Hong Kong Med J 2025;31:Epub 4 Jun 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Evaluation of the safety and efficacy of the Sentire Surgical System (C1000) for robot-assisted radical prostatectomy
CF Ng, MB, ChB, MD; CH Yee, MB, BS, MD; Peter KF Chiu, MB, ChB, PhD; Mandy HM Tam, MB, ChB, FHKAM (Surgery); Franco PT Lai, BN
SH Ho Urology Centre, Department of Surgery, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof CF Ng (ngcf@surgery.cuhk.edu.hk)
Abstract
Introduction: This prospective clinical study
evaluated the clinical safety and efficacy of the
Sentire Surgical System (C1000), a locally developed
robotic surgical platform, in performing radical
prostatectomy in Hong Kong.
Methods: This was a single-centre, single-arm study.
Adult patients with a clinical diagnosis of localised
prostate cancer planned for surgical treatment
were invited to participate. Surgery was performed
using the Sentire C1000 system following the
standard approach. The primary endpoints were the
conversion rate and the incidence of perioperative
complications within 30 days. Secondary outcomes,
including perioperative, pathological, oncological,
and functional outcomes at 1 month after surgery,
were also assessed.
Results: From August 2022 to September 2023,
20 patients were recruited. All procedures were
performed without conversion. There were no
intraoperative complications related to the robotic
device. Minor surgical complications (Grade I-II
according to the Clavien–Dindo Classification)
occurred in seven patients and were managed
conservatively. The mean total operative time was 184.5 minutes (standard deviation=30.0). The median
estimated blood loss was 175.0 mL (interquartile
range [IQR]=100.0-275.0). The median length of
hospital stay was 3.0 days (IQR=2.0-4.0). Seventeen
patients achieved undetectable levels of prostate-specific
antigen at 1 month after surgery.
Conclusion: These initial results support the
Sentire Surgical System (C1000), Hong Kong’s first
locally developed multidisciplinary surgical robotic
platform, as a safe and effective option for radical
prostatectomy, with clinical performance and
outcomes comparable to existing robotic systems.
New knowledge added by this study
- The first locally developed multidisciplinary surgical robotic system demonstrated safety and efficacy outcomes comparable to those of existing robotic systems.
- Initial clinical use in radical prostatectomy showed successful implementation, without conversion or device-related complications.
- This locally developed surgical robotic system may offer a more affordable option for locoregional institutes and allow more patients to benefit from robotic surgery.
- Wider adoption of locally developed systems could reduce reliance on monopolised international platforms and promote technological self-sufficiency in surgical care.
Introduction
Over the past few decades, the widespread adoption
of robotic surgical systems has revolutionised
surgical management, particularly for radical
prostatectomy.1 Enhanced visualisation, superior
dexterity, and tremor filtration enable surgeons to
maintain precision in the deep pelvis with better
ergonomics. These advantages contribute to lower
rates of positive surgical margins and biochemical
recurrence, thereby reducing the need for salvage therapy.2 Evidence also shows that robotic surgery can significantly reduce postoperative complications
and shorten the time to regain continence and
potency.3
For the past two decades, the global market for
robotic surgery has been dominated by the da Vinci
Surgical System (Intuitive Surgical, Sunnyvale [CA],
US). However, worldwide adoption of robotic surgery
remains limited by the high costs associated with
device acquisition, maintenance, and disposables. Consequently, access disparities persist worldwide,
particularly exacerbating inequities in surgical care4
in low- and middle-income countries.5 Surgeons and
trainees are also deprived of opportunities to acquire
robotic skills, creating a bottleneck in the clinical
application of advanced surgical technologies. To
address this problem, a novel, high-performing
yet affordable robotic surgical system is needed to
expand access to the highest standards of surgical
care.
The Sentire Surgical System (C1000) is a novel
robotic surgical system developed by Cornerstone
Robotics Limited (Hong Kong, China). It is the
first locally developed surgical robot designed for
multispecialty use. The system consists of three
interconnected components: a Patient-Side Robot
(PSR), a Surgeon Console, and a Vision Cart. The
PSR has four robotic arms, on which an endoscope
and up to three robotic surgical instruments can be
mounted. The endoscope provides a high-resolution,
three-dimensional image for the console surgeon.
