Hong Kong Med J 2023 Aug;29(4):311–21 | Epub 3 Aug 2023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Cross-cultural translation into Chinese and psychometric evaluation of a screening tool for nocturia: the Targeting the individual’s Aetiology of Nocturia to Guide Outcomes (TANGO) questionnaire
Steffi KK Yuen, MB, BS, FRCSEd (Urol); Wendy Bower, FACP, PhD; CF Ng, MB, ChB, MD; Peter KF Chiu, MB, ChB, PhD (Erasmus); Jeremy YC Teoh, MB, BS, FRCSEd (Urol); Crystal SY Li, MBA (HSM); Hilda SW Kwok, MNurs; CK Chan, MB, ChB, FRCSEd (Urol); Simon SM Hou, MB, BS, FRCSEd (Urol)
SH Ho Urology Centre, Division of Urology, Department of Surgery, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof CF Ng (ngcf@surgery.cuhk.edu.hk)
Abstract
Introduction: We conducted translation and psychometric validation of a self-administered, 22-item dichotomous response–based questionnaire to identify nocturia aetiologies and co-morbidities in adult patients.
Methods: The Targeting the individual’s Aetiology
of Nocturia to Guide Outcomes (TANGO)
questionnaire was forward- and backward-translated,
then finalised using a standardised
methodology. The resulting version, a Chinese
version of the TANGO [TANGO (CV)], was
evaluated for internal consistency, test-retest
reliability, content validity, convergent validity,
criterion validity, and discriminant validity via
responses from 65 participants (46 men and 19
women; mean age, 67 years, range, 50-88), in
comparison with other validated questionnaires and
a 4-day bladder/sleep diary.
Results: Only 0.4% of responses were missing;
3% of participants required assistance with
comprehension. The Kuder–Richardson Formula
20 (KR-20) coefficient for the whole tool was
0.711. Kappa values for individual domains and the
whole tool varied from 0.871 to 0.866, indicating
satisfactory test-retest reliability. There was strong
agreement between the sum of positive responses
to each domain and the whole tool (intra-class
correlation coefficient=0.878-1.000). Modest
correlations (ρ=0.4-0.6) were detected between the
tool and bladder/sleep diary–based parameters for convergent validity. Criterion validity was confirmed
for each domain and the whole tool [ρ=0.287-0.687]. In receiver operating characteristic analysis,
the tool could distinguish patients (≥2 nocturia
episodes/night) from controls (≤1 nocturia episode/night) [Youden’s J statistic=0.453, area under the
curve=0.818, 95% confidence interval (CI)=0.683-0.953] and patients with significant nocturia distress
from patients with mild nocturia distress (Youden’s
J statistic=0.398, area under the curve=0.729,
95% CI=0.581-0.878).
Conclusion: The TANGO (CV) was formally cross-culturally adapted and translated. Its psychometric properties (except sensitivity to change) were validated.
New knowledge added by this study
- A Chinese version of the Targeting the individual’s Aetiology of Nocturia to Guide Outcomes questionnaire, a tool to screen for nocturia aetiologies and co-morbidities, has been validated.
- The tool can be understood by patients without substantial assistance from medical staff.
- The tool can distinguish patients with significant nocturia distress from patients with mild nocturia distress.
- The tool can be self-administered and used by multiple specialties in the treatment of patients with nocturia distress.
- The aetiologies contributing to nocturia can be rapidly identified.
- Patients can receive earlier referral to the appropriate teams/specialties to manage the underlying causes of nocturia.
Introduction
A recent population survey in Hong Kong showed
that 68% of men and 67% of women aged >40
years seeking medical advice for lower urinary
tract symptoms (LUTS) had ≥2 nocturia episodes/night1; these prevalences are greater than that
among individuals of similar age reported in other
global studies.2 Across urology clinics in Southeast
Asian countries, nocturia has emerged as the most
common presenting symptom (up to 88%) among
men with LUTS requiring treatment3; however, at
least half of these patients were dissatisfied with the
results of treatment.4
Nocturia is no longer considered a distinct
urologic disease.5 Indeed, it is related to disorders
within and outside the lower urinary tract, which
are associated with diminished bladder capacity,
increased rate and volume of nocturnal urine
production, sleep disturbance, or a combination of
these symptoms.6 Thus, initial treatment is difficult
and there is a need for a tool that captures relevant aetiological information earlier in the diagnostic pathway.
The short form of the Targeting the individual’s
Aetiology of Nocturia to Guide Outcomes (TANGO)
is a recently developed, 22-item, dichotomous-choice,
multi-dimensional, self-administered
questionnaire in English with robust psychometric
properties.7 8 This questionnaire covers four thematic
areas regarding aetiologies and co-morbidities
related to nocturia: cardiovascular or metabolic
disorders, sleep/nocturnal pain/apnoea variables,
urinary tract symptoms, and mental health and well-being
(including falls). This study was performed
to translate and cross-culturally adapt the TANGO
into Chinese, ie, to produce a Chinese version of the
TANGO [TANGO (CV)], then evaluate its reliability
and validity for use in Hong Kong.
Methods
Phase I: linguistic translation
We adopted the cross-cultural translation
methodology described by Sperber9 and
recommended by the original authors of the
TANGO.7 Six independent bilingual translators
were asked to produce six forward translations (in
Chinese) of each item of the TANGO, with the goal
of conceptual translation; all six forward translations
were back-translated to English, yielding six back-translations.
The six back-translations (in English) were
reviewed by a panel of urologists (n=4), urology
nurse specialists (n=2), and staff without a medical
background (n=2) who were not involved in
conducting this study, to produce a preliminary
draft of each item in the translated tool. Each item
in the English back-translations was compared with
the original English version by ranking in terms
of language comparability and the interpretation
similarity using a Likert scale from 1 (extremely
comparable/similar) to 7 (not at all comparable/similar). Items from the back-translations with
a mean score <2.50 were retained. The forward
translations (Chinese) of the retained back-translated
English items were reviewed and compared in a
panel consensus meeting comprising four urologists,
two urology nurse specialists, and two bilingual
translators. These items were used to draft the final
version of the translated tool, the TANGO (CV).
