Bringing light to the dark: an interview with Dr Cecilia Fan and her medical team
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
HEALTHCARE FOR SOCIETY
Bringing light to the dark: an interview with Dr Cecilia Fan and her medical team
Eric Choy1, Valerie Sophia Chung2
1 Year 4, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Year 4, The University of Hong Kong, Hong Kong SAR, China
When disaster strikes, the resilience of a community
is often measured by the dedication of those who
step forward to help. Among them are healthcare
professionals who extend their expertise beyond
the confines of hospitals and clinics, venturing
into the most challenging environments to provide
humanitarian aid. One such individual is Dr Cecilia
Fan, a consultant in family medicine with over 30
years of experience working in the Department
of Health. She then served in the Professional
Development and Quality Assurance Service,
overseeing families clinic services for government
employees and correctional medical services, and
operating quarantine centre medical posts during
major infectious disease outbreaks such as SARS,
swine flu, and coronavirus disease 2019. Dr Fan’s
unwavering dedication to humanitarian efforts
culminated in her leading the Department of Health
medical support team of the Hong Kong SAR Search
and Rescue Team to Türkiye in response to the 2023
Türkiye–Syria earthquake.
The Department of Health medical support
team, comprising two doctors and two nursing
officers, was deployed with the core mission of
supporting the health of frontline rescue workers.
Although many might assume such missions focus on
direct victim care, it is equally essential to ensure that
firefighters and rescue personnel remain physically
and mentally fit during their lifesaving operations.
Healthcare professionals in these settings act as the
backbone of operations, ensuring that those risking
their lives to save others are well cared for.
Their journey began with an arduous
deployment process, as flights could only be
confirmed at the last minute, requiring multiple
transfers before arriving in Hatay. Once on the
ground, the team travelled through damaged and
unlit roads, navigating a disaster-ravaged landscape
with limited supplies. Dr Kinson Lau, the other
doctor on the team, recalls, “It was pitch black,
the roads had no lights, and the driver had been
driving through the small hours without rest. Our
commander kept talking to him to keep him awake.”
Upon arrival, the team set up a tent as a medical
post on open ground riddled with cracks, to serve
the rescue forces. They conducted daily health
checks, monitoring vital signs and psychological
well-being. The nonstop travel and race-against-time
operation schedule led to fatigue among team
members, whereas the wide temperature range and
cold nights caused respiratory symptoms. Minor
injuries and skin conditions were common, and the
psychological stress of witnessing destruction and
death was immense. When one team member fell ill
with a high fever, the team had to assess the need to
isolate him to prevent the spread of infection. It was
decided that it would be more suitable to treat him
while ensuring his tent-mate wore a mask. Mr CF
Kwok, nursing officer of the team, stated, “He might
feel deserted if being isolated. Instead, we ensured
his tent-mate, who is caring and supportive, wore a
mask and took precautions.”
Another major challenge was maintaining
mental well-being. The emotional weight of witnessing destruction and loss took a toll on
everyone. There were shocking moments when the
team recovered deceased victims. Psychological
debriefing became an essential part of their routine,
allowing them to process their experiences and
support one another. “We saw families sitting in
front of collapsed buildings, waiting for news of their
loved ones, overflowing with a sense of helplessness.”
Despite this, the team found strength in each other
and in the moments when their work led to a
successful rescue.
Every deployment brings unique lessons,
and the mission in Türkiye was no exception. The
extreme cold posed unexpected difficulties, with
temperatures dropping below freezing at night.
With limited supplies, the team had to improvise
ways to stay warm, including using cardboard as
insulation and huddling around makeshift fires.
Clean water was scarce, making hygiene a challenge.
The team had to ration bottled water and adopted
innovative methods for sanitation, such as using
small amounts of disinfectant wipes for personal
hygiene. Mr Stephen Ngai, another nursing officer
on the team, mentioned, “Food, simply, was also
a concern.” Initially, the team relied on military
ration packs, which were practical but monotonous.
However, through collaboration with the China
Search and Rescue team, they were able to secure
hot meals, substantially boosting morale. Looking
ahead, Dr Fan advocates for better preparedness and
training programmes for medical support teams,
emphasising the need for psychological resilience
training and logistical pre-planning to enhance
efficiency in future deployments.
Amid these challenges, the team found
profound moments of impact, especially when the
first survivor was found on the fifth day. For Dr Fan,
it was incredibly rewarding to see the team’s efforts
come to fruition: “Eighty percent of the buildings
in the city collapsed. We walked through ruins,
knowing that buried beneath were people in dire
need of being found. The golden time for survival
might have been missed, but the team never gave up.