An array of instruments, including graspers, needle
drivers, clip appliers, and scissors, can be installed
depending on the operational requirements. The
Surgeon Console includes two hand controls and
a set of foot pedals, enabling surgeons to operate
the surgical instruments and endoscope on the
PSR, while applying energy through the surgical
instruments. The Vision Cart includes a touchscreen display showing the endoscopic view for the assistant
surgeon. It houses the energy source for monopolar
and bipolar instruments, as well as the light and
camera source for the endoscope.
This study aimed to evaluate the clinical
safety and efficacy of the Sentire Surgical System by
reporting outcomes from the first clinical trial for
radical prostatectomy, as part of a multispecialty
clinical study. Comparable safety and patient
outcomes will provide supporting evidence for the
continued development of this robotic surgical
technology, facilitating its implementation and
evaluation in further clinical trials.
Methods
Study design
This was a prospective, single-centre, single-arm
study aligned with Stage 1 (Innovation) of the
IDEAL (Innovation, Development, Exploration,
Assessment, Long-term Study) framework.6 The
study formed part of a multi-speciality clinical
investigation to evaluate the safety and efficacy
of the Sentire Surgical System for robot-assisted
colorectal, upper gastrointestinal, and urological
surgery (radical prostatectomy).
Study population
From August 2022 to September 2023, 20 adult men
with clinically localised prostate cancer and planned
radical prostatectomy were recruited. The inclusion
criteria were: (1) age between 50 and 80 years; (2)
clinical diagnosis of non–metastatic prostate cancer;
(3) body mass index <35 kg/m2; (4) deemed suitable
for minimally invasive treatment; and (5) provision
of informed consent. Exclusion criteria were: (1)
contraindication to general anaesthesia; (2) prior
history of prostatic surgery; (3) untreated active
infection; (4) uncorrected coagulopathy; (5) presence
of other malignancies or distant metastases; and (6)
membership in a vulnerable population.
Surgical procedure
All 20 robot-assisted radical prostatectomies were
performed by four practising urological surgeons,
each with extensive experience (>50 prior cases
as chief surgeon). All participating surgeons had
been trained in the use of the system and had prior
experience performing procedures with the system
on cadaveric and live porcine models.
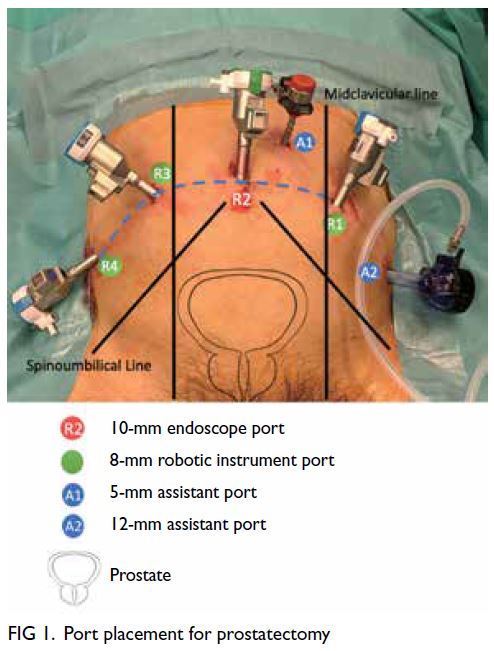
Patient and trocar positioning
Patients were placed under general anaesthesia in
the lithotomy position. A total of four robotic ports
were used. First, a 10-mm endoscope port was
placed supraumbilically through an open approach.
After pneumoperitoneum was established, three additional 8-mm robotic ports were inserted: one on
either side of the supraumbilical port, adjacent to the
left mid-clavicular line at approximately the vertical
level of the umbilicus, and one along the right or left
anterior axillary line, about 2 cm above the anterior
iliac spine. A 12-mm assistant port was inserted
opposite the most lateral robotic port, mirrored
across the midline. Finally, a 5-mm assistant port
was inserted between the midline and either the
right or left mid-clavicular line (on the same side as
the 12-mm assistant port) for suction and retraction
(Fig 1).
