong Kong Med J 2015 Apr;21(2):143–8 | Epub 10 Mar 2015
DOI: 10.12809/hkmj144349
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Impact of nuchal cord on fetal outcomes, mode of delivery, and management: a questionnaire survey of pregnant women
CW Kong, FHKAM (Obstetrics and Gynaecology); Diana HY Lee, MB, BS; LW Chan, FRCOG; William WK To, MD, FRCOG
Department of Obstetrics and Gynaecology, United Christian Hospital, Kwun Tong, Hong Kong
Corresponding author: Dr CW Kong (melizakong@gmail.com)
Abstract
Objectives: To explore pregnant women’s views on
the impact of nuchal cord on fetal outcomes, mode
of delivery, and management.
Design: Questionnaire survey.
Setting: Antenatal clinic of two regional hospitals in
Hong Kong.
Participants: A questionnaire survey of all pregnant
women at their first visit to the antenatal clinic of
United Christian Hospital and Tseung Kwan O
Hospital in Hong Kong was conducted between
August and October 2012.
Results: Most participants (71.8%) were worried
about nuchal cord, and 78.3% and 87.7% of them
thought that nuchal cord could cause intrauterine
death and fetal death during labour, respectively.
Approximately 87.5% of participants thought that
nuchal cord would reduce the chance of successful
vaginal delivery and 56.4% thought that it would
increase the chance of assisted vaginal delivery.
Most (94.1%) participants thought that it was
necessary to have an ultrasound scan at term to
detect nuchal cord. In addition, 68.8% thought that
it was necessary to deliver the fetus early and 72.8%
thought that caesarean section must be performed
in the presence of nuchal cord. Participants born
in Mainland China were significantly more worried
about the presence of nuchal cord than those born
in Hong Kong. However, there was no difference
between participants with different levels of
education.
Conclusion: Most participants were worried about
the presence of nuchal cord. Many thought that
nuchal cord would lead to adverse fetal outcomes,
affect the mode of delivery, and require special
management. These misconceptions should be
addressed and proper education of women is needed.
New knowledge added by this
study
- Most women were worried about the presence of nuchal cord.
- Many women thought that nuchal cord would lead to adverse fetal outcomes, affect the mode of delivery, and require special management.
- Avoiding routine ultrasound scans for nuchal cord in order to reduce needless maternal anxiety and unnecessary caesarean sections on women’s request is warranted.
- The correct concept that nuchal cord would not normally lead to adverse fetal outcomes and that its presence should not affect the mode of delivery should be publicised widely in Hong Kong.
Introduction
In daily clinical practice, pregnant women regularly
request antenatal ultrasound scans to look for nuchal
cord around the time of delivery or request that
the presence of nuchal cord is specifically checked
for when they undergo ultrasound scans for other
obstetric reasons. Many women have requested
elective caesarean sections because nuchal cord has
been detected on ultrasound scan. In order to explore
women’s views on the impact of nuchal cord on fetal
outcomes, mode of delivery and management, we
conducted a questionnaire survey to evaluate their
true concerns and beliefs.
Methods
A questionnaire evaluating the impact of nuchal
cord on fetal outcomes and mode of delivery were
distributed to all pregnant women at their first
antenatal visit to the out-patient clinic of United
Christian Hospital and Tseung Kwan O Hospital
from August to October 2012. The questionnaire
was in three versions: traditional Chinese, simplified
Chinese, and English according to the participant’s
preference (Appendices 1 to 3). Participants who
were not able to understand Chinese or English
were excluded from the study. The questionnaires
were collected by the nursing staff immediately after
completion. Assuming that 50% of the women would
express concern about the presence of nuchal cord,
a sample size of 357 women would allow for random
errors of up to 5%. Assuming the response rate to
the questionnaire to be around 80%, distribution of
around 450 questionnaires would be sufficient.
The Statistical Package for the Social Sciences
(Windows version 20.0; SPSS Inc, Chicago [IL], US)
was used for statistical analysis. Chi squared test and
Fisher’s exact test were used when appropriate. All
the differences were defined as being statistically
significant at P<0.05.
