Hong Kong Med J 2020 Jun;26(3):184–91 | Epub 28 May 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Awareness of fertility preservation among
Chinese medical students
Elaine YL Ng, BSc1; Jeffrey KH Ip2, Diane R Mak2, Andrea YW Chan2, Jacqueline PW Chung, MB, ChB (CUHK), FHKAM (Obstetrics and Gynaecology)1
1Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong
2Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Prof Jacqueline PW Chung (jacquelinechung@cuhk.edu.hk)
Abstract
Introduction: The fertility preservation (FP) services
offered in Hong Kong are underutilised. There
have been no previous studies on Chinese medical
students to investigate the underlying reasons for this
underutilisation in terms of awareness, knowledge,
and attitudes towards FP and age-related fertility.
Methods: This was a cross-sectional survey among Chinese medical students in Hong Kong.
Results: The majority of participants (77.8%) were
not familiar with any clinics or specialists who
provide FP services. The vast majority (88.1%)
underestimated female infertility at age 45 years, and
89.8% overestimated the age of male fertility decline.
The students’ FP knowledge was mainly acquired
from electronic media (58.4%) and medical school
(57.6%). Medical students showed overwhelming
support towards FP for medical reasons (97.9%) but
had mixed responses about FP for elective reasons
related to career development in women (58.8%). Of
the participants, 80.2% agreed that the government
should subsidise FP services for patients with medical reasons.
Conclusion: This study highlights the limited
awareness and knowledge of FP among Chinese
medical students. There is a strong worldwide need
to increase education about and exposure to FP
in the medical curriculum and improve medical
students’ knowledge.
New knowledge added by this study
- Chinese medical students tend to overestimate the success rate of in vitro fertilisation and the age of male fertility decline.
- Chinese medical students who had completed the clinical attachments of the obstetrics and gynaecology module rotations showed significantly higher awareness of fertility preservation, reproductive techniques used, and the availability of specialty clinics than did medical students who had not completed the module.
- Appropriate and timely education can improve medical students’ awareness and knowledge.
- More involvement from the public sector and enhanced facilities in terms of service provision and financial support could increase FP service utilisation.
Introduction
Chemotherapy, radiotherapy, certain medications
for cancer, and some rheumatological and
haematological diseases are gonadotoxic, which
can jeopardise patients’ fertility, particularly that
of young cancer survivors.1 With advancements in treatment, the 5-year survival rate of patients with
cancer in childhood and adolescence has increased
to over 80%.2 Thus, improving their quality of life and reducing their risk of infertility is an important
aspect of their management plan.
International clinical guidelines, including the
American Society of Clinical Oncology (ASCO),3
European Society for Medical Oncology (ESMO),4
and Royal College of Radiologists guidelines,5 suggest discussion of fertility preservation (FP) with patients
of childhood and reproductive age during the course
of cancer therapy. However, a study showed that
fewer than half of oncologists routinely refer their
patients to reproductive endocrinologists, and even
fewer oncologists follow the guidelines, despite their
willingness to discuss infertility in relation to cancer
therapy.6 Moreover, a lack of awareness and related
training about FP among clinicians may cause
underutilisation of FP services worldwide, including
in Canada, the US, and Hong Kong.7 8 9 In Hong Kong,
clinicians and patients alike may consider FP as an
expensive, privatised option without subsidisation.
In a previous cross-sectional study that
evaluated the awareness, attitudes, and knowledge of FP among clinicians across different specialties
in Hong Kong, only 45.6% of clinicians were familiar
with FP.10 As current medical students will become
our future clinicians, it is important to assess their
level of understanding and awareness of fertility and
FP, as this may greatly influence their future practice
and consideration of appropriate interventions
to improve affected patients’ outcomes. Cross-sectional
studies have been conducted to assess
college students’ awareness and knowledge of
fertility in Canada,11 Serbia,12 and the US.13 These
studies in Western populations showed knowledge
inadequacy about age-related fertility decline and
FP. However, to the best of our knowledge, there are
no studies in a Chinese population that have aimed
to investigate the awareness, knowledge gaps, and
attitudes of medical students regarding fertility and
FP. Therefore, the aims of this study were to evaluate
the awareness of, attitudes towards, and knowledge
regarding FP among Chinese medical students in
Hong Kong.