Phase II: psychometric evaluation
After linguistic translation, a prospective
psychometric evaluation study was conducted. From
December 2019 to March 2020, we recruited male
and female patients aged 45 to 90 years who presented
to the urology clinic for management of LUTS
problems and with self-reported nocturia episodes
of ≥2 per night as patient group. Exclusion criteria were a history of prostatic surgery and/or prostate
cancer, as well as the presence of active urinary
tract infection, active cancer receiving treatment,
bladder stone, neuropathic bladder, dependent daily
activities (including feeding, bathing, and walking
with assistance), diabetes insipidus, renal failure,
pregnancy, and/or illiteracy. Healthy individuals of
similar age with self-reported nocturia episode of ≤1
per night were recruited as controls.
After recruitment, participants completed
the TANGO (CV), the Chinese version of the
International Prostate Symptom Score (IPSS),10
the International Consultation on Incontinence
Questionnaire Nocturia module (ICIQ-N),11 the
Nocturia-Specific Quality-of-Life Questionnaire
(NQoL),12 the Hong Kong Chinese version of the
Overactive Bladder Symptom Score (OABSS-HKC)
questionnaire,13 the Epworth Sleepiness Scale (ESS),14 and the Chinese version of the STOP-Bang
questionnaire.15 Participants underwent assessment
of their histories of hypertension, diabetes mellitus,
hyperlipidaemia, cerebrovascular accident,
ischaemic heart disease, peripheral oedema, and
obstructive sleep apnoea; their responses were
cross-checked with the diagnostic codes of the
central registry and their previous medical records.
Blood glucose, glycated haemoglobin (HbA1c), and
estimated glomerular filtration rate were measured.
Participants were also given bladder/sleep diaries to
record the time and volume of each voiding event,
along with their sleep information (times of going to
bed, falling asleep, awakening from sleep, and rising
from bed), for 4 consecutive days at home within 2
weeks after recruitment. Participants then returned
the bladder/sleep diaries to the clinic and repeated
the TANGO (CV).
Reliability and validity
Reliability (inter-item correlation) was determined by internal consistency based on the Kuder–Richardson
Formula 20 (KR-20) coefficient, which is specifically
designed for dichotomous-choice questionnaires.16
Test-retest reliability was determined using Cohen’s
kappa value (κ) and the intra-class correlation
coefficient (ICC) by comparing the agreement of
repeat responses for each item and the congruency of
the number of positive responses to the tool between
recruitment and follow-up (2 weeks later). κ≥0.4 and
ICC ≥0.7 were considered acceptable reliability.17
We examined content validity by assessing the
level of missing data, which indicated acceptability
and difficulty in terms of participant understanding
of items within the tool. Construct validity, which
reflects the theory underlying nocturia, was
evaluated by comparing the number of the positive
responses to each of the four domains and all four
domains of the TANGO (CV) with data regarding
bladder/sleep diary–based parameters, as follows:
- Cardiovascular/metabolic domain (Questions 1-7) was compared with the bladder diary (nocturia episodes, rate and volume of nocturnal urine output between falling asleep and awakening, and nocturnal polyuria index);
- Sleep-related domain (Questions 8-13) was compared with the bladder diary [sleeping time, sleep latency, sleep quality, and degree of vitality after sleep, using a scale from 0 (the worst) to 10 (the best)];
- LUTS domain (Questions 14-18) was compared with the bladder diary as in (1);
- General well-being domain (Questions 19-22) was compared with the bladder diary as in (2);
- The whole tool (all four domains, Questions 1-22) was compared with the abovementioned parameters.
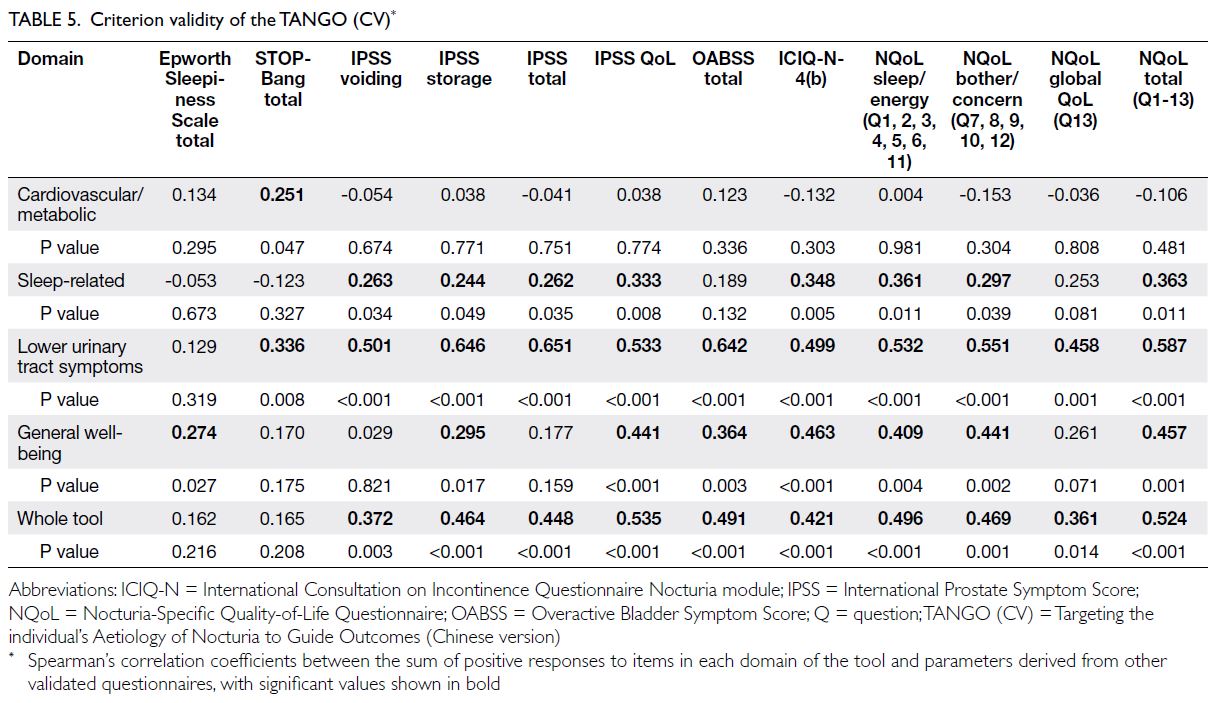
Criterion validity was estimated by comparing
the number of the positive responses to each of the
four domains and all four domains with the responses
to items on other questionnaires evaluating similar
constructs, as follows:
- Cardiovascular/metabolic domain was compared with ESS, STOP-Bang questionnaire, ICIQ-N-4(b) and NQoL sleep/energy domain, NQoL bother/concern domain, NQoL global QoL domain, and total score of NQoL;
- Sleep-related domain was compared with ESS, STOP-Bang questionnaire, ICIQ-N-4(b), and NQoL;
- LUTS domain was compared with IPSS voiding (sum of scores of Questions 1, 3, 5, and 6), IPSS storage (sum of scores of Questions 2, 4, and 7), ICIQ-N-4(b), OABSS (total), and NQoL;
- General well-being domain was compared with IPSS QoL, NQoL sleep/energy domain, NQoL bother/concern domain, NQoL global QoL domain, and total score of NQoL.
