Hong Kong Med J 2020 Feb;26(1):19–26 | Epub 6 Feb 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Age, sex, and disease status as determinants of skin hydration and transepidermal water loss among children with and without eczema
KL Hon, MB, BS, MD1,2; PH Lam, MSSc, MA1; WG Ng, MPhril1; JS Kung, PhD1; NS Cheng, MNur1; ZX Lin, PhD2; CM Chow, MB, ChB3; TF Leung, MB, ChB, MD1,4
1 Department of Paediatrics, The Chinese University of Hong Kong, Shatin, Hong Kong
2 The Hong Kong Institute of Integrative Medicine, The Chinese University of Hong Kong, Shatin, Hong Kong
3 Department of Paediatrics, Prince of Wales Hospital, Shatin, Hong Kong
4 Hong Kong Hub of Paediatric Excellence, The Chinese University of Hong Kong, Shatin, Hong Kong
Corresponding author: Dr KL Hon (ehon@hotmail.com)
Abstract
Purpose: Skin hydration (SH) and transepidermal water loss (TEWL) are important skin biophysical parameters for assessment of childhood eczema. This study investigated whether age, sex, and disease status influence these parameters.
Methods: Skin hydration and TEWL were measured by Delfin MoistureMeterSC and Delfin Vapometer SWL5, respectively, among children aged ≤18 years with and without eczema. Disease status was evaluated using Scoring Atopic Dermatitis (SCORAD) and Nottingham Eczema Severity Score (NESS) clinical tools.
Results: Clinical scores and objective measurements were reviewed for 132 patients with eczema and 120 patients without eczema. In both sexes, SH was significantly higher among children aged ≤2 years with and without eczema than among children aged >2 years with and without eczema. Among children aged >2 years, SH was higher among girls with and without eczema than among boys with and without eczema. Regardless of age or sex, SH was lower among children with eczema than among children without eczema. Age-, sex-, and disease-related differences were not observed for TEWL. Skin hydration was negatively correlated with objective SCORAD (r=-0.418, P<0.001), overall SCORAD (r=-0.385, P<0.001), oedema/papulation (r=-0.243, P=0.041), lichenification (r=-0.363, P=0.002), dryness (r=-0.415, P<0.001), and intensity (r=-0.266, P=0.025). Transepidermal water loss was positively correlated with objective SCORAD (r=0.209, P=0.018), overall SCORAD (r=0.215, P=0.015), and lichenification (r=0.240, P=0.043). Skin hydration was negatively correlated with TEWL among children without eczema (r=-0.401, P<0.001), but not among children with eczema.
Conclusion: Skin hydration can be used to distinguish clinical differences in eczema based on age, sex, and disease status.
New knowledge added by this study
- Skin hydration was lower in children with eczema than in children without eczema and generally decreased with age, especially in patients with more severe disease.
- Among children aged >2 years, skin hydration was generally higher in girls than in boys.
- Age-, sex-, and disease-related differences were not observed with respect to transepidermal water loss.
- Skin hydration and transepidermal water loss both were correlated with eczema severity, as measured by the SCORAD clinical tool.
- Skin hydration can be used to distinguish clinical differences in eczema based on age, sex, and disease status.
- The effects of age and sex on skin hydration should be considered in research studies and in clinical treatment of patients with eczema.
- Caregivers for children with eczema should receive information regarding the effects of age and sex on skin hydration.
Introduction
Eczema is a prevailing childhood dermatological disease associated with skin dryness and impaired quality of life.1 2 3 4 Eczema, particularly during disease flare-ups, is typically characterised by unbearable itchiness, sleep disturbance, erythematous rash, dryness, and inflammation.1 5 6 In the clinical setting, subjective and objective assessments are used in combination to evaluate eczema disease severity.7 8
SCORing Atopic Dermatitis (SCORAD) is a clinical tool often used to evaluate disease severity.7 9 Eczematous areas and intensity of eczema are recorded; these are considered the objective components in SCORAD (ie, objective SCORAD). Subjective symptoms including the degree of skin itchiness and sleep disturbance due to skin itchiness are also recorded to determine the overall SCORAD assessment outcome.10 Nottingham Eczema Severity Score (NESS) is a clinical assessment tool that adopts subjective and objective approaches for evaluation of the severity of eczema.4 7 11 12 Using an assessment form, patients record their symptoms of sleep impairment due to skin itchiness in terms of the number of nights and length of the presence of eczematous symptoms within the previous 12 months; they also report the areas of eczematous skin.11 In Hong Kong, a validated Chinese version of the NESS is used.12
In addition to clinical scores, skin measurements including skin hydration (SH) and transepidermal water loss (TEWL) are important indicators of the barrier function of the skin.8 13 Skin hydration and TEWL measurements have been shown to correlate with eczema severity and quality of life impairment.8 13 Measurements of these non-invasive parameters may be useful in prognostic prediction of the development of eczema in infants14; these parameters have been use in Hong Kong as auxiliary tools in eczema therapeutic trials.7 8 15 16 To the best of our knowledge, there have been no studies in Hong Kong regarding the influences of age and sex on these parameters. This study aimed to compare the age and sex of Chinese children with and without eczema in terms of SH and TEWL, and to evaluate the correlations of SH and TEWL with clinical scores.
