DOI: 10.12809/hkmj134155
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Digital ischaemia: a rare but severe complication of jellyfish sting
Stacey C Lam, BS, MB, ChB; YW Hung, FHKCOS, FHKAM (Orthopaedic Surgery);
Esther CS Chow, FHKCOS, FHKAM (Orthopaedic Surgery); Clara WY Wong, FHKCOS, FHKAM (Orthopaedic Surgery); WL Tse, FHKCOS, FHKAM (Orthopaedic Surgery); PC Ho, FHKCOS, FHKAM (Orthopaedic Surgery)
Division of Hand and Microsurgery, Department of Orthopaedics, Prince of
Wales Hospital, Shatin, Hong Kong
Corresponding author: Dr YW Hung (ywhung@ort.cuhk.edu.hk)
Abstract
We report a case of digital ischaemia in a 31-year-old
man who presented with sudden hand numbness,
swelling, and cyanosis 4 days after a jellyfish
sting. This is a rare complication of jellyfish sting,
characterised by a delayed but rapid downhill course.
Despite serial monitoring with prompt fasciotomy
and repeated debridement, he developed progressive
ischaemia in multiple digits with gangrenous change.
He subsequently underwent major reconstructive
surgery and aggressive rehabilitation. Although
jellyfish stings are not uncommon, no severe jellyfish
envenomation has been reported in the past in Hong
Kong and there has not been any consensus on the
management of such injuries. This is the first local
case report of jellyfish sting leading to serious hand
complications. This case revealed that patients who
sustain a jellyfish sting deserve particular attention
to facilitate early detection of complications and
implementation of therapy.
Case report
Our patient was a 31-year-old man with
unremarkable past health. He was swimming in the
waters of Phuket, Thailand, when he experienced
a sudden, intense burning pain in his right arm
and right thigh. He spotted a jellyfish in the water
after the incident. After getting out of the water, he
noticed immediate reddening and swelling over the
right thigh and right upper limb (from elbow down
to the hand). No systemic symptoms were reported.
The locals gave him some water to irrigate the sting
site and slathered a soothing cream on it. He was
then admitted to the local hospital and given a dose
of steroids.
The next day, he was discharged from the
local hospital and returned to Hong Kong. He was
admitted to the Department of Orthopaedics and
Traumatology of Prince of Wales Hospital, Hong
Kong, in July 2013. It was the second day after his
injury, and his right arm was swollen up to the
midarm, and there were multiple maculopapular
lesions over his right thigh and arm (Fig 1a, 1b). The injury site in the right forearm was explored
the same day, revealing healthy subcutaneous tissue,
fascia, and muscle (without features of necrotising
fasciitis). Wound swab culture was negative.

Figure 1. Serial photos showing progressive digital gangrene and large skin defect after repeated debridement
Typical lesion after jelly fish sting over (a) right thigh, (b) elbow, and (c) hand on day 2 after injury: linear; papular whip-like dermatitis (‘tentacle print’). (d) Finger tip with cyanotic changes on day 8 after injury. (e) Well-demarcated gangrenous change over finger tips on day 15 after injury. (f) Extensive skin defect with expose tendon after debridement on day 17 after injury. (g) Reconstruction included a two-stage operation with groin flap to cover the dorsum of hand and a second groin flap to cover gangrene tip (6 weeks after injury). (h) Outcome (attempt to make tight fist) after multiple major reconstruction (8 months after injury)
On the fourth day after the sting, he
experienced sudden onset of numbness and pain in
his right hand which rapidly progressed to almost
complete loss of sensation. The swelling in the right
arm and forearm also increased. The skin was cold
with cyanotic change in all fingers and the thumb;
capillary refill was sluggish (<4 seconds) but with
preserved turgor (Fig 1c). The radial pulse was not palpable. Compartment pressure measured
with Stryker needle revealed superficial flexor
compartment pressure of 35 mm Hg, deep flexor
compartment pressure of 25 mm Hg, and extensor
compartment pressure of 22 mm Hg.