We assumed that a correlation coefficient
ρ≥0.4 was moderate and acceptable18 as evidence of
construct/criterion validity.
For discriminant validity, receiver operating
characteristic analysis, in combination with
Youden’s J statistic [ie, sensitivity–(1-specificity)],
was performed to explore whether the sum of
positive responses to the whole tool could be used
to distinguish: (1) patients from controls; and (2)
patients with significant nocturia distress from
patients with mild nocturia distress (Question 12 of
NQoL).
Sample size calculation
Assuming a type I error (α) of 0.05 and type II error (1-β) of 0.8, we calculated that:
Assuming an attrition rate of 20%,
approximately 60 participants (patients and controls) were needed.
Statistical analysis
Continuous data were reported as mean and standard
deviation or median and range. Categorical data
were described using frequencies and percentages.
For comparisons of continuous data, Student’s t test or the Mann-Whitney U test was used, depending on
the data distribution; for comparisons of categorical
data, the Pearson Chi squared test or Fisher’s exact
test was used. The Spearman’s correlation coefficient
was used to assess associations between parametric
or ordinal data and continuous data with a skewed
distribution; the Pearson correlation coefficient
was used to assess associations between normally
distributed continuous data. SPSS Statistics
(Windows version 26.0; IBM Corp, Armonk [NY],
