Hong
Kong Med J 2018 Dec;24(6):636.e1–2
DOI: 10.12809/hkmj176953
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Caesarean scar ectopic pregnancy: imaging findings of
this rare but potentially life-threatening condition
Joseph Andrew WK Tang, MB, ChB, FRCR1;
Esther MF Wong, MB, BS, FHKAM (Radiology)1; Wendy Shu, MB, BCh,
FHKCOG2
1 Department of Radiology, Pamela Youde
Nethersole Eastern Hospital, Chai Wan, Hong Kong
2 Department of Obstetrics and
Gynaecology, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
Corresponding author: Dr Joseph Andrew WK Tang (tangwingkin2000@gmail.com)
Caesarean scar ectopic pregnancy is a rare
pregnancy complication with an estimated incidence of 1/1800 to 1/2500
pregnancies.1 2 Complications include uterine rupture, massive
haemorrhage, placenta accrete, and pregnancy loss.3 Ultrasound examination is usually the first-line
investigation. Magnetic resonance imaging (MRI) serves as a powerful
confirmation tool. With its inherent superior tissue contrast and
mulitplanar capability, MRI depicts anatomical details with robust
reproducibility.4 Caesarean scar
ectopic pregnancy is associated with a high risk of uterine rupture and
uncontrollable haemorrhage. Expectant management is possible but not
advocated. Surgical treatment leads to quicker postoperative recovery but
may be associated with major haemorrhage.5
Other treatment includes systemic methotrexate and uterine artery
embolisation.3
A high index of suspicion is required to diagnose
this condition so that timely treatment can be initiated and
life-threatening complications from a ruptured ectopic pregnancy
prevented.
Case
A 34-year-old woman with a history of Caesarean
section presented to the emergency department with per vaginal bleeding.
Her pregnancy was 7 weeks of gestation by date.
On vaginal examination, the cervical os was closed
and mildly blood-stained. She was haemodynamically stable with a normal
haemoglobin of 12.9 g/dL and beta–human chorionic gonadotropin 15 877
mIU/mL. Transvaginal ultrasound revealed a single intrauterine gestational
sac in the lower segment of the uterus, closely related to the myometrium
(Fig 1). The fetal pole with positive fetal heart
beat was identified. Crown to rump length was 11 mm, corresponding with 7
weeks and 1 day of gestation. The anterior uterine wall adjacent to the
gestational sac was very thin with a thickness of only 4 mm (Fig
2). However, it was uncertain whether the placenta was directly
implanted onto the Caesarean scar. A provisional diagnosis was made of
pending abortion or Caesarean scar ectopic pregnancy. Magnetic resonance
imaging of the pelvis was performed to determine whether the thin layer of
soft tissue at the anterior uterine wall represented myometrium in the
Caesarean scar with placental implantation elsewhere or if the placental
tissue was implanted directly onto the scar.
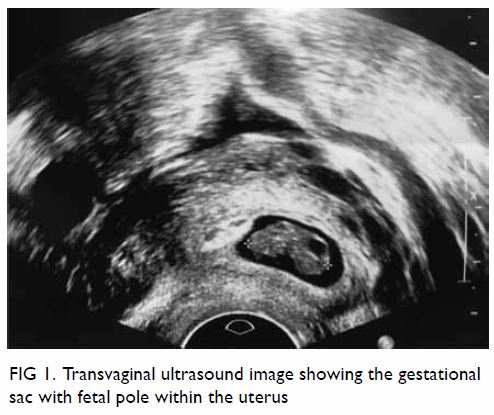
Figure 1. Transvaginal ultrasound image showing the gestational sac with fetal pole within the uterus
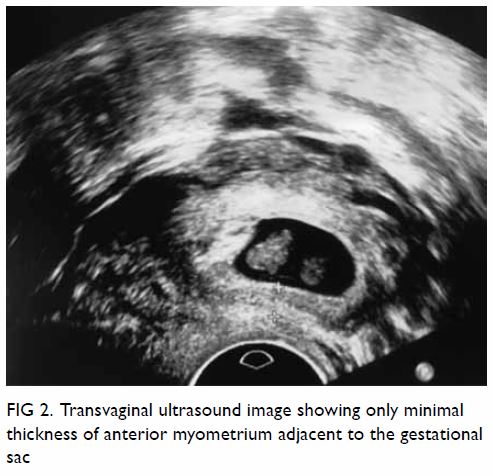
Figure 2. Transvaginal ultrasound image showing only minimal thickness of anterior myometrium adjacent to the gestational sac
Magnetic resonance imaging showed a 1.7-cm defect
at the anterior lower segment of the myometrium, corresponding to the
Caesarean section scar. It was distended by a gestational sac. A singleton
pregnancy was identified with crown-rump length consistent with
gestational age. Trophoblastic tissue was seen implanted onto the serosa
of the uterus (Fig 3). Overall MRI findings were compatible with
Caesarean scar ectopic pregnancy. There was no direct extension of
trophoblastic tissue into adjacent organs such as the urinary bladder or
sign of uterine rupture (Fig 4).