Immediate fasciotomy of the right forearm
was done, revealing subcutaneous oedema but no
evidence of myonecrosis. Arteriotomy was not
performed in view of return of palpable radial and
ulnar pulse. Again, wound swab culture revealed no
bacterial growth. Biopsy revealed muscle necrosis
and infiltrate with white cells (predominantly
polymorph). Postoperatively, he was put in a warm
room with adequate fluid replacement and started
on subcutaneous fraxiparine.
Despite wound debridement and aggressive
medical treatment, 2 weeks after his initial insult,
his right hand circulation remained sluggish,
with progressive gangrenous change in the distal
phalanges of the thumb, index finger, middle finger,
half of the ring finger, and dorsum of the hand (Fig 1d, 1e). Computed tomography angiogram showed that the brachial artery was patent down to the palmar
arch level, suggesting distal small vessel disease. As
such, his gangrene would not be amenable to surgical
intervention. Finally, he had a staged reconstructive
surgery with distal amputation of his distal index
finger and thumb; a groin flap (distant pedicle
flap) was used to cover the major skin defect over
the dorsum of the hand and the thumb (Fig 1f, 1g).
With careful reconstructive surgery and aggressive
rehabilitation, 9 months after the incident, his right
hand regained movement, although it remained
functionally impaired with significant stiffness and
numbness (Fig 1h).
Discussion
Jellyfish belong to a family of Cnidaria found all
over the world. There are more than 2000 different
types of jellyfish, of which approximately 70 are
toxic to humans.1 The pathophysiology of jellyfish
sting is a combination of toxin and immunological
response (immediate allergic reaction and delayed
reaction).2 The toxins are composed of a mixture
of polypeptides and enzymes, leading to local or
systemic inflammatory responses.2 There has also
been a report on toxins causing platelet aggregation.3
Hence, the physiological response of jellyfish sting
depends on the species of jellyfish and the toxins
they release.
The toxin of Cnidaria is located in the
cnidocytes, which are stinging cells composed of
organelles called ‘nematocysts’. Nematocysts are
present on the outer surfaces of tentacles or near the
mouth. These are released when the victim’s skin is
in contact with jellyfish, injecting the venom into the
victim via a thread tube, sufficient to penetrate the
dermis of human skin.2
The majority of jellyfish stings are mild with
local skin reactions. The usual presentation is a
painful papular-urticaria at site of contact, which
looks like multiple whip-like eruptions. This is
compatible with the sting on the right leg in our case,
with a linear whip-like ‘tentacle print’. Lesions can
last for minutes or hours. Other local reactions also
include hyperhidrosis of skin, lymphadenopathy,
fat atrophy, vasospasm, gangrene, and contracture.
Systemic reactions—including gastro-intestinal
symptoms, cardiac arrest, respiratory arrest and
anaphylactic shock—are rare but not impossible.2
Hong Kong is a city surrounded by ocean. Many
people enjoy recreational water sports and, thus,
injury related to marine life is unavoidable. The latest
annual report by the Hong Kong Poison Information
Centre ranked venomous stings and bites as the
seventh commonest cause of poisoning.4 This is
likely an underestimation as most marine accidents
are managed at the scene, and this figure only takes
into account the ones reported. In the English
literature, there have only been three case reports of
serious jellyfish sting injuries leading to serious hand
or foot complications,5 6 7 and our case is the first local
case report. Similar to the sudden deterioration in
our patient, these documented cases all reported
patients who suffered from sudden oedema, cyanotic
changes, and weak pulse. This occurred around 3 to
4 days after the initial insult. In addition, the case
reported by Abu-Nema et al7 noted that the patient
had suffered from arterial spasm complicated by
thrombosis, and was subsequently treated with
urokinase. Our patient shares a similar complication
of vasospasm, as evidenced by patent but diminished
flow in distal arteries. It may be postulated that the
delayed vasospasm and possible thrombosis may
have led to this rare complication of jellyfish sting.
Although jellyfish injuries usually present with acute
skin reactions, our patient presented with clinical
deterioration of the hand on day 4 when the lower
limb skin reaction was actually improving.
The differences between our case and the other
case reports are in terms of alternative management
modalities and complications. Our patient received
fasciotomy, repeated debridement, and fraxiparine.