United States) was used for data analysis. P values
<0.05 were considered statistically significant.
Results
Linguistic validation
Comparability scores for each item in the TANGO
(CV) ranged from 1.38 (0.52) to 2.25 (1.28), with an
overall mean score of 1.70 (0.88). Similarity scores for
each item ranged from 1.00 (0.52) to 2.13 (1.36), with
an overall mean score of 1.63 (0.88). The TANGO
(CV) is shown in the online supplementary Table.
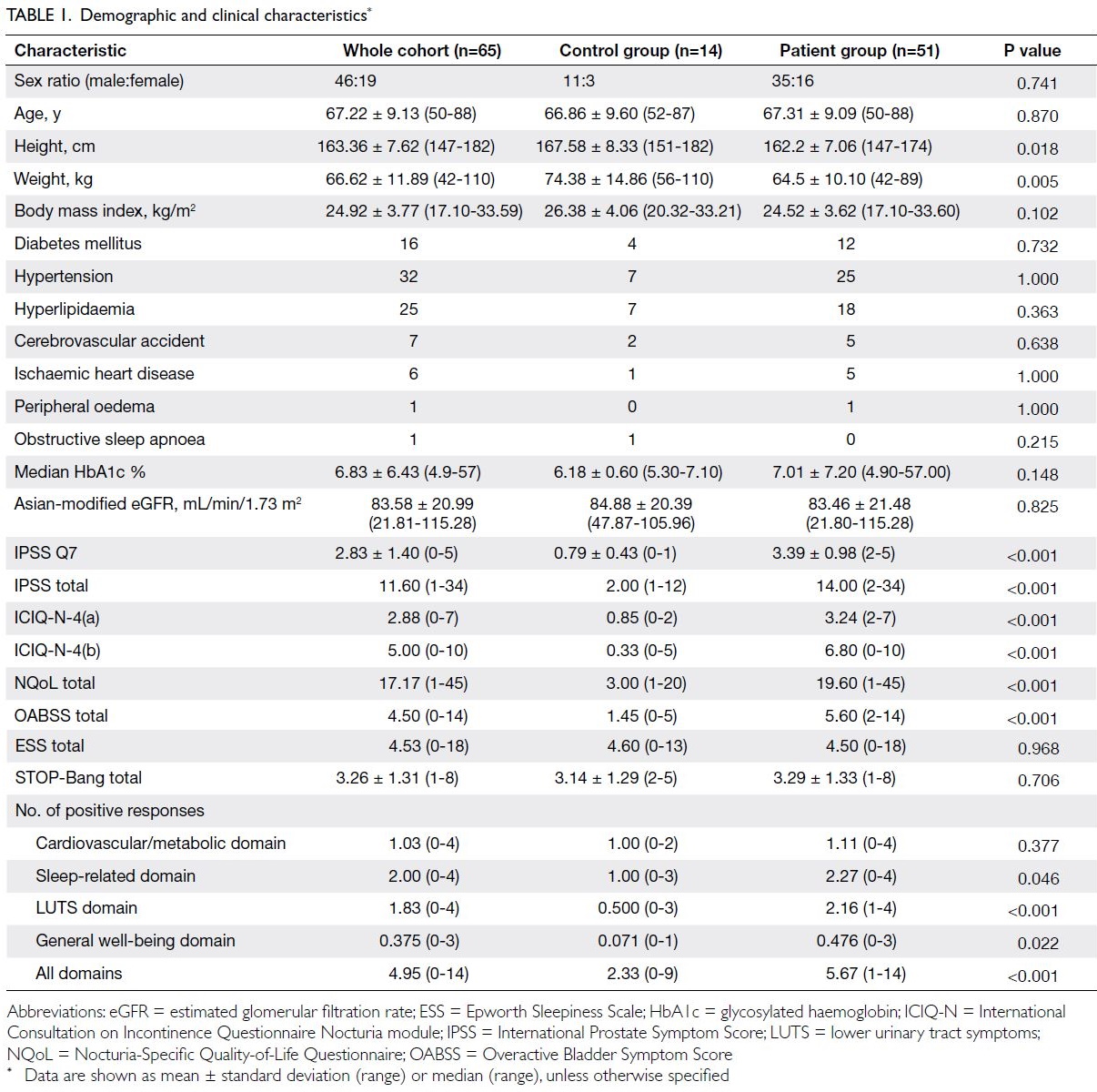
Demographic data and patient responses to
the items
This study included 65 participants, which include
51 (78.5%) patients (mean age: 67 years; 35 men, 16
women) with mean self-reported nocturia episodes
of 3.39 per night (standard deviation=0.98; range,
2-5) and 14 (21.5%) controls (mean age: 67 years;
11 men, three women) with mean self-reported
nocturia episodes of 0.79 per night (standard
deviation=0.43, range, 0-1). The demographic
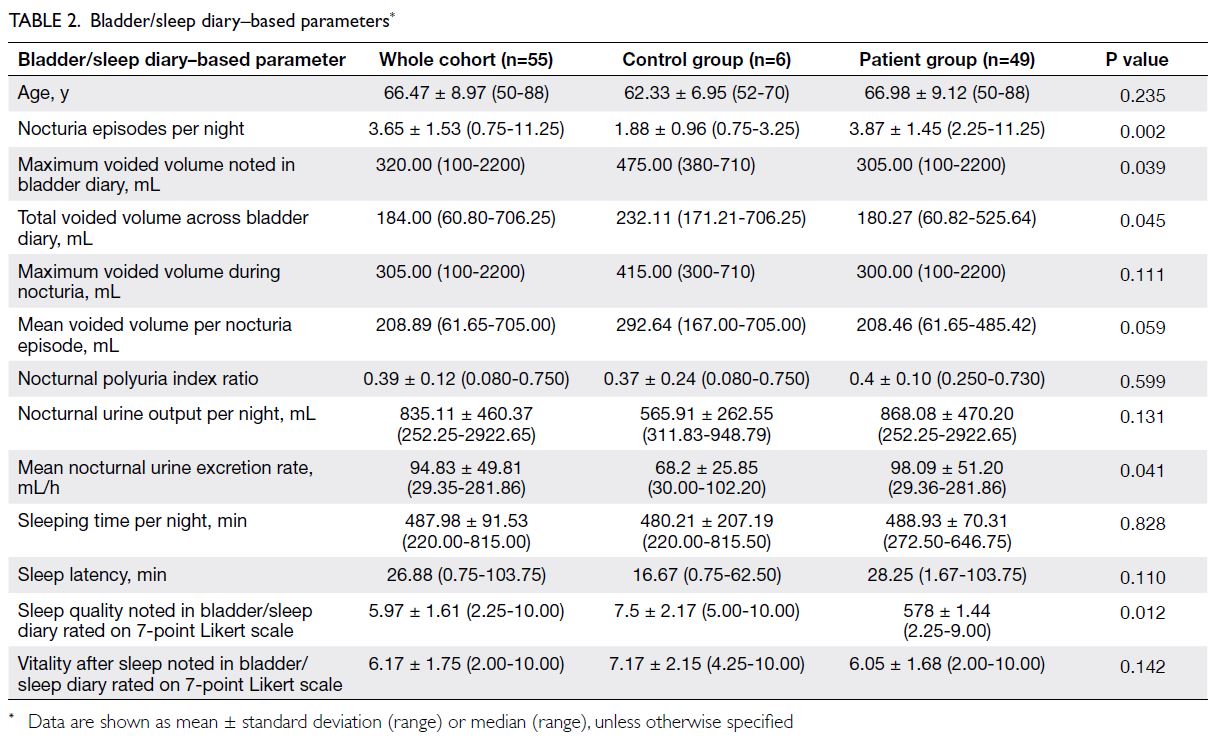
and baseline clinical characteristics are shown in
Table 1; the bladder/sleep diary–based parameter data are shown in Table 2. The control group had
fewer positive responses (median=2.33) to items
in the TANGO (CV), less nocturia distress, higher
functional bladder capacity during daytime and
night-time, and a lower nocturnal urine excretion
rate; however, control participants reported similar
prevalences of medical conditions that could cause nocturia, compared with patients who experienced
≥2 nocturia episodes/night.