Methods
This was a cross-sectional survey conducted
from November 2018 to June 2019. The study
population consisted of Chinese medical students
from The Chinese University of Hong Kong.
Chinese undergraduate students aged ≥18 years
studying in the Medicine programme and capable of
communicating in English were included. Those who
were non-Chinese, under age 18 years, incapable of
communicating in English, and those who refused to
join the study were excluded.
Eligible participants were invited to complete
a self-administered online survey. The online survey
was sent to participants by internal mass email and
social networking applications. Snowball sampling
was done by encouraging medical students to send
the online survey to their classmates to boost the
response rate.
The online survey was developed on an
electronic form (MyCUform). The self-administered
survey included a brief explanation and was
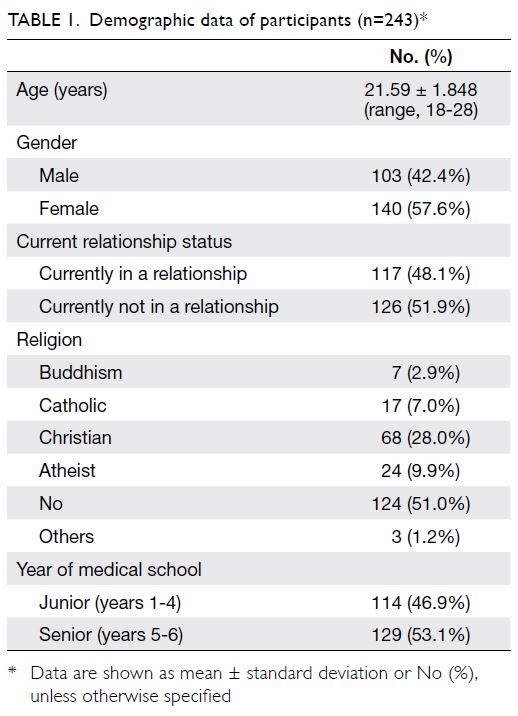
comprised of four parts: (1) baseline demographic
data (Table 1); (2) awareness of FP; (3) knowledge
about FP (Table 2); multiple choice questions