Docking
Following port placement, the patient was placed in
the Trendelenburg position. The PSR of the Sentire
Surgical System, which consists of four robotic arms
extending from a central column, was positioned
between the patient’s legs. Figure 2 shows photos of
the operating room during radical prostatectomy.

Figure 2. Intraoperative images of the Sentire Surgical System (C1000) during radical prostatectomy. (a) Robotic arms docked for the procedure. (b) Assistant surgeon position. (c) Surgeon Console. (d) Anaesthesiologist position
Instruments
For most radical prostatectomy procedures, a 0°
endoscope was used throughout. One surgeon
alternated among the 0°, 30° up (for initial bladder
detachment), and 30° down endoscopes (for bladder
neck dissection) according to their preference.
Bipolar Maryland Forceps (Cornerstone Robotics
Limited, Hong Kong SAR, China) were used in the
left hand, Monopolar Curved Scissors (Cornerstone
Robotics Limited, Hong Kong SAR, China) in the
right hand, and ExtraGrasp forceps (Cornerstone
Robotics Limited, Hong Kong SAR, China) on the
fourth robotic arm for traction. Left-hand and right-hand
instruments were exchanged for the Large
Needle Driver during vesicourethral anastomosis
and other suturing tasks. The right-hand instrument
could also be replaced with the Large Clip Applier
for vessel ligation.
Operation
Each operation was performed using the standard
transperitoneal anterior approach. Briefly, bladder
dissection was carried out in the areolar tissue plane
between the peritoneum and transversalis fascia
after the peritoneum had been incised at the lateral
borders of the urinary bladder. Dissection continued
caudally to develop the retropubic space. Preprostatic
fat was removed for enhanced anatomical
localisation. Dissection of the endopelvic fascia was
then performed. The dorsal venous complex was
ligated according to surgeon preference. Bladder
neck dissection followed, then dissection of the vas
deferens and seminal vesicles. The posterior plane
of the prostate was then dissected, continuing to
the prostatic apex. Lateral dissection was performed
next, with the degree of nerve sparing determined by preoperative erectile function, tumour location,
and tumour grade. Apical dissection was performed
and the urethra was then divided.
Haemostasis was secured by further suturing
of the dorsal venous complex, if not previously
completed. If indicated, pelvic lymph node dissection
was performed at this stage. Posterior Rocco’s
stitch reconstruction was carried out, followed by
vesicourethral anastomosis with continuous sutures.
After confirming watertightness, a pelvic drain was
placed via the most lateral robotic port. The robot
was then undocked and specimens were removed
in a specimen bag through an extended camera
port incision. Wounds were closed using standard
techniques.
Study endpoints
Primary endpoints included the conversion rate and
the incidence of perioperative complications within
30 days. Conversion was defined as an emergent
change to a conventional laparoscopic or open
approach. Intraoperative events and postoperative
complications during the hospital stay and within
30 days of discharge were recorded. The severity of
complications was graded according to the Clavien–Dindo Classification. Whether complications
were anticipated was determined based on their
consistency with the current investigational plan
or consent form. In the event of postoperative
complications, the relationship to the Sentire
Surgical System, the surgical procedure, and the patient’s underlying condition was documented,
along with actions taken and outcomes.
Secondary endpoints included perioperative
and pathological outcomes. Perioperative outcomes
included total operative time, docking time, total
console time, estimated blood loss, time to resume
regular activity, length of hospital stay, time of drain
and removal, time of urethral catheter removal,
visual analogue scale (VAS) pain scores at 14 and
30 days, and use of pads for urinary incontinence at
14 days and 30 days. Pathological outcomes included
surgical margins, lymph node metastasis, tumour
involvement, pathological tumour stage, number of
lymph nodes harvested, and postoperative prostate-specific
antigen (PSA) level.
Statistical analyses
Data are presented in a descriptive manner.
Continuous variables are reported as means
with standard deviations (SDs) or medians with
interquartile ranges, whereas categorical variables
are presented as percentages. All analyses were
performed using SPSS (Windows version 25.0; IBM
Corp, Armonk [NY], US).