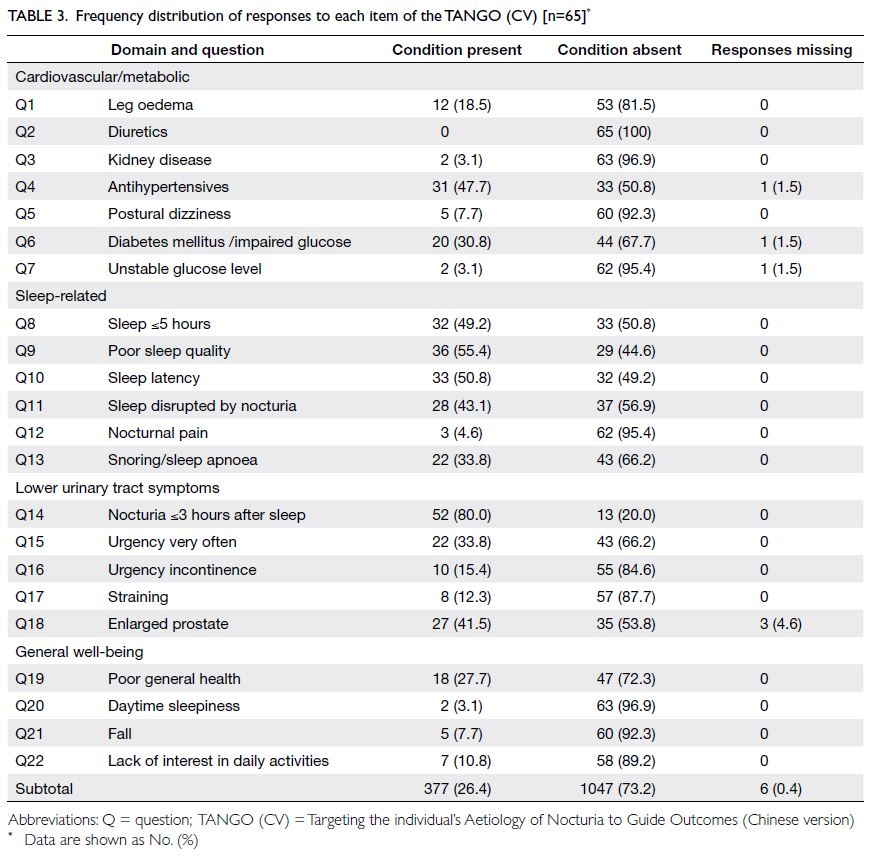
All 65 participants reported that the questions
in the tool were clearly presented, and they answered
99.6% of the items in the tool (total items=22 × 65=1430). Two (3%) participants required assistance
with comprehension to complete the TANGO (CV).
Missing responses were noted for items related to
the use of antihypertensives (n=1), the diagnosis
of diabetes mellitus/impaired glucose level (n=1),
and unstable glucose level (n=1); three men were
unable to respond to the question concerning
prostate enlargement [Table 3]. In total, 41 (63%)
participants reported at least one positive response
(total responses=72) in the cardiovascular/metabolic
domain, 48 (74%) participants reported at least one
positive response (total responses=154) in the sleep-related
domain, 54 (83%) participants reported at
least one positive response (total responses=119) in
the LUTS domain, and 21 (32%) participants reported
at least one positive response (total responses=32) in
the general well-being domain. The item with most
positive responses was nocturia within 3 hours after
going to bed (80% of participants) and the item with
the fewest positive responses was the use of diuretics
(0 responses) [Table 3]. Among the four thematic
areas, 90% of participants had positive responses
to ≥1 domain. Only three (6%) of the 51 patients
with ≥2 nocturia episodes/night exhibited nocturia-related problems that were limited to a single domain.
Internal consistency and test-retest reliability
The KR-20 coefficients of the four domains of the
TANGO (CV) were 0.354-0.615 (best in sleep-related
and general well-being domains; worst in
cardiovascular/metabolic domain), suggestive of
fair to moderate subscale internal consistency. For
the whole tool, the KR-20 coefficient was 0.711
(ie, >0.700), indicating satisfactory overall internal
consistency. Kappa values were between 0.817 and
0.871 for items in each of the four domains and
0.866 for the whole tool, whereas ICCs were between
0.878 and 1.000 for the subtotal positive responses
in each of the four domains and 0.972 for the whole
tool; these findings indicated near-perfect test-retest
reliability.
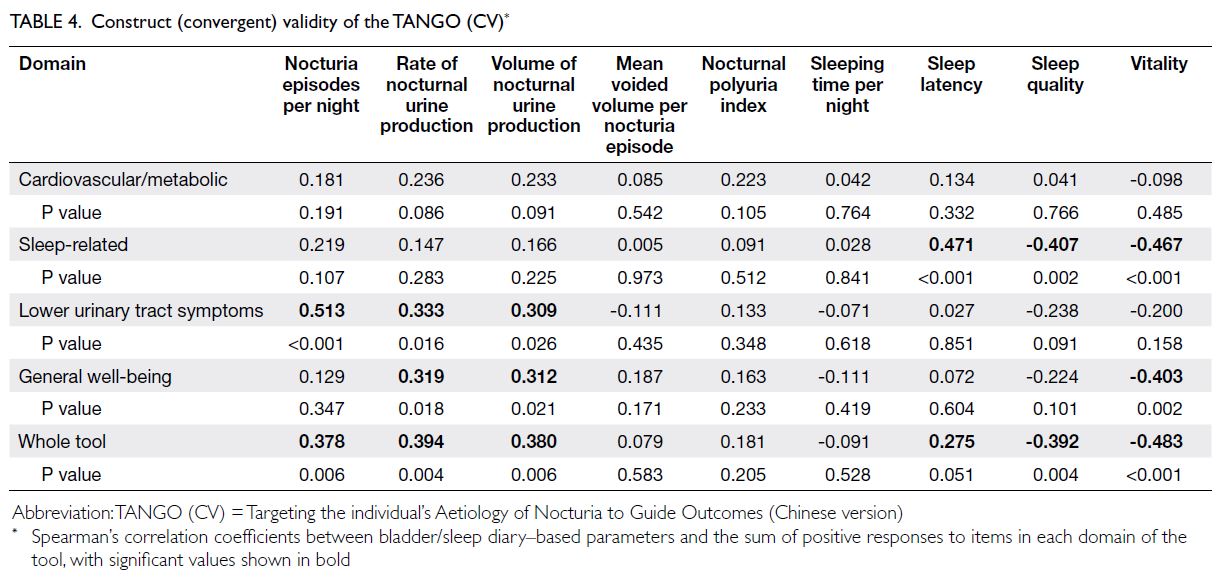
Construct (convergent) validity
Table 4 shows the construct (convergent) validity of the TANGO (CV). The sleep-related domain was
positively correlated with sleep latency [ρ=0.471
(P<0.001)], whereas it was negatively correlated
with sleep quality [ρ=-0.407 (P=0.002)] and vitality
after sleep [ρ=-0.467 (P<0.001)], as reported in
the bladder/sleep diary. The LUTS domain was
positively correlated with the number of nocturia
episodes, rate of nocturnal urine production, and
volume of nocturnal urine production [ρ=0.513
(P<0.001), ρ=0.333 (P=0.016), and ρ=0.309 (P=0.026),
respectively]. However, the LUTS domain was not
correlated with sleep/vitality parameters. In contrast,
the general well-being domain was significantly
positively correlated with the rate and volume of
nocturnal urine production [ρ=0.319 (P=0.018) and
ρ=0.312 (P=0.021), respectively]; it was significantly negatively correlated with vitality after sleep
[ρ=-0.403 (P=0.002)]. The cardiovascular/metabolic
domain did not display significant correlations with
the bladder/sleep diary parameters. Nonetheless, the
whole tool was significantly positively correlated with
the number of nocturia episodes [ρ=0.378 (P=0.006)], the rate and volume of nocturnal urine production
[ρ=0.394 (P=0.004) and ρ=0.380 (P=0.006),
respectively], and sleep latency very closely [ρ=0.275
(P=0.051)]; it was significantly negatively correlated
with sleep quality and vitality after sleep [ρ=-0.392
(P=0.004) and ρ=-0.483 (P<0.001), respectively].
Criterion validity
Criterion validity was confirmed for each domain and the whole tool (ρ=0.287-0.687). Regarding criterion
validity, the cardiovascular/metabolic domain was
only significantly correlated with the STOP-Bang
questionnaire. The sleep-related domain was not