consisting of five or six options on knowledge about
fertility and FP; and (4) attitudes towards FP (Tables 3 and Table 4). It consisted of 38 questions and took
approximately 15 minutes to finish. The survey was
developed after reviewing the literature.14 15 16 It was
assessed for logical validity by three physicians in
the Department of Obstetrics and Gynaecology, who
reviewed the accuracy of the contents. The survey
was also piloted on a small number of doctors and
medical students for content clarity and modified
accordingly to incorporate the pilot participants’
feedback. The final version was then administered to
the full study’s participants.
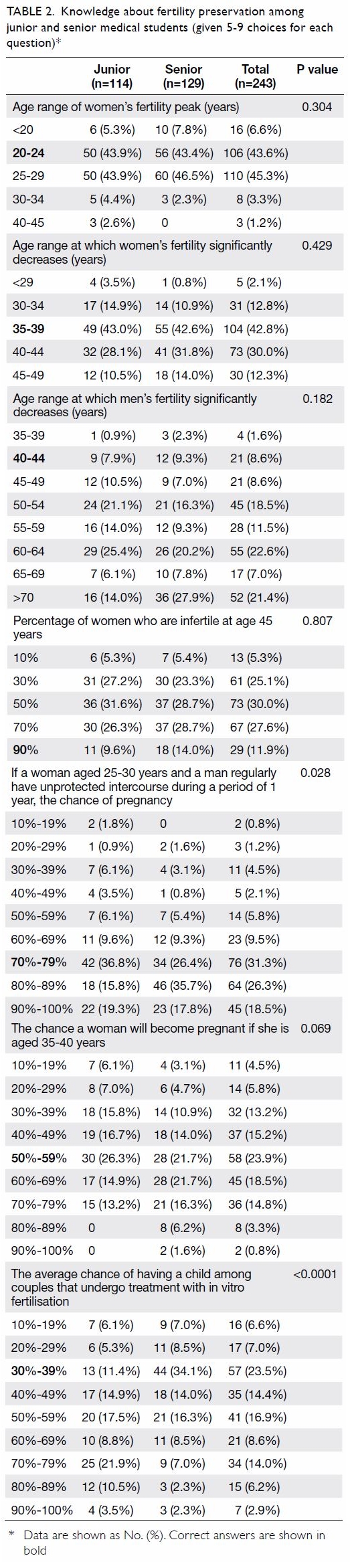
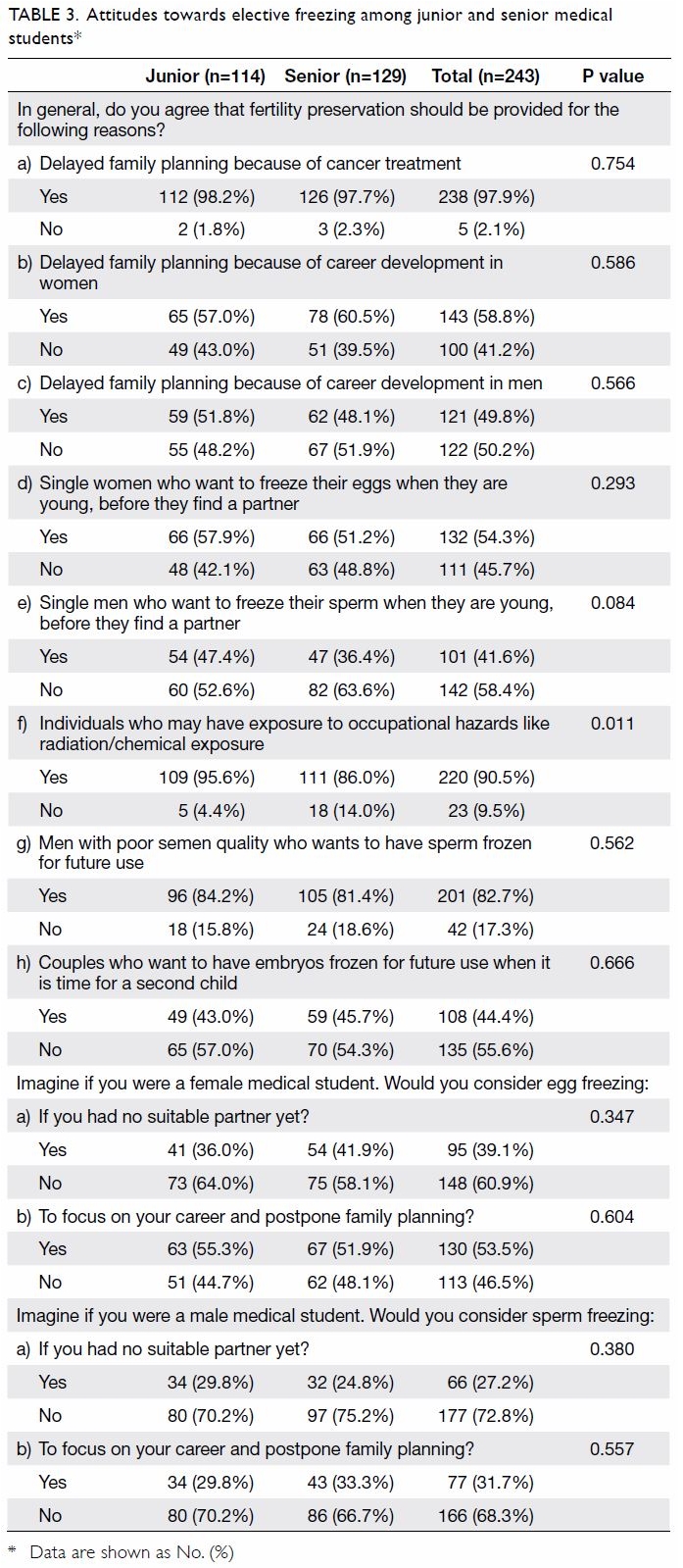
Table 2. Knowledge about fertility preservation among junior and senior medical students (given 5-9 choices for each question)
Statistical analysis was performed using SPSS
(Windows version 24.0; IBM Corp, Armonk [NY],
US). Continuous data were described as means,
standard deviations, and percentiles. Categorical data were summarised as frequencies and percentiles.