Results
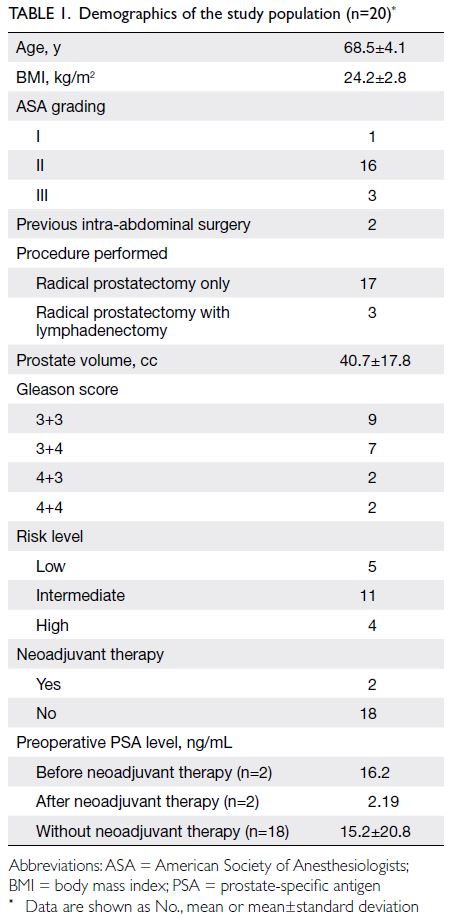
Twenty patients were enrolled in the trial, and
all successfully underwent robot-assisted radical
prostatectomy using the Sentire Surgical System. The
mean age was 68.5 years (SD=4.1) and the mean body
mass index was 24.2 kg/m2 (SD=2.8). Two patients
had a history of abdominal surgery: Case 3 had
undergone open appendicectomy, and Case 11 had
undergone laparoscopic cholecystectomy. Seventeen
patients underwent radical prostatectomy only, while
three also underwent lymphadenectomy. The mean
prostate volume was 40.7 cc (SD=17.8). Nine patients
had a Gleason score of 6, nine had a score of 7, and
two had a score of 8. Five patients were classified as
low-risk, 11 as intermediate-risk, and four as high-risk.
Two patients received neoadjuvant hormonal
therapy due to concerns about prolonged waiting
times during the coronavirus disease 2019 period;
their mean initial PSA level dropped from 16.2 ng/mL
to 2.19 ng/mL. The mean preoperative PSA level for
patients who did not receive neoadjuvant therapy
was 15.2 ng/mL (SD=20.8) [Table 1].
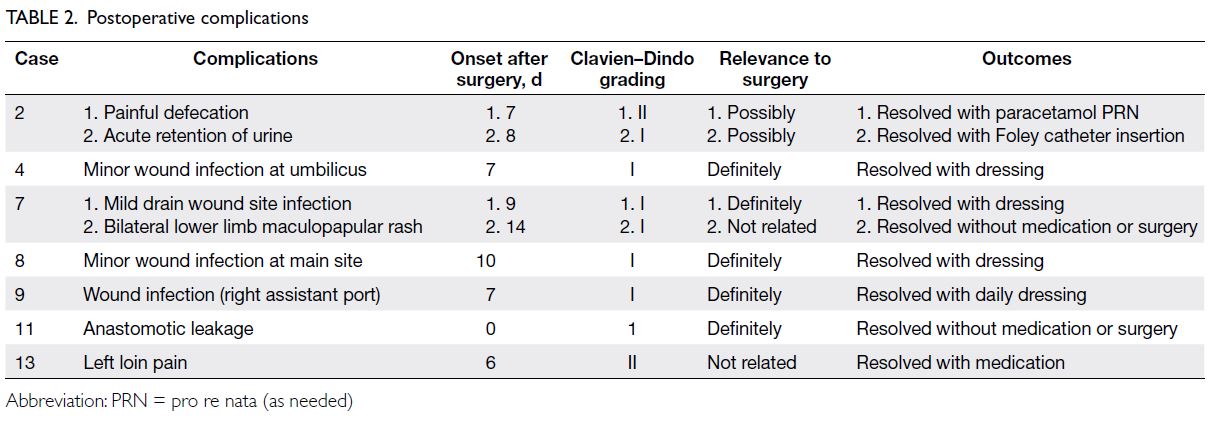
All operations were completed without
conversion. There were no intraoperative complications related to the robotic device. Minor
surgical complications (Grade I-II) occurred in seven
patients, including four cases of wound infection,
one case of urinary retention, one case of prolonged
anastomotic leakage, one case of bilateral lower
limb rash, and one case of left loin pain. Only five of
these complications—namely wound infections and
prolonged anastomotic leakage—were considered
related to the surgery (Table 2).