correlated with questionnaires specifically designed
to assess obstructive sleep apnoea. However, this
domain was strongly correlated with the IPSS, IPSS
QoL, and the sleep/energy, bother/concern, and
total domains of NQoL (Table 5). The LUTS domain
was significantly correlated with the STOP-Bang
questionnaire, IPSS, OABSS questionnaire, and
NQoL; the strongest correlations involved IPSS total
[ρ=0.651 (P<0.001)], OABSS [ρ=0.642 (P<0.001)],
and NQoL bother/concern [ρ=0.551 (P<0.001)].
In contrast to the LUTS domain, the general well-being
domain was significantly correlated with the
ESS; it was also correlated with the IPSS, OABSS
questionnaire, ICIQ-N-4(b) and NQoL, but these
correlations were weaker than the correlations of the
LUTS domain (Table 5).
Discriminant validity
Receiver operating characteristic analysis (Fig)
showed that a cut-off of four positive responses on
the TANGO (CV) could distinguish patients from controls (Youden’s J statistic=0.453; area under the
curve=0.818, 95% confidence interval [CI]=0.683-0.953; odds ratio=7.81, 95% CI=2.02-30.30;
sensitivity: 83%, specificity: 62%), whereas a cut-off
of five positive responses could distinguish patients
with significant nocturia distress from patients with
mild nocturia distress (Youden’s J statistic=0.398;
area under the curve=0.729, 95% CI=0.581-0.878;
odds ratio=4.07, 95% CI=1.17-14.15; sensitivity:
70%, specificity: 63%).

Figure. Receiver operating characteristic (ROC) curves (in red) showing sensitivity (true positives) and 1-specificity (false positives) for distinguishing (a) patients from controls and (b) patients with significant nocturia distress from patients with mild nocturia distress, based on the sum of positive responses on the TANGO (CV). Cut-off values are indicated by dashed circles. Blue lines are baseline classification due to chance
Discussion
Current questionnaires in evaluating nocturia
The International Continence Society (ICS) defines
nocturia as the need to wake at least once during the
night to void. Each instance of voiding is preceded
and followed by sleep.20 A recent Delphi panel convened by the ICS5 recommended using disease-specific
questionnaires in the diagnostic pathway for
nocturia. In English, there are a few psychometrically
validated disease-specific measurement tools for
nocturia: the NQoL, developed and validated by
Abraham et al12; the ICIQ-N, a form of the NQoL
modified from the ICIQ (https://iciq.net/iciq-nqol);
and the Nocturia, Nocturnal Enuresis and Sleep-Interruption Questionnaire (NNES-Q) developed by Bing et al.21 The ICIQ-N11 is a combined
questionnaire that incorporates a bladder diary–Nocturia Impact Diary.22 However, all of these tools
mainly focus on the impact of nocturia on distress
and quality of life in affected patients; none of them
explore the aetiologies of nocturia.
The TANGO has emerged as a questionnaire
that can capture information concerning the
multifaceted nature of nocturia and identify nocturia-related
co-morbidities.7 23 This tool is expected
to be useful across various medical specialties to
facilitate, improve, and accelerate the process of
nocturia management. Thus far, the TANGO has
been translated into Dutch,24 Arabic,25 and Turkish.26
However, none of these translated versions have been
subjected to validity assessment using a bladder/sleep diary. To our knowledge, the present study is
the first to perform such an assessment.
Translation and development of the TANGO
(CV)
The ages of our study participants were similar to
that of individuals in whom nocturia is commonly
observed (>60 years). We found that the TANGO
(CV) could be easily comprehended by patients
visiting urology clinics, as indicated by the small
percentage of missing responses (0.4%) and minimal
need for assistance from medical staff (97%); these
results suggested good content validity. The low
rate of missing responses might be related to the
dichotomous-choice nature of responses to items,
which facilitated answers by participants.