Subgroup analyses were performed between gender
and year groups, with the medical students split
into junior (year 1-4) and senior (year 5-6) year
groups. Junior medical students had not completed
the clinical attachments of the obstetrics and
gynaecology module rotation (OB-GYN), whereas
senior medical students had finished the OB-GYN
module in year 5. The categorical data were tested
by Pearson’s Chi squared test or Fisher’s exact test
to check for significant differences between groups.
Results with P values of <0.05 were considered
statistically significant.
Results
Approximately 700 Chinese medical students were
approached through social networking applications
and email, and 243 completed the online survey
(response rate: 34.7%). Table 1 summarises the
participants’ demographic data. In terms of age
distribution, there was no significant difference
(P=0.597) between the two groups.
Awareness
Overall, 71.2% (n=173) of respondents were aware
of FP strategies. Despite this, 77.8% (n=189) of
respondents were not familiar with any clinics or
specialists who provide FP services. Senior students
showed better awareness than junior students of
the above items (P<0.001). The majority (86.8%,
n=211) had not heard of any regulations related
to FP. Gamete and embryo freezing were the most
well-known FP methods, with female students being
significantly more aware than male students of those
methods (P<0.003).
The majority (71.2%, n=173) responded that
they would discuss the option of FP with their
patients as future doctors, even if the treatment had
a <30% chance of causing infertility. If a treatment
had a ≥70% chance of causing infertility, nearly all
(95.5%, n=232) students would discuss FP.
Knowledge
Table 2 shows the results of the questions that address knowledge about fertility and FP. Overall, there were
no gender differences besides the response regarding
the age range of a woman’s significant fertility decline:
proportionally more female students answered that
item correctly (45.7% vs 38.8%; P<0.05).
Knowledge regarding FP was mainly acquired
from electronic media (58.4%, n=142), medical school
(57.6%, n=140), and medical professionals (38.7%,
n=94). More senior students than junior students
acquired fertility knowledge through medical school
education (81.4% vs 30.7%; P<0.0001) and medical
professionals (54.3% vs 21.1%; P<0.0001).
Most of the responding students (86.4%,
n=210) wished to know more about FP, with 80.7%
(n=196) of the students agreeing that there is a
need to incorporate FP material into the medical
curriculum.
Attitudes
Regarding attitudes, 94.2% (n=229) of medical
students agreed that establishing one or two
dedicated clinics or centres for FP counselling is
necessary. Subgroup analysis indicated that more
male medical students would like to have two
dedicated centres (75.0% vs 68.2%, P=0.021). More
senior than junior students agreed that FP should be
available solely as a public service (89.1% vs 71.9%;
P=0.001). Overall, 97.9% (n=238) of participants
thought that practice guidelines for FP should be
required. More than half of respondents (59.7%,
n=145) agreed that there should be an age limit for
FP. More female than male students agreed to set an
age limit for FP (65.7% vs 51.5%, P=0.025).
Among various factors considered by medical
students to determine whether to recommend
FP to patients, the desire to have children (51.0%, n=124), the prognosis of cancer or a medical
condition (23.5%, n=57), and time available before
gonadotoxic treatment (7.4%, n=18) were the most
likely considerations.
Most participants (80.2%, n=195) responded
that the government should subsidise FP in
patients undergoing gonadotoxic treatment, with
senior students expressing stronger support for
subsidisation than junior students (86.0% vs 73.7%;
P<0.02). More than half of the responding students
agreed that the government should subsidise 30% to
50% of the cost of FP procedures including sperm
(79.8%, n=194) and egg freezing (80.2%, n=195),
and in vitro fertilisation (IVF) [67.9%, n=165].
More senior than junior students thought that the
government should subsidise >70% of the cost of IVF
(34.1% vs 20.1%; P<0.02).