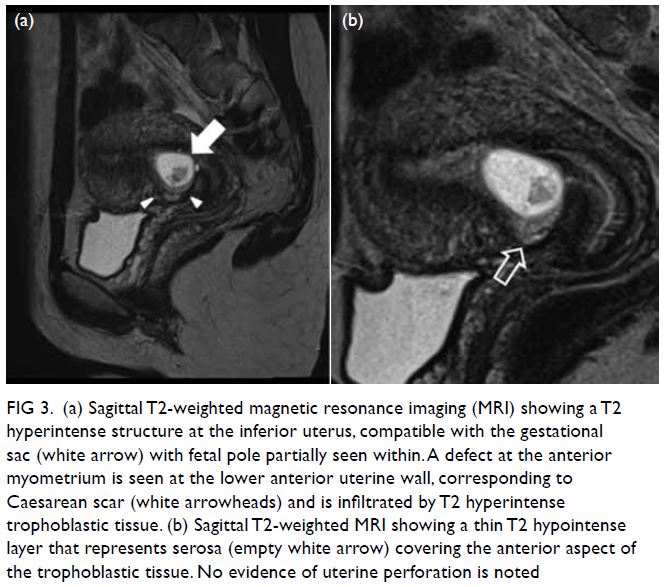
Figure 3. (a) Sagittal T2-weighted magnetic resonance imaging (MRI) showing a T2 hyperintense structure at the inferior uterus, compatible with the gestational sac (white arrow) with fetal pole partially seen within. A defect at the anterior myometrium is seen at the lower anterior uterine wall, corresponding to Caesarean scar (white arrowheads) and is infiltrated by T2 hyperintense trophoblastic tissue. (b) Sagittal T2-weighted MRI showing a thin T2 hypointense layer that represents serosa (empty white arrow) covering the anterior aspect of the trophoblastic tissue. No evidence of uterine perforation is noted
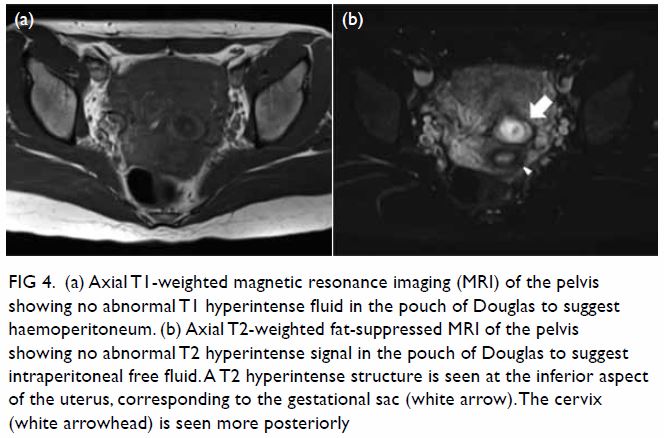
Figure 4. (a) Axial T1-weighted magnetic resonance imaging (MRI) of the pelvis showing no abnormal T1 hyperintense fluid in the pouch of Douglas to suggest haemoperitoneum. (b) Axial T2-weighted fat-suppressed MRI of the pelvis showing no abnormal T2 hyperintense signal in the pouch of Douglas to suggest intraperitoneal free fluid. A T2 hyperintense structure is seen at the inferior aspect of the uterus, corresponding to the gestational sac (white arrow). The cervix (white arrowhead) is seen more posteriorly
The superior contrast resolution in MRI for
different soft tissues is advantageous in the differentiation of uterine
serosa, myometrium, endometrium, and trophoblastic tissue. This helped
confirm the diagnosis of Caesarean scar ectopic pregnancy in our patient
and would have been difficult if only ultrasound findings were available.
The patient received intramuscular methotrexate
therapy. Serial beta–human chorionic gonadotropin levels showed a
decreasing trend. Subsequent definitive treatment with suction evacuation
was performed. The patient made an uneventful recovery.
Author contributions
Concept and design of the study: All authors.
Acquisition of data: EMF Wong, W Shu.
Analysis and interpretation of data: EMF Wong, W Shu.
Drafting of the manuscript: JAWK Tang.
Critical revision for important intellectual content: JAWK Tang, EMF Wong.
Acquisition of data: EMF Wong, W Shu.
Analysis and interpretation of data: EMF Wong, W Shu.
Drafting of the manuscript: JAWK Tang.
Critical revision for important intellectual content: JAWK Tang, EMF Wong.
Declaration
All authors have disclosed no conflicts of
interest. All authors had full access to the data, contributed to the
study, approved the final version for publication, and take responsibility
for its accuracy and integrity.
References
1. Seow KM, Huang LW, Lin YH, Lin MY, Tsai
YL, Hwang JL. Caesarean scar pregnancy: issues in management. Ultrasound
Obstet Gynecol 2004;23:247-53. Crossref
2. Jurkovic D, Hillaby K, Woelfer B,
Lawrence A, Salim R, Elson CJ. First-trimester diagnosis and management of
pregnancies implanted into the lower uterine segment caesarean section
scar. Ultrasound Obstet Gynecol 2003;21:220-7. Crossref
3. Michaels AY, Washburn EE, Pocius KD,
Benson CB, Doubilet PM, Carusi DA. Outcome of cesarean scar pregnancies
diagnosed sonographically in the first trimester. J Ultrasound Med
2015;34:595-9. Crossref
4. Kao LY, Scheinfeld MH, Chernyak V,
Rozenblit AM, Oh S, Dym RJ. Beyond ultrasound: CT and MRI of ectopic
pregnancy. AJR Am J Roentgenol 2014;202:904-11. Crossref
5. Alalade AO, Smith FJ, Kendall CE,
Odejinmi F. Evidencebased management of non-tubal ectopic pregnancies. J
Obstet Gynaecol 2017;37:982-91. Crossref