Pulling someone out alive after several days was a
feeling I will never forget.”
Dr Fan and her team embody the spirit of
selfless service, demonstrating that healthcare
professionals are not confined to hospitals and
clinics—they are essential pillars in disaster
response and humanitarian relief. Their work in
Türkiye serves as an inspiring example of how
medical expertise, adaptability, and teamwork
can make a life-saving difference in the most
challenging environments. As crises continue to
arise worldwide, their efforts remind us that the
true essence of medicine lies in its ability to serve
humanity, regardless of borders. The mission of
medical support teams is never just about treating injuries; it is about preserving the health, safety, and
dignity of those who put themselves at risk for the
sake of others.
The team’s efforts have led to lasting institutional
and societal impacts. Their experience served as
a catalyst for the formation of a dedicated medical
team within the Hospital Authority to support the
Fire Services Department’s Disaster Response and
Rescue Team in its efforts to obtain accreditation
from the International Search and Rescue Advisory
Group. This medical team, comprising orthopaedic
and emergency specialists and nurses, underwent
humanitarian training and exchange in Beijing,
equipping them with essential skills such as mass
casualty management, field amputations, and
high-stress resuscitation. Their contributions
have fortified Hong Kong’s capacity to respond to
future crises, while inspiring a broader cultural
shift towards valuing humanitarian medicine as a
professional imperative.
For Dr Fan, the motivation to engage in high-risk
humanitarian work transcends professional duty—it is a reaffirmation of medicine’s foundational
ethos: to serve where the need is greatest. She candidly
reflects on the medical, logistical, and emotional
challenges faced in Türkiye, from confronting the
limits of intervention in catastrophic settings to
navigating psychological stress. Yet, despite these
difficulties, Dr Fan and the team emphasised the
profound fulfilment of such missions. Their vision
for the future is clear: to help cultivate a generation
of medically trained humanitarians who are
technically proficient, psychologically prepared, and
ethically grounded. “When the call comes, answer
it,” she urges, framing humanitarian service not as
an extraordinary sacrifice but as a natural extension
of medical vocation—one that enriches both the
provider and the profession.
Dr Fan and the team’s story is one of
extraordinary resilience and commitment. Their
experiences in Türkiye reinforce the message that
humanitarian medical work is not just an act of
service—it is a duty that bridges borders and uplifts
humanity in its darkest hours.

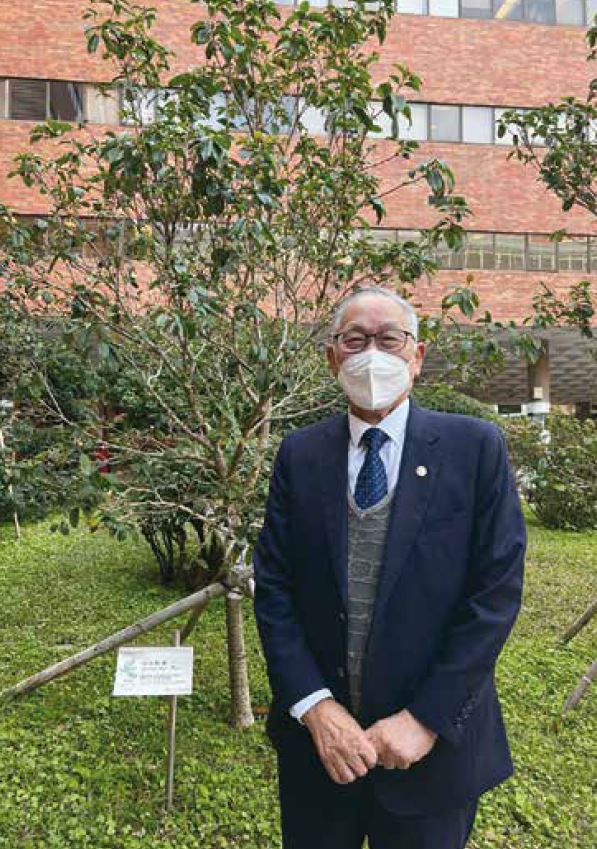
The Medical Support Team conducting daily health assessments during their humanitarian mission in Türkiye

(From left) Mr Stephen Ngai, Mr CF Kwok, Dr Kinson Lau, and Dr Cecilia Fan with student reporters, Valerie and Eric