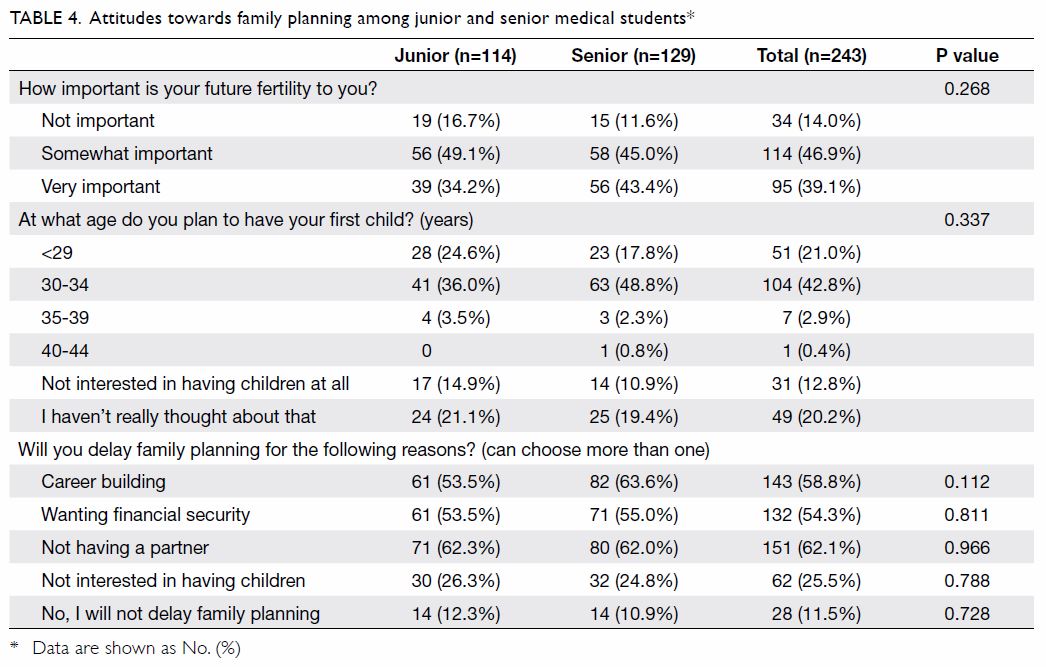
Table 3 shows the respondents’ attitudes
towards elective and medical gamete and embryo
freezing. More male students than female students
expressed agreement with FP provision to men
because of having no suitable partner (34.0% vs
22.1%; P<0.05). Table 4 illustrates attitudes towards
family planning among the responding medical
students. More male than female students were
determined not to delay their family planning (16.5%
vs 7.9%, P=0.037).
Discussion
With the advancement of technology, FP has
become increasingly effective at enabling patients who have undergone gonadotoxic treatment to
raise families. However, as shown by many previous
studies on medical students’ understanding of FP,
this study reflects an overall worldwide tendency
towards a lack of awareness and knowledge about
fertility and FP.11 12 13 To the best of our knowledge,
this is the first study that has aimed to investigate
the awareness, knowledge, and attitudes of Chinese
medical students regarding fertility and FP, as well as
identifying their knowledge gaps in the subject.
Awareness
The majority of Chinese medical students in Hong
Kong have heard of at least one FP strategy. Senior
students had significantly greater awareness than
junior students of FP, reproductive techniques, and
the availability of specialty clinics, likely reflecting
the knowledge and exposure gained during the
clinical OB-GYN module in the fifth year of study.
This suggests that appropriate and timely education
can improve medical students’ awareness of FP.
Previous studies have shown that even brief
educational interventions about FP to medical
students and house staff have potential benefits.13 To
provide quality service, ASCO and ESMO guidelines
suggest that patients with cancer be informed of
their potential fertility decline and referred to FP
services after treatment.3 4 Most students responded
that they would refer patients to FP services even if
treatment had only a low risk of infertility, but they
were not familiar with the actual practice of FP, including relevant regulations and referral methods.
Downloadable fact sheets on the effects of cancer
treatment on fertility, available options for FP, and
a list of service providers with reference costs stated
should be available and accessible for proper patient
education and counselling.