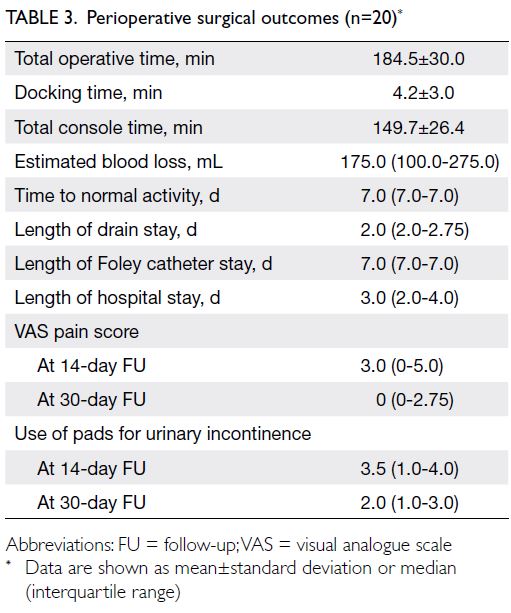
The mean total operative time (from skin
incision to closure) was 184.5 minutes, including a
mean docking time of 4.2 minutes and a mean total
console time of 149.7 minutes. The median estimated
blood loss was 175.0 mL. Postoperatively, the median
time to resumption of regular activity was 7.0 days,
the median duration of drainage was 2.0 days and
the median duration of urethral catheterisation was
7.0 days. The median length of hospital stay was
3.0 days. The median VAS pain score at the 14-day
follow-up was 3.0, whereas at the 30-day follow-up it
was 0. Pad usage for urinary incontinence was 3.5 at
the 14-day follow-up and 2.0 at the 30-day follow-up
(Table 3).
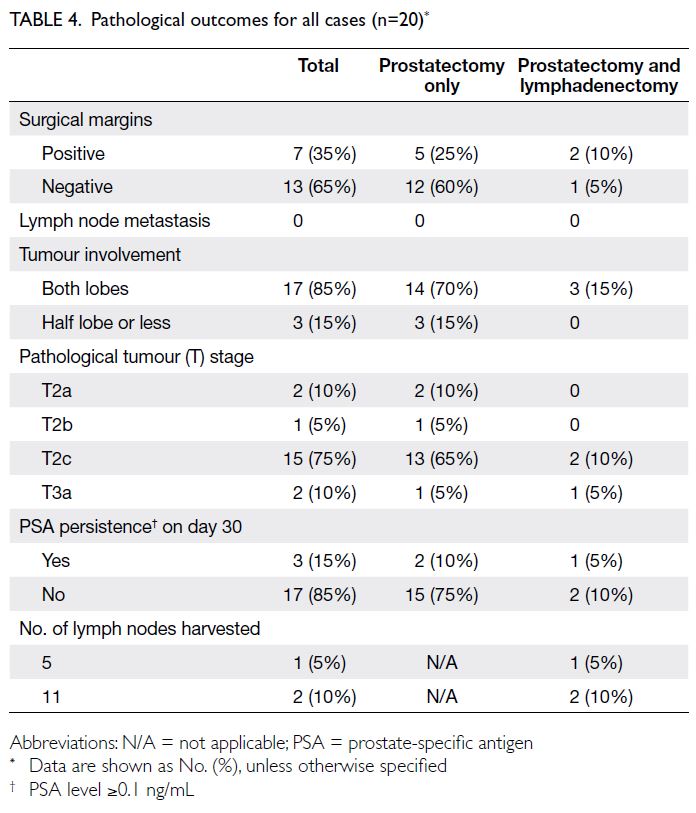
Regarding pathological outcomes, 13 of the
20 patients (65%) had negative surgical margins,
including the two who received neoadjuvant
hormonal therapy. Seventeen patients (85%) had
undetectable PSA levels 1 month after surgery, while
two other patients (95%) achieved undetectable
levels at 3 months. Among the three patients who
underwent lymphadenectomy, the mean number of
lymph nodes harvested was 9 (range=5-11) [Table 4].