In all, 94% of our participants with ≥2 nocturia
episodes/night were affected by multiple domains of
aetiological factors/nocturia-related co-morbidities;
approximately 8% of patients reported experiencing
falls, which is a higher percentage than in a previous
study that used a nocturia-specific questionnaire
(<3%).27 The distribution of aetiologies/co-morbidities
of nocturia in our study was similar
to the distribution reported by a Turkish group26:
the LUTS domain was most commonly observed,
followed by the sleep-related domain, and then
the cardiovascular/metabolic domain. However,
the rate of poor general well-being was lower in
the present study than in the Turkish study. The
simple TANGO (CV) can easily capture information
concerning the multifactorial nature of nocturia
that could be not elucidated by other nocturia-specific
questionnaires.11 12 21 22 Thus, it will facilitate the provision of more individualised treatment for
nocturia.
The KR-20 coefficient for the whole tool was
0.711 (>0.700), confirming the internal consistency
of the whole TANGO (CV) tool. The highest domain-specific
positive response correlation coefficient was
observed in the sleep-related domain, implying that
nocturia is closely related to impaired sleep quality and disrupted sleep architecture.
The high ICC value (>0.8) for each domain of
nocturia-related problems confirmed the excellent
test-retest reliability of the tool, in combination
with the convergent validity identified in the sleep-related,
LUTS, and general well-being domains
of the TANGO (CV). With the exception of the
cardiovascular/metabolic domain, criterion validity
was also established for other domains and the
whole TANGO (CV) tool; the criterion validity
was the greatest in the LUTS domain, followed by
the sleep-related domain and then the general well-being
domain. Importantly, the original version of
the TANGO7 does not provide a symptom score,
although such a score is strongly recommended in
European Association of Urology guidelines as a
means of quantifying symptoms and distinguishing
patients with mild problems from patients with
severe problems.28 In this regard, a scoring system
involving the various domains of the TANGO has
recently been proposed to distinguish the relative
contributions of nocturia aetiologies to treatment
outcomes.8 In the present study, we showed that by
using cut-offs of four and five positive responses,
respectively, the sum of the positive responses could
distinguish individuals with more nocturia episodes
(≥2/night) from individuals with fewer nocturia
episodes (≤1/night), and patients with significant
nocturia distress (Question 12 of NQoL) from
patients with mild nocturia distress (Fig). These
findings confirmed the discriminatory validity of the
TANGO (CV).
The cardiovascular/metabolic domain
demonstrated suboptimal performance in terms
of internal consistency, convergent, criterion, and
discriminant validity. These findings might be
related to selection bias in that patients with higher
cardiovascular risk were not recruited [ie, there was
a low positive response rate (72 of 455 potential
responses, 16%)].
Use of the TANGO (CV) in clinical practice
The TANGO (CV) can be used to investigate
common aetiologies and nocturia-related outcomes
across multiple medical specialties, providing
guidance for subsequent treatment. For example,
positive responses to Questions 1, 2, and 3 in the
cardiovascular/metabolic domain and Question
13 in the sleep-related domain may indicate
that desmopressin is less appropriate or even
contraindicated for the treatment of nocturia, in
accordance with the recent consensus report by
the ICS.5 The questionnaire can also be used as
a screening tool for epidemiological studies and
routine clinical work-up for nocturia. It is a simple,
rapid, easily understood, and clinically meaningful
tool that can help clinicians to thoroughly evaluate
nocturia aetiology and related problems earlier in the clinical pathway of nocturia treatment. Moreover,
it may be useful in categorising or predicting the
prognosis of nocturia in adults.
Limitations
The limitations of the current study included the
fact that about 70% of the participants were men,
which may limit its utility in assessment of female
patients with nocturia. Additionally, the sample
size was insufficient to clarify correlations among
domain variables, number of positive responses, and
subtotal and total symptom scores across the various
questionnaires used for validation. The inclusion of
patients with more pronounced illnesses within the
studied domains should be considered to clearly
identify relationships among nocturia, aetiologies,
lower urinary tract function, and co-morbidities,
as measured by bladder/sleep diaries and validated
questionnaires.
Conclusion
The TANGO (CV) is a multi-dimensional, self-administered, formally translated, psychometrically
validated Chinese version of the TANGO. It can
be used to screen for aetiologies and measure the
impacts of nocturia-related problems on affected
individuals, including their quality of life. The sum of
positive responses to the whole tool was significantly
correlated with the degree of nocturia-related
distress.
Author contributions
Concept or design: SKK Yuen, W Bower, CF Ng.
Acquisition of data: SKK Yuen, CSY Li, HSW Kwok.
Analysis or interpretation of data: SKK Yuen, PKF Chiu, JYC Teoh.
Drafting of the manuscript: SKK Yuen, CF Ng.
Critical revision of the manuscript for important intellectual content: SKK Yuen, CF Ng, SSM Hou.
Acquisition of data: SKK Yuen, CSY Li, HSW Kwok.
Analysis or interpretation of data: SKK Yuen, PKF Chiu, JYC Teoh.
Drafting of the manuscript: SKK Yuen, CF Ng.
Critical revision of the manuscript for important intellectual content: SKK Yuen, CF Ng, SSM Hou.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As editors of the journal, CF Ng and JYC Teoh were not involved in the peer review process. Other authors have
disclosed no conflicts of interest.
Acknowledgement
We thank all staff from Lithotripsy and Uro-investigation Centre of Prince of Wales Hospital and research staff from
Department of Urology of The Chinese University of Hong
Kong for facilitating the data collection.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study protocol was approved by the Joint Chinese University of Hong Kong—New Territories East Cluster
Clinical Research Ethics Committee (Ref No.: 2019.400), in
accordance with the Declaration of Helsinki and the Good
Clinical Practice guidelines. Informed consent to take part in
the research was obtained from all participants.