Methods
Patient recruitment
Chinese patients with eczema, who were aged 4 weeks to 18 years and were attending the paediatric dermatology clinic at Prince of Wales Hospital, were recruited from July 2018 to October 2018. Eczema was diagnosed in accordance with the United Kingdom working diagnosis.9 In addition, Chinese patients without eczema (eg, naevi or warts), aged 4 weeks to 18 years, were also recruited from the same paediatric dermatology clinic at Prince of Wales Hospital during the study period. Patients without eczema were defined as those who had not been clinically diagnosed with eczema in their medical history. Patients and their caregivers received an explanation of the details of the study including its aim and procedures, as well as each patient’s rights and possible risks related to involvement in the study. Written informed consent for participating in the overall study was obtained from patients or caregivers before enrolment in the study. Patients were then separated into two groups; those with a current or prior clinical diagnosis of eczema were regarded as children with eczema, while those without clinically diagnosed eczema were regarded as children without eczema. Both children with and without eczema underwent the same study measurements and received the same treatment procedures throughout the study.
Clinical assessment of eczema
Eczema was routinely assessed by clinicians using the SCORAD tool.9 10 The overall SCORAD assessment outcome was determined by two objective components and one subjective component. The extent of eczematous areas involved were assessed by observing patient’s eczematous body surface area covering head and neck (9%), bilateral upper limbs (9% each), bilateral lower limbs (18% each), anterior trunk (18%), back (18%) and genitals (1%), which were aggregated to 100% of whole body surface areas. Intensity of dermatological lesions was assessed by indicating none (0), mild (1), moderate (2) and severe (3) onto the eczematous areas in terms of six categories: redness, swelling, oozing/crust, excoriation, lichenification, and dryness on non-eczematous areas. The score of intensity of dermatological lesions was obtained by adding up the scores of these six categories. Subjective components of SCORAD were assessed by evaluation of subjective symptoms (ie, pruritus and sleep loss) over the course of the previous three nights, which were rated on a scale from 0 to 10.9 10 Objective SCORAD scores <15, 15 to 40, and >40 were classified as mild, moderate, and severe disease, respectively; overall SCORAD scores <25, 25 to 50, and >50 were classified as mild, moderate, and severe disease, respectively.9 10 17 Both overall SCORAD and objective SCORAD scores were used in this study. The NESS tool was also used to determine the severity of eczema.11 18 With respect to the past 12 months, the duration of eczema and number of nights impacted by skin itchiness weekly were rated from 1 to 5. A higher score indicated greater eczema severity. In addition, areas of skin with eczematous lesions (eg, rash, lichenified skin, and/or bleeding) were recorded. Scores ranging from 3 to 8, 9 to 11, and 12 to 15 were categorised as mild, moderate, and severe disease.11 The validated Chinese version of the NESS was used.12
Equipment-based skin measurements
Patients were first taken to an air-conditioned treatment room and rested for 20 minutes. All children included in this study (regardless of the presence or absence of eczema) reported no use of emollient in any form within 24 hours prior to the skin measurements. Skin hydration was measured topically using the MoistureMeterSC (Delfin Technologies Ltd., Kuopio, Finland) at a standard site 2 cm below the antecubital fossa of each patient’s right arm.8 13 The SH is measured in arbitrary units (a.u.), which range from 0 to 300 a.u. The MoistureMeterSC serves as a capacitance meter, measuring the skin capacitance detected from the probe head of equipment onto the skin surface layer, based on the relationship between skin capacitance and the water content of the surface layer of skin19 20; a higher SH value indicates greater skin moisture. Transepidermal water loss was topically measured using the Vapometer SWL5 (Delfin Technologies Ltd.) at the same standard site 2 cm below the antecubital fossa of each patient’s right arm.8 13 The TWEL is measured in g/m2h, which range from 0 to 300. The Vapometer is equipped with a closed cylindrical chamber containing sensors which detect changes in relative humidity and temperature after placement on the skin surface. The TEWL is then measured based on the change in relative humidity19 20; an increasing TEWL value indicates greater skin dryness. Skin measurements were conducted by trained research personnel, and fewer than 5 minutes were required to complete both procedures. During the measurements, no psychological or physiological discomforts occurred.
Statistical analyses
Clinical data were de-identified and analysed using SPSS Statistics for Windows, version 25.0 (IBM Corp, Armonk [NY], US). Frequency distributions were used to describe patients’ demographic data. Independent-samples t tests were used to compare SH and TEWL between patients in terms of sex, age, and presence or absence of disease. Pearson correlation was used to investigate associations between skin measurements and SCORAD subcategories. Trend analysis was performed regarding the effects of age on SH. Multiple regression model of the interactions of SH and TEWL with age and sex in children with and without eczema was done. P values <0.05 were considered statistically significant and 95% confidence intervals were adopted for all statistical comparisons in this study.
Results
Patient characteristics
In total, datasets of clinical scores (SCORAD) and equipment measurements were reviewed for 252 patients during the period from August 2018 to October 2018. Among the 252 patients (mean age, 5.84±5.97 years; 52.0% boys), 132 were children with eczema (mean age, 7.05±6.60 years; 52.3% boys), while 120 were children without eczema (mean age, 4.52±