Results
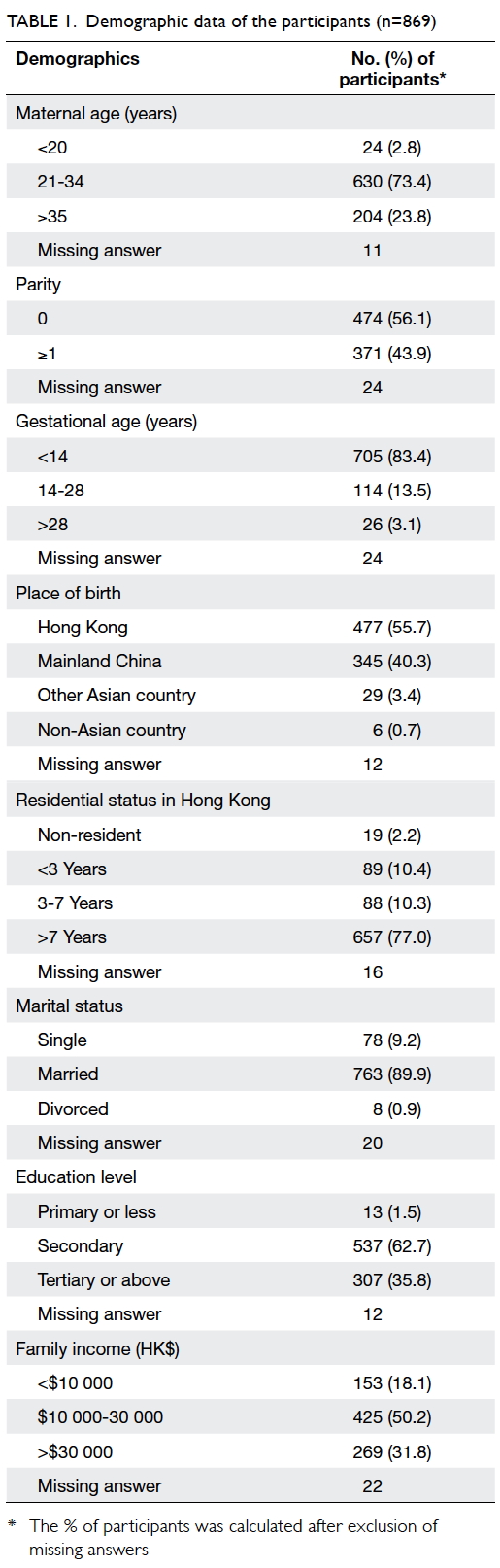
Of 950 questionnaires distributed, a total of
869 (91.5%) questionnaires were received. The
demographic data of the participants are shown in
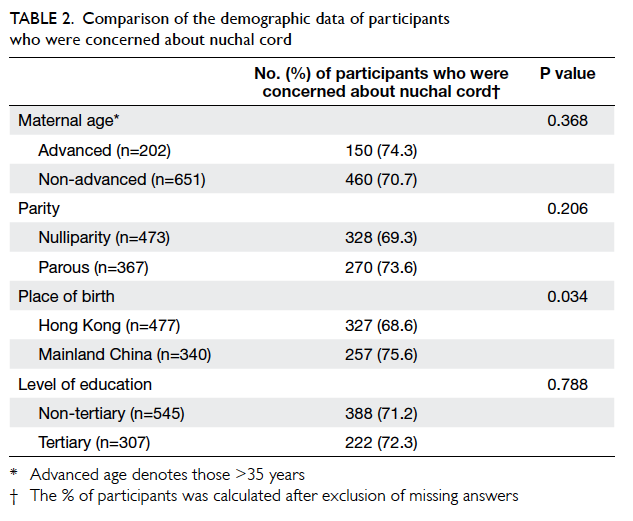
Table 1. Around 72% of participants expressed
worries about nuchal cord. The different demographic
parameters among the participants who expressed
worries about nuchal cord were analysed (Table 2).
Participants born in Mainland China were more
worried about nuchal cord than those born in Hong
Kong. Advanced maternal age, nulliparity, and lower
education level were not associated with higher
maternal anxiety for nuchal cord.