Discussion
This prospective study reports the results of the
first-in-human clinical trial of the Sentire Surgical
System—the first locally developed multispecialty surgical robot—used for radical prostatectomy. All
20 procedures were completed successfully, without
conversions and device-related intraoperative or
postoperative complications, demonstrating that
this novel surgical system is safe and effective for
robot-assisted radical prostatectomy.
Since the introduction of robotic surgery in
Hong Kong in 2005, its use—particularly in urology—has steadily expanded.7 According to the latest
Surgical Outcome Monitoring and Improvement
Programme report (2022-2023), almost all
radical prostatectomies (409 of 410 patients) were
performed using robotic surgery.8 Improved
outcomes have been a key factor supporting its
development.9 However, the high cost of robotic
systems considerably limits further expansion
and popularisation. With the expiration of certain
technological patents, new robotic systems are
rapidly emerging worldwide.10 The development
of a locally based robotic system in Hong Kong
represents an important milestone for the future of
robotic surgery in the region.
Perioperative outcomes in this trial were
favourable, with a mean total operative time of
184.5 minutes, comparable to reported times in the
existing literature on both laparoscopic and robotic
radical prostatectomy.11 The short docking time
reflected a smooth docking process. Most cases
had acceptable blood loss, and no patients required
transfusion, again comparable to the literature.11
Despite the higher-than-expected wound infection
rate, most infections were minor and managed with
simple dressing. No specific cause was identified,
and these events are unlikely to be related to the
robotic system. Postoperative hospital stay was
also short, with satisfactorily low VAS pain scores.
Early functional outcomes, specifically pad usage for
urinary incontinence, were also satisfactory (Table 3).
Short-term oncological outcomes also support
the system’s efficacy, such that 65% of patients
achieved a negative surgical margin and 85% and
95% of patients showed no PSA persistence (PSA
level ≥0.1 ng/mL) at 30 days and 3 months after
surgery, respectively—results that are comparable
to the literature.12 In the three cases where
lymphadenectomy was performed, the mean lymph
node yield was 9, which is considered optimal for
balancing the biochemical recurrence-free rate and
complication risk.13 These findings indicate that the
system can achieve oncological outcomes in radical
prostatectomy comparable to those of established
robotic systems.
Compared with our previously reported
outcomes using other robotic systems,14 the
performance of the current system was highly
comparable. The mean operative time and hospital stay were 184.5 minutes/3.1 days (Sentire C1000),
225.8 minutes/3.3 days,14 (da Vinci S), and 223.7 minutes/3.0 days,14 (da Vinci SP). These results not
only demonstrate that the Sentire C1000 offers
performance comparable to existing robotic systems
but also confirm the ease of surgical transition. A key
factor enabling this transition is the similarity of the
robotic control interface—including hand controls
and foot pedals, allowing surgeons to adopt the new
system more readily and apply their existing robotic
experience. This is akin to driving different brands of
cars, where consistent interfaces such as the steering
wheel and pedals enable smooth adaptation. As
a result, most new robotic systems adopt similar
interface designs to support seamless integration
by experienced surgeons. Moreover, the PSR has a
similar arm configuration and setup to the da Vinci
system, which also helps both surgeons and nursing
staff adapt to the setup.
As this is the initial report of the Sentire Surgical
System’s clinical use in radical prostatectomy,
further clinical studies are warranted to evaluate its
performance across a broader range of procedures.
Conclusion
Our findings indicate that the Sentire Surgical System
(C1000) is a safe and effective robotic platform for
radical prostatectomy. Its successful performance
in this first-in-human experience supports ongoing
development and broader application of this novel
surgical robotic system.