References
1. Yee CH, Chan CK, Teoh JY, et al. Survey on prevalence
of lower urinary tract symptoms in an Asian population.
Hong Kong Med J 2019;25:13-20. Crossref
2. Bosch JL, Weiss JP. The prevalence and causes of nocturia. J Urol 2013;189(1 Suppl):S86-92. Crossref
3. Ho LY, Chu PS, Consigliere DT, et al. Symptom prevalence,
bother, and treatment satisfaction in men with lower
urinary tract symptoms in Southeast Asia: a multinational,
cross-sectional survey. World J Urol 2018;36:79-86. Crossref
4. Ho LY, Chan CK, Chu PS. Patient opinion of lower urinary
tract symptoms and their treatment: a cross-sectional
survey in Hong Kong public urology clinics. Hong Kong
Med J 2017;23:562-9. Crossref
5. Everaert K, Hervé F, Bosch R, et al. International Continence Society consensus on the diagnosis and
treatment of nocturia. Neurourol Urodyn 2019;38:478-98. Crossref
6. Weiss JP, Blaivis JG, Blanker MH, et al. The New England
Research Institutes, Inc. (NERI) Nocturia Advisory
Conference 2012: focus on outcomes of therapy. BJU Int
2013;111:700-16. Crossref
7. Bower WF, Rose GE, Ervin CF, Goldin J, Whishaw DM,
Khan F. TANGO—a screening tool to identify
comorbidities on the causal pathway of nocturia. BJU Int
2017;119:933-41. Crossref
8. Rose GE, Bower WF. Development of a scoring process for
the nocturia causality screening tool TANGO: a rationale
and methodology. Aust N Z Continence J 2020;26:32-8. Crossref
9. Sperber AD. Translation and validation of study
instruments for cross-cultural research. Gastroenterology
2004;126(1 Suppl 1):S124-8. Crossref
10. Chan HC. The psychometric evaluation of the Chinese version of the International Prostate Symptom Score
(IPSS) [thesis]. Hong Kong: The University of Hong Kong;
2004: 174.
11. Avery K, Hashim H, Gardener N, Abrams P, Donovan J, Abraham L. Development and psychometric evaluation of
the ICIQ nocturia module: the ICIQ-N. (Abstract 595), in
ICS/IUGA 2004. Paris; 2004.
12. Abraham L, Hareendran A, Mills IW, et al. Development and validation of a quality-of-life measure for men with
nocturia. Urology 2004;63:481-6. Crossref
13. Yiu MK, Li CM, Hou SM, Wong CW, Tam S, Chu SK. Reliability and validity of the overactive bladder symptom
score in Hong Kong Chinese. Hong Kong Med J
2013;19:504-10. Crossref
14. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540-5. Crossref
15. Ha SC, Lee DL, Abdullah VJ, van Hasselt CA. Evaluation and validation of four translated Chinese questionnaires for obstructive sleep apnea patients in Hong Kong. Sleep
Breath 2014;18:715-21. Crossref
16. Kuder GF, Richardson MW. The theory of the estimation of test reliability. Psychometrika 1937;2:151-60. Crossref
17. Bujang MA, Baharum N. Guidelines of the minimum sample size requirements for Cohen’s kappa. Epidemiol
Biostat Public Health 2017;14:e12267. Crossref
18. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Philadelphia (PA): Lawrence Erlbaum Associates; 1988.
19. Bujang MA, Baharum N. Sample size guideline for correlation analysis. World J Soc Sci Res 2016;3:37-46. Crossref
20. Hashim H, Blanker MH, Drake MJ, et al. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol Urodyn 2019;38:499-508. Crossref
21. Bing MH, Moller LA, Jennum P, Mortensen S, Lose G.
Validity and reliability of a questionnaire for evaluating
nocturia, nocturnal enuresis and sleep-interruptions in an
elderly population. Eur Urol 2006;49:710-9. Crossref
22. Holm-Larsen T, Andersson F, van der Meulen E, Yankov V,
Rosen RC, Nørgaard JP. The Nocturia Impact Diary: a self-reported
impact measure to complement the voiding diary.
Value Health 2014;17:696-706. Crossref
23. Bower WF, Everaert K, Ong TJ, Ervin CF, Norgaard JP, Whishaw M. Questions to ask a patient with nocturia. Aust
J Gen Pract 2018;47:465-9. Crossref
24. Decalf V, Everaert K, De Witte N, Petrovic M, Bower W.
Dutch version of the TANGO nocturia screening tool:
cross-culturally translation and reliability study in
community-dwelling people and nursing home residents.
Acta Clin Belg 2020;75:397-404. Crossref
25. Altaweel W, Alrumayyan M, Seyam R. Arabic language
validation of TANGO questionnaire for nocturia: a
translation into the Arabian Peninsula dialect. Neurourol
Urodyn 2020;39:2146-52. Crossref
26. Culha MG, Culha Y, Buyukyilmaz F, Turan N, Bower W. “TANGO” nocturia scanning tool: Turkish validity and
reliability study. Low Urin Tract Symptoms 2021;13:88-92. Crossref
27. Yamanishi T, Fuse M, Yamaguchi C, et al. Nocturia Quality-of-Life questionnaire is a useful tool to predict
nocturia and a risk of falling in Japanese outpatients: a
cross-sectional survey. Int J Urol 2014;21:289-93. Crossref
28. Gravas S, Cornu JN, Gacci C, et al. EAU Guidelines on
management of non-neurogenic male lower urinary tract
symptoms (LUTS), incl. Benign Prostatic Obstruction
(BPO). European Association of Urology Guidelines Office:
Arnhem, The Netherlands; 2020. Available from: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Non-Neurogenic-Male-LUTS-2023.pdf. Accessed 26 Jul 2023.