The perceived incidence of nuchal cord was
assessed by a linear scale from 0% to 100%. Excluding
the 50 participants who did not reply to this question,
37.9% thought that the incidence of nuchal cord was
less than 20%. The perceived sonographic accuracy
for nuchal cord was similarly assessed. Around
one third (31.2%) of participants thought that the
accuracy was less than 70% while 35 participants did
not answer this question.
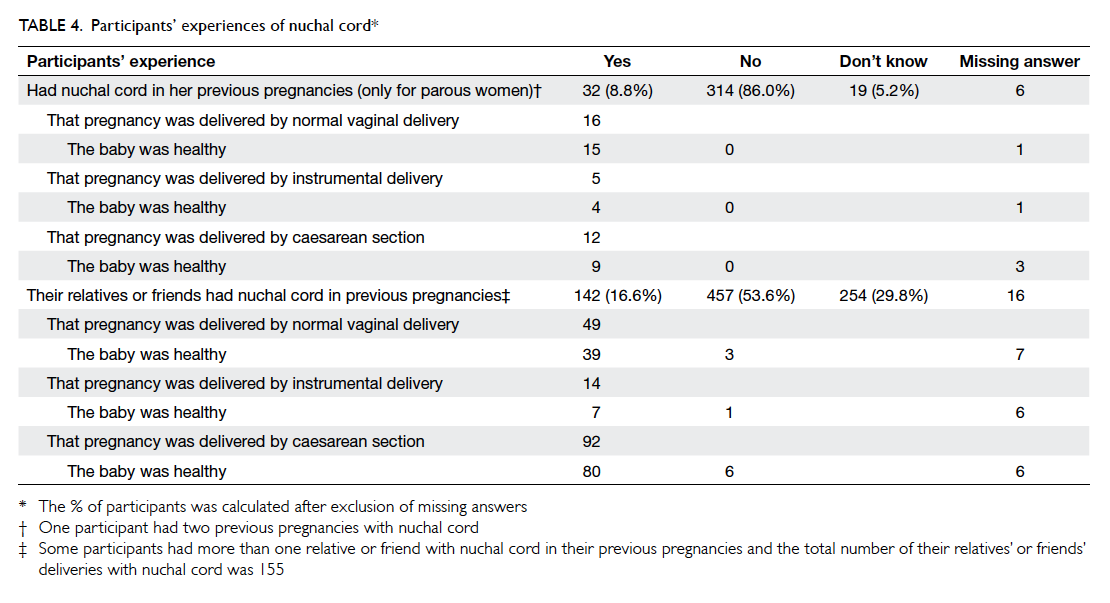
The perceived impact of nuchal cord on fetal
outcomes, mode of delivery, and management are
shown in Table 3. Around 78.3% and 87.7% thought
that nuchal cord could cause intrauterine death and
fetal death during labour, respectively, while 87.5% of
participants thought that it would reduce the chance
of successful vaginal delivery and 56.4% thought
that it would increase the chance of assisted vaginal
delivery. In addition, 94.1% of participants thought
that it was necessary to have ultrasound scan to
detect nuchal cord at term, while 68.8% thought that
it was necessary to deliver the fetus early and 72.8%
thought that caesarean section must be performed
in the presence of nuchal cord.