Knowledge
There are several misconceptions among medical
students regarding knowledge about fertility and
FP. The responding medical students tended to
overestimate the age of the female fertility peak
and the success rate of IVF and underestimate the
risk of infertility in women at age 45 years (Table 2). Overestimation of female fertility has also been
observed in overseas studies.11 12 13 17 18 Medical students
have better knowledge about female fertility than
male fertility. This could be explained by the fact that
there have been many more studies about the concern
of female fertility decline with age. As sex education
programmes at the secondary and university levels
mainly emphasise pregnancy prevention education
rather than infertility awareness, there may be a
lack of knowledge about the impact of ageing on
fertility among women.11 Fertility-related knowledge
should be included in the undergraduate medical
curriculum and ideally be integrated in high school
education as well to enhance public education on
this topic. Beyond patient care, medical students’
inadequate knowledge about this topic also has great
implications for their future careers and personal
lives. They may delay their own family planning for
career reasons without sufficient consideration of
their impending fertility decline or may have a false
sense of security regarding the success rate of IVF.
Therefore, more education about fertility is required,
which was also supported by the respondents of our
study.
Electronic media play a significant role in the
promotion of FP, especially among junior students.
In contrast, medical school was the main source
of FP knowledge for senior students, followed by
medical professionals and electronic media. This
is consistent with findings in American medical
students and house staff.13 Media reports of female
celebrities undergoing FP procedures, particularly
egg freezing, could explain the high prevalence of
student familiarity with this procedure and their lack
of knowledge about other, less popular options.19
Knowledge acquisition through both the medical
curriculum and electronic media have proven to
be significant, particularly in people who have not
received formal education about FP. This can be
applied to the general public, although it poses a
risk of promoting misinformation: people could be
misled into having a false sense of security regarding
successful childbearing late in one’s reproductive life
through the use of FP methods.11 Therefore, caution should be used to ensure that materials released through the media are accurate.
Attitudes
Most of the responding medical students would first
consider the patient’s desire when referring patients
for FP, while 41.3% of physicians would consider
the patient’s prognosis first.10 This finding could be
explained by the medical students’ lack of medical
practice experience and doctors’ awareness of
resource limitations, as it has been shown that junior
doctors make judgements mostly based on their own
assumptions, compared with the experience-based
judgements made by senior doctors.20
The private sector is the only current provider
of FP services in Hong Kong. More male than female
medical students who responded to our survey
had positive attitudes towards the establishment of
related facilities. The cost of freezing gametes is at
least US$7800 (US$1 to HK$7.8),21 and the median
monthly household income of a 1-person family in
Hong Kong is US$1282.22 There are currently no
gamete freezing subsidy programmes available. Such
high costs are unaffordable to many patients, and
especially patients with cancer are already financially
burdened by their current treatment. In this regard,
most medical students agreed that the government
should subsidise FP services to patients undergoing
gonadotoxic treatment, with more than half agreeing
that 30% to 50% is a reasonable subsidy proportion.
There has been an increasing trend towards
elective FP in recent years, which has opened
up a debate about the ethicality of FP for non-medical
indications and whether FP should only be
provided for medical reasons. Our study reflected
overwhelming support for FP for medical reasons.
However, the responding medical students’ opinions
were mixed regarding elective freezing for non-medical
indications. Only approximately half of the
respondents agreed that FP should be provided to
people because they have not found a suitable partner,
or because they delay family planning for the sake of
career development. Despite the mixed responses
regarding elective freezing, Chinese medical
students from Hong Kong were more supportive of
elective freezing than undergraduates and medical
students from the US.23 This finding may be driven
by the higher cost of FP in the US compared with
that in Hong Kong.23 Indeed, elective freezing has
gained popularity in recent years. Still, the greater
acceptance of FP for medical reasons echoes the
healthcare-related perceptions and expectations of
patients in Hong Kong: fertility is not a necessity,
and FP healthcare is considered a luxury as opposed
to a necessity for immediate physical well-being.
This study’s participants were more supportive
of elective freezing for women than men. This is
likely because of their awareness that women’s fertility declines relatively earlier than that of men.
Moreover, women in Hong Kong are expected to
have a predominantly domestic and childrearing
role within their families,16 largely because of deeply
rooted traditional Chinese familial constructs in
which women tend to take on homemaking roles.
However, the male medical students who responded
were also concerned about their own family
planning. This study’s results show that more male
than female medical students were determined not
to delay their family planning or stated their intent
to have gametes frozen because they had no suitable
partner.
Most medical students agree that their future
fertility is important to them. Over half of the
responding medical students stated their intent to
delay family planning for career development, and
the majority plan to have their first child between
age 30 and 34 years (the average age of residency
completion is 29 years). However, few responded
that they would consider undergoing FP treatments.