Author contributions
Concept or design: CF Ng.
Acquisition of data: CH Yee, PKF Chiu, MHM Tam, FPT Lai.
Analysis or interpretation of data: FPF Lai.
Drafting of the manuscript: CF Ng, FPF Lai.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: CH Yee, PKF Chiu, MHM Tam, FPT Lai.
Analysis or interpretation of data: FPF Lai.
Drafting of the manuscript: CF Ng, FPF Lai.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, CF Ng was not involved in the peer review process. Other authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank the support from the operating theatre staff in Prince of Wales Hospital.
Funding/support
The research was supported by Cornerstone Robotics Limited for equipment and research fund. The funder had no role in the study design, data collection/analysis/interpretation, or manuscript preparation.
Ethics approval
The research was approved by the Joint Chinese University
of Hong Kong—New Territories East Cluster Clinical
Research Ethics Committee, Hong Kong (Ref No.: CREC
2021.472). It was registered on www.ClinicalTrials.gov (Ref
No.: NCT05151835). Written informed consent was obtained
from all patients for the publication of this research and the
accompanying images.
References
1. Ng AT, Tam PC. Current status of robot-assisted surgery.
Hong Kong Med J 2014;20:241-50. Crossref
2. Okegawa T, Omura S, Samejima M, et al. Laparoscopic
radical prostatectomy versus robot-assisted radical
prostatectomy: comparison of oncological outcomes at a
single center. Prostate Int 2020;8:16-21. Crossref
3. Allan C, Ilic D. Laparoscopic versus robotic-assisted radical
prostatectomy for the treatment of localised prostate
cancer: a systematic review. Urol Int 2016;96:373-8. Crossref
4. Bansal E, Kunaprayoon S, Zhang LP. Opportunities
for global health diplomacy in transnational robotic
telesurgery. AMA J Ethics 2023;25:E624-36. Crossref
5. Mehta A, Cheng Ng J, Andrew Awuah W, et al. Embracing
robotic surgery in low- and middle-income countries:
potential benefits, challenges, and scope in the future. Ann
Med Surg (Lond) 2022;84:104803. Crossref
6. IDEAL Collaboration. The IDEAL Framework. Available from: https://www.ideal-collaboration.net/the-ideal-framework/. Accessed 26 May 2025.
7. Chan SY, Hou SM, Wong WS, Ng CF. Robotic urological surgery: prospects for Hong Kong. Surg Pract 2007;11:154-8. Crossref
8. Surgical Outcomes Monitoring and Improvement
Programme (SOMIP) report. Volume Fifteen: July
2022—June 2023. Hospital Authority, Hoong Kong SAR
Government; 2024.
9. Lo KL, Ng CF, Lam CN, Hou SS, To KF, Yip SK. Short-term
outcome of patients with robot-assisted versus open
radical prostatectomy: for localised carcinoma of prostate.
Hong Kong Med J 2010;16:31-5.
10. Marchegiani F, Siragusa L, Zadoroznyj A, et al. New
robotic platforms in general surgery: what’s the current
clinical scenario? Medicina (Kaunas) 2023;59:1264. Crossref
11. Novara G, Ficarra V, Rosen RC, et al. Systematic review
and meta-analysis of perioperative outcomes and
complications after robot-assisted radical prostatectomy.
Eur Urol 2012;62:431-52. Crossref
12. Wu S, Lin SX, Cornejo KM, et al. Clinicopathological and
oncological significance of persistent prostate-specific
antigen after radical prostatectomy: a systematic review
and meta-analysis. Asian J Urol 2023;10:317-28. Crossref
13. Zhang X, Zhang G, Wang J, Bi J. Different lymph node
dissection ranges during radical prostatectomy for patients
with prostate cancer: a systematic review and network
meta-analysis. World J Surg Oncol 2023;21:80. Crossref
14. Ng CF, Teoh JY, Chiu PK, et al. Robot-assisted single-port
radical prostatectomy: a phase 1 clinical study. Int J Urol
2019;26:878-83. Crossref