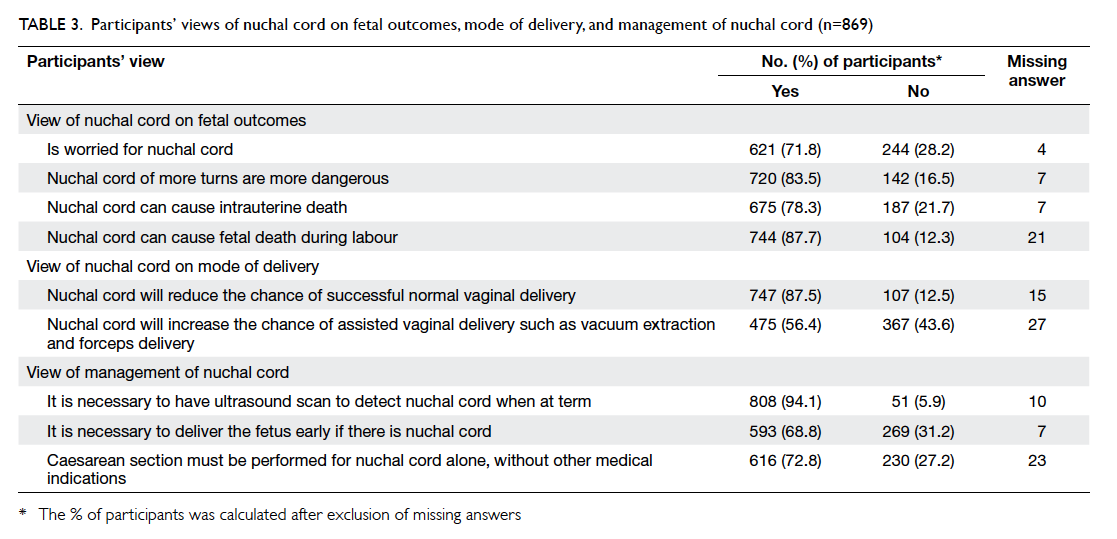
Table 3. Participants’ views of nuchal cord on fetal outcomes, mode of delivery, and management of nuchal cord (n=869)
Women’s experience of nuchal cord from their
previous pregnancies or from their relatives’ or
friends’ deliveries were explored. We asked questions
on the mode of delivery for nuchal cord pregnancies
and whether or not the babies were healthy. Only 32
(8.8%) participants had nuchal cord in their previous
pregnancies; one participant had nuchal cord in
both her previous two pregnancies. Among those
nuchal cord pregnancies, 48.5% of them had normal
vaginal deliveries, 15.2% had instrumental deliveries,
and 36.4% had caesarean sections. None of these
babies were remarked to be unhealthy. A total of 142
(16.6%) participants had relatives or friends who had
nuchal cord in their previous pregnancies, and some
of them had more than one relative or friend who
had nuchal cord in their previous pregnancies. The
total number of their relatives’ or friends’ deliveries
with nuchal cord was 155. Among those nuchal cord
pregnancies, 31.6% of them had normal vaginal
deliveries, 9.0% had instrumental deliveries, and
59.4% had caesarean sections. Approximately 6.5%
of the babies were claimed to be unhealthy by the
participants and such replies were evenly distributed
in the normal vaginal delivery group, instrumental
delivery group, and caesarean section group (Table
4).
Table 5 shows the comparison of the views
between participants with different places of birth
and education levels. Those born in Mainland China
were more likely to believe that nuchal cord led to
assisted instrumental deliveries when compared
with those born in Hong Kong (63.2% vs 50.7%). In
contrast, they were less likely to believe that nuchal
cord led to intrapartum death in labour (84.1%
vs 90.9%) and the need for earlier delivery (64.9%
vs 71.8%). There were no significant differences
between the two groups in their views on the impact
on intrauterine death, chance of successful vaginal
delivery, and whether or not caesarean section was
needed.