Some of the other authors incorporated other
surgical interventions such as cervicodorsal or
thoracic sympathectomy and medical treatments
such as dextran, prednisolone, reserpine, and
urokinase in case of thrombosis. Our patient suffered
from gangrenous thumb and fingers. In other case
reports, reported complications ranged from a
mere loss of superficial sensation, to amputation of
necrotic digits with Volkmann’s contracture.
Despite the adverse effects of cnidarian
stings, literature on treatment is limited and often
conflicting. It is difficult to perform high-quality
studies with sound methodology, owing to reasons
including limited number of cases and lack of
randomisation.8 The majority of cases are dealt with
at the scene by the general physician or accident and
emergency department. It is important for us to be
well equipped with management strategies for this
type of injury and maintain a high level of suspicion
for major complications. Our recommendations are
summarised in Figure 2a.
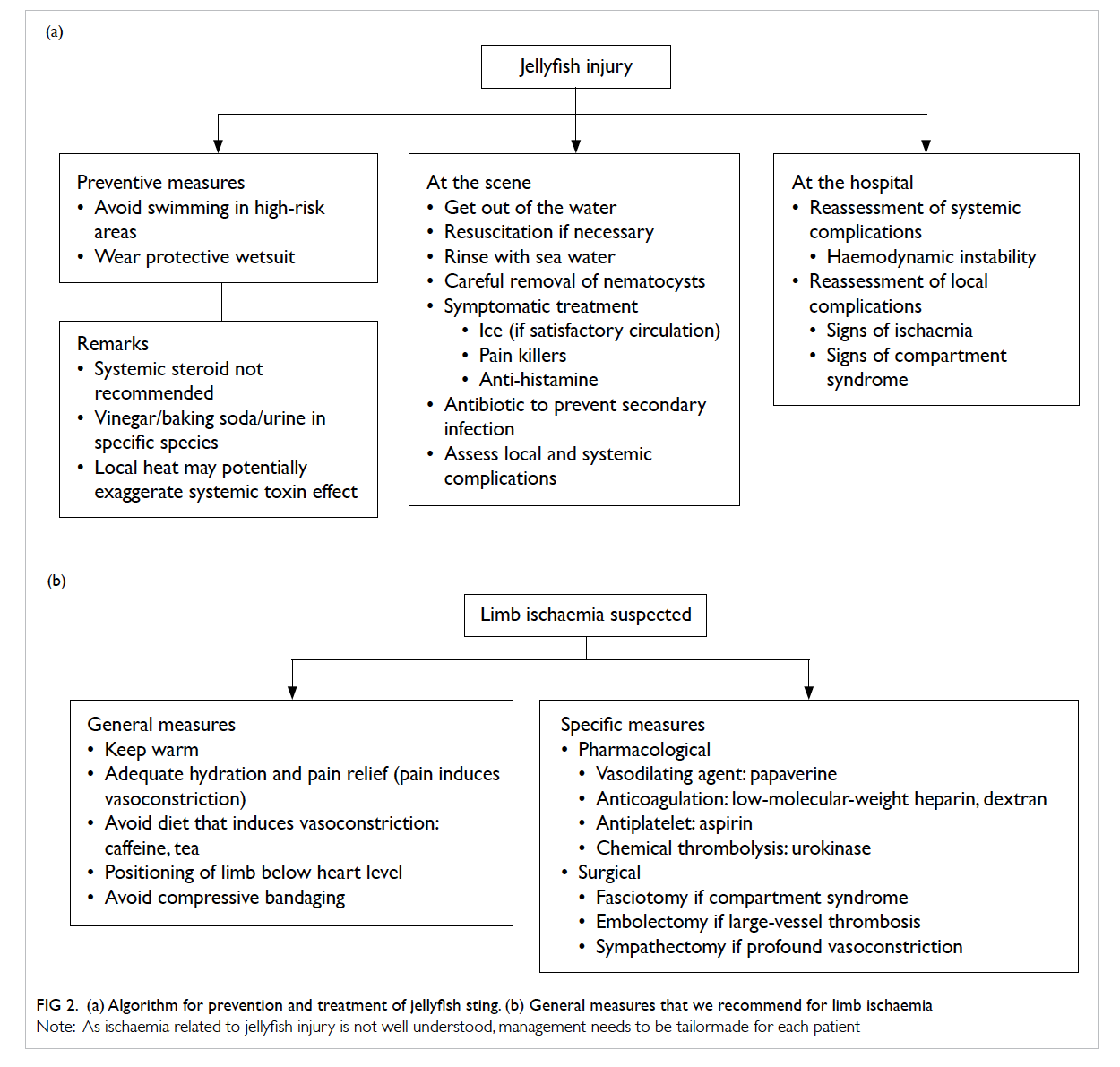
Figure 2. (a) Algorithm for prevention and treatment of jellyfish sting. (b) General measures that we recommend for limb ischaemia
Note: As ischaemia related to jellyfish injury is not well understood, management needs to be tailormade for each patient
The principles of the management of jellyfish
injury are:
(1) Best treatment remains prevention of injury
(2) Alleviate the local effect of venom (pain and
tissue damage)
(3) Prevent further discharge of nematocysts
(4) Control systemic reaction, including shock
Some important points need to be highlighted.