This paradoxical response is consistent with the
results of another study on Hong Kong university
students that showed low inclination to seek help
in the event of fertility problems compared with
Western counterparts.16 The taboo of childlessness
in Chinese culture may be another reason why
planning and conversation are discouraged in the
event of infertility.16 Thus, students may view FP
techniques as drastic and unconventional, preferring
natural conception. As discussed earlier, the lack of
correct knowledge about age-related female fertility
decline could also lead to such results. Medical
training is long, potentially delaying doctors from
starting families during their most fertile years.
Education is beneficial not only to future patients,
but also to current and future physicians’ quality of
life.
Limitations
As a form of convenience sampling, the online
survey method was chosen to efficiently distribute
the survey throughout the large population of
medical students. However, this inherently came
with limitations, including low response rate,
small sample size, selection bias, and the inability
to characterise non-respondents. Ideally, students
of other medical schools in Hong Kong should be
included to make our study more comprehensive;
however, this would be logistically difficult. Because
of constraints on advertising, the study consisted
of slightly more senior than junior students and
more female than male respondents. Moreover, our
study did not specifically ask about the educational
background of students that may have influenced
their knowledge. However, there was no significant
difference in the age distribution between the junior
and senior student groups. Information bias may have also affected the responses from students who
had not completed the OB-GYN module.
Conclusion
In conclusion, this study revealed important aspects
of FP from the perspective of Chinese medical
students in Hong Kong. In particular, we highlighted
that awareness and knowledge of FP are limited
among medical students. There is a strong worldwide
need to increase education about and exposure of
FP in the curriculum to improve medical students’
knowledge. More involvement from the public sector
and enhancement of facilities in terms of service
provision and financial support for FP services are
also needed. Given the variety of perspectives on
childbearing among different cultures, this should
be taken into account when doctors consider FP
options for their patients and themselves. Only by
increasing awareness and knowledge can more
accepting attitudes towards FP arise among our
doctors, allowing for better clinical outcomes and
quality of life for future patients.
Author contributions
Concept or design: JPW Chung, EYL Ng.
Acquisition of data: All authors.
Analysis or interpretation of data: EYL Ng.
Drafting of the article: All authors.
Critical revision for important intellectual content: JPW Chung.
Acquisition of data: All authors.
Analysis or interpretation of data: EYL Ng.
Drafting of the article: All authors.
Critical revision for important intellectual content: JPW Chung.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, JPW Chung was not involved in the peer review process of the article. Other authors have no
conflicts of interest to disclose.
Acknowledgement
The authors would like to thank the medical students at The Chinese University of Hong Kong for their kind participation
in the study.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethical approval for the study was obtained from the Survey and Behavioural Research Ethics Committee (Ref SBRE-18-168).
References
1. Husson O, Huijgens PC, van der Graaf WTA. Psychosocial challenges and health-related quality of life of adolescents and young adults with hematologic malignancies. Blood
2018;132:385-92. Crossref
2. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin 2019;69:7-34. Crossref
3. Oktay K, Harvey BE, Partridge AH, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol 2018;36:1994-2001. Crossref
4. Peccatori FA, Azim HA Jr, Orecchia R, et al. Cancer, pregnancy and fertility: ESMO Clinical Practice Guidelines
for diagnosis, treatment and follow-up. Ann Oncol 2013;24
Suppl 6:vi160-70. Crossref
5. The Royal College of Physicians, The Royal College of Radiologists, The Royal College of Obstetrics and
Gynaecology. The effects of cancer treatment on
reproductive functions: guidance on management 2007.
Available from: https://www.rcr.ac.uk/system/files/
publication/field_publication_files/Cancer_fertility_
effects_Jan08.pdf. Accessed 3 Jan 2020.
6. Köhler TS, Kondapalli LA, Shah A, Chan S, Woodruff TK, Brannigan RE. Results from the Survey for Preservation of
Adolescent Reproduction (SPARE) study: gender disparity
in delivery of fertility preservation message to adolescents
with cancer. J Assist Reprod Genet 2011;28:269-77. Crossref
7. Chung JP, Haines CJ, Kong GW. Sperm cryopreservation for Chinese male cancer patients: a 17-year retrospective
analysis in an assisted reproductive unit in Hong Kong.