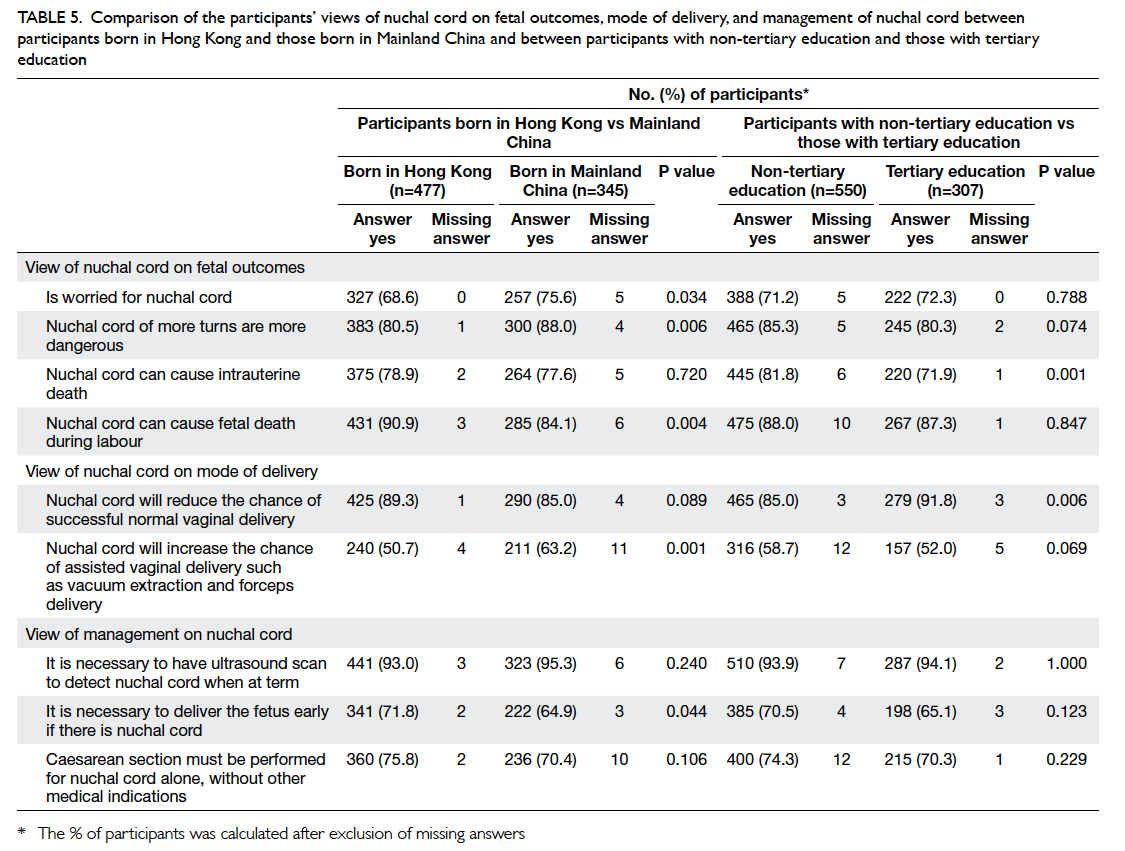
Table 5. Comparison of the participants’ views of nuchal cord on foetal outcomes, mode of delivery, and management of nuchal cord between participants born in Hong Kong and those born in Mainland China and between participants with non-tertiary education and those with tertiary education
For the education level, there was no significant
difference for worry about the presence of nuchal
cord. Those who had received tertiary education
were less likely to believe that nuchal cord led to
intrauterine death (71.9% vs 81.8%). However, more
of this group thought that nuchal cord decreased the
chance of successful normal vaginal delivery (91.8%
vs 85.0%).
Discussion
This questionnaire survey revealed that many of our
participants were worried about nuchal cord. The
percentage (71.8%) was much higher than anticipated,
implying that this issue should be given greater
attention in the antenatal education of pregnant
women. Our local audit showed that the incidence of
nuchal cord was 27% among all singleton deliveries
(n=5166) in 2010 (not published). Therefore, about
one third of the participants underestimated the
incidence of nuchal cord.
It is common for nuchal cord to be the
indication for caesarean section in China, which
accounted for 16.1% to 25.4% of the indications in
a teaching hospital and some regional hospitals
there.1 2 As many participants are immigrants from Mainland China, their views on nuchal cord
were compared with those born in Hong Kong.
Although this survey showed that participants
born in Mainland China were more worried about
nuchal cord than those born in Hong Kong, most
participants in both groups also believed that
nuchal cord could cause intrauterine death (>77%)
and would reduce the chance of successful vaginal
delivery (>85%). Moreover, despite variable levels
of education, most participants also believed that
nuchal cord would cause fetal death during labour
(>87%) and more than 70% thought that caesarean
section was needed in the presence of nuchal cord.
Therefore, it was apparent that misconceptions
about the clinical implications of nuchal cord were
widespread among all groups.