After rapid resuscitation, the next step is to remove
nematocysts, if technically feasible. It is also
important to note that popular home remedies such
as alcohol, physical rubbing by sand, or rinsing by
fresh water can actually worsen symptoms for the
victim, as these may lead to a massive nematocyst
discharge and toxin release. Another common folk
measure is the use of vinegar or urine to inactivate
the venom. Unfortunately, these two methods
are not applicable to all types of jellyfish stings as
different species have different toxins. We do not
recommend the general population to use either
vinegar or baking soda if the offending organism is
not well known.
Ice therapy is safe in general for pain relief due
to an unclear mechanism; whereas the application of
local heat is still debated, as it may potentially induce
vasodilation and a systemic toxic reaction rather
than denaturation of the venom. Anti-histamine
is generally safe for local symptom control and
antibiotics are also recommended for secondary
infection. There are no studies to support the use
of systemic corticosteroids in toxic reactions.8 Anti-venom
exists for a species of jellyfish called Chironex
fleckeri (sheep-derived whole immunoglobulin G).
However, it has unknown cardiotoxic effects and,
therefore, not approved or readily available.9
The underlying mechanism of local ischaemia
in our case was not well understood. Toxin- and
hypersensitivity-induced vasospasm and secondary
thrombosis are the postulated mechanisms. The
management algorithm in Figure 2b is based on this postulation. As there is no standardised management
in the literature, management should be tailored to
the patient and should balance the risks and benefits.
Further research is needed to confirm our postulation
and formulate a protocol for management of jellyfish
stings.
References
1. Brennan J. Jellyfish and other stingers. In: World Book’s
animals of the world. Chicago, IL: World Book, Inc;
2003.
2. Burnett JW, Calton GJ, Burnett HW. Jellyfish envenomation
syndromes. J Am Acad Dermatol 1986;14:100-6. CrossRef
3. Azuma H, Sekizaki S, Satoh A, Nakajima T, Ishikawa M.
Platelet aggregation caused by a partially purified jellyfish
toxin from Carybdea rastonii. Toxicon 1986;24:489-99. CrossRef
4. Chan YC, Tse ML, Lau FL. Hong Kong Poison Information
Centre: Annual Report 2010. Hong Kong J Emerg Medicine
2012;19:110-20.
5. Giordano AR, Vito L, Sardella PJ. Complication of a
Portuguese man-of-war envenomation to the foot: a case
report. J Foot Ankle Surg 2005;44:297-300. CrossRef
6. Drury JK, Noonan JD, Pollock JG, Reid WH. Jelly fish sting
with serious hand complications. Injury 1980;12:66-8. CrossRef
7. Abu-Nema T, Ayyash K, Wafaii IK, Al-Hassan J, Thulesius
O. Jellyfish sting resulting in severe hand ischaemia
successfully treated with intra-arterial urokinase. Injury
1988;19:294-6. CrossRef
8. Cegolon L, Heymann WC, Lange JH, Mastrangelo G.
Jellyfish stings and their management: a review. Mar Drugs
2013;11:523-50. CrossRef
9. Balhara KS, Stolbach A. Marine envenomations. Emerg
Med Clin North Am 2014;32:223-43. CrossRef