Hong Kong Med J 2013;19:525-30. Crossref
8. Flink DM, Sheeder J, Kondapalli LA. A review of the oncology patient’s challenges for utilizing fertility
preservation services. J Adolesc Young Adult Oncol
2017;6:31-44. Crossref
9. Liu SS, Chan KY, Leung RC, et al. Prevalence and risk factors of human papillomavirus (HPV) infection in
Southern Chinese women—a population-based study.
PLoS One 2011;6:1-7. Crossref
10. Chung JP, Lao TT, Li TC. Evaluation of the awareness of, attitude to, and knowledge about fertility preservation in
cancer patients among clinical practitioners in Hong Kong.
Hong Kong Med J 2017;23:556-61. Crossref
11. Bretherick KL, Fairbrother N, Avila L, Harbord SH, Robinson WP. Fertility and aging: do reproductive-aged
Canadian women know what they need to know? Fertil
Steril 2010;93:2162-8. Crossref
12. Vujčić I, Radičević T, Dubljanin E, Maksimović N, Grujičić S. Serbian medical students’ fertility awareness and
attitudes towards future parenthood. Eur J Contracept
Reprod Health Care 2017;22:291-7. Crossref
13. Anspach Will E, Maslow BS, Kaye L, Nulsen J. Increasing awareness of age-related fertility and elective fertility
preservation among medical students and house staff:
a pre- and post-intervention analysis. Fertil Steril 2017;107:1200-5.e1. Crossref
14. Hickman LC, Fortin C, Goodman L, Liu X, Flyckt R. Fertility and fertility preservation: knowledge, awareness
and attitudes of female graduate students. Eur J Contracept
Reprod Health Care 2018;23:130-8. Crossref
15. Schwartz D, Mayaux MJ, Spira A, et al. Semen characteristics as a function of age in 833 fertile men. Fertil
Steril 1983;39:530-5. Crossref
16. Chan CH, Chan TH, Peterson BD, Lampic C, Tam MY. Intentions and attitudes towards parenthood and fertility
awareness among Chinese university students in Hong
Kong: a comparison with Western samples. Hum Reprod
2015;30:364-72.Crossref
17. Virtala A, Vilska S, Huttunen T, Kunttu K. Childbearing, the desire to have children, and awareness about the impact of
age on female fertility among Finnish university students.
Eur J Contracept Reprod Health Care 2011;16:108-15. Crossref
18. Yu L, Peterson B, Inhorn MC, Boehm JK, Patrizio P. Knowledge, attitudes, and intentions toward fertility
awareness and oocyte cryopreservation among obstetrics
and gynecology resident physicians. Hum Reprod
2016;31:403-11. Crossref
19. Moss R. Egg freezing is the fastest growing fertility treatment—here’s what you need to know. 2019.
Available from: https://www.huffingtonpost.co.uk/
entry/egg-freezing-is-the-fastest-growing-fertilitytreatment-
heres-what-you-need-to-know-about-it_
uk_5cd1b93ae4b04e275d50f3e0. Accessed 3 Jan 2020.
20. Nilsson MS, Pilhammar E. Professional approaches in clinical judgements among senior and junior doctors:
implications for medical education. BMC Med Educ
2009;9:25. Crossref
21. Healthy Matters. Your Complete guide to egg freezing in Hong Kong. Jun 2019. Available from: https://www.
healthymatters.com.hk/guide-egg-freezing-hong-kongwomen-
need-know-preserving-fertility/. Accessed 3 Jan
2020.
22. Census and Statistics Department, Hong Kong SAR
Government. Table E032: domestic households by
household size and monthly household income (excluding
foreign domestic helpers) [Table 9.4A in Quarterly Report
on General Household Survey]. Population estimates.
2019. Available from: https://www.censtatd.gov.hk/hkstat/
sub/sp150.jsp?productCode=D5250036. Accessed 3 Jan
2020.
23. Mahesan A, Mundt S, Smith L, Stadtmauer L. Knowledge and attitudes regarding elective oocyte cryopreservation
in medical students and undergraduates. Fertil Steril
2017;108:e109-10. Crossref