In our survey, only 8.8% of the participants
claimed to have nuchal cord in their previous
pregnancies and none of them reported adverse fetal
outcomes. However, a significant proportion of the
participants’ experiences and impressions on nuchal
cord were from their relatives and friends. From this
survey, the caesarean section rate in participants’
relatives or friends with nuchal cord was high. This
may be one of the reasons why so many participants
thought that caesarean section must be performed
for nuchal cord.
Women were worried about nuchal cord
due to the concept that nuchal cord could lead to
adverse fetal outcomes. Although some studies
showed nuchal cord was associated with increased
prevalence of variable fetal heart rate decelerations
during labour and increased incidence of umbilical
artery acidaemia, higher incidences of lower 1-minute Apgar score and meconium-stained liquor,3 4
these findings may not reflect clinically on fetal wellbeing.
Furthermore, most available studies showed
nuchal cord was not associated with lower Apgar
scores in 5 minutes and was not associated with
increase in caesarean sections, neonatal intensive
care unit admissions, and perinatal mortalities.5
6 7 8 9
Such reassuring evidence supporting the benign
nature of nuchal cord and the absence of true adverse
impact clinically on the fetal outcomes should be
publicised widely to the general population to reduce
their misconceptions and anxiety.
Although 94.1% of participants thought that
it is necessary to have an ultrasound scan to detect
nuchal cord at term, this is not usually necessary.
As almost all participants now have continuous
fetal heart rate monitoring during labour in Hong
Kong, even if there is presence of nuchal cord
causing variable fetal heart rate decelerations during
labour, this will be detected on cardiotocogram and
appropriate actions such as fetal blood sampling or
assisted delivery can be performed when needed.
Avoiding routine ultrasound scans for nuchal
cord should reduce needless maternal anxiety and
unnecessary caesarean sections on participants’
request, as 68.8% thought that it was necessary
to deliver the fetus early and 72.8% thought that
caesarean section must be performed for nuchal
cord.
Conclusion
Many pregnant women are worried about nuchal
cord due to misconceptions on its effect on fetal
outcomes and mode of delivery. Proper education
is necessary to reduce maternal anxiety. The correct
concept that nuchal cord would not normally lead to
adverse fetal outcomes and that its presence should
not affect the mode of delivery should be publicised
widely in Hong Kong.
Appendices
Additional material related to this article can be found on the HKMJ website. Please go to , and search for the article.
References
1. Gao Y, Xue Q, Chen G, Stone P, Zhao M, Chen Q. An
analysis of the indications for cesarean section in a
teaching hospital in China. Eur J Obstet Gynecol Reprod
Biol 2013;170:414-8. Crossref
2. Qin C, Zhou M, Callaghan WM, et al. Clinical indications and determinants of the rise of
cesarean section in three hospitals in rural China. Matern
Child Health J 2012;16:1484-90. Crossref
3. Hankins GD, Snyder RR, Hauth JC, Gilstrap LC 3rd,
Hammond T. Nuchal cords and neonatal outcome. Obstet
Gynecol 1987;70:687-91.
4. Singh G, Sidhu K. Nuchal cord: a retrospective analysis.
Medical Journal Armed Forces India 2008;64:237-40. Crossref
5. Sheiner E, Abramowicz JS, Levy A, Silberstein T, Mazor M,
Hershkovitz R. Nuchal cord is not associated with adverse
perinatal outcome. Arch Gynecol Obstet 2006;274:81-3. Crossref
6. Shrestha NS, Singh N. Nuchal cord and perinatal outcome.
Kathmandu Univ Med J (KUMJ) 2007;5:360-3.
7. Schäffer L, Burkhardt T, Zimmermann R, Kurmanavicius J.
Nuchal cords in term and postterm deliveries—do we need
to know? Obstet Gynecol 2005;106:23-8. Crossref
8. González-Quintero VH, Tolaymat L, Muller AC, Izquierdo
L, O’Sullivan MJ, Martin D. Outcomes of pregnancies
with sonographically detected nuchal cords remote from
delivery. J Ultrasound Med 2004;23:43-7.
9. Peregrine E, O’Brien P, Jauniaux E. Ultrasound detection
of nuchal cord prior to labor induction and the risk of
Cesarean section. Ultrasound Obstet Gynecol 2005;25:160-4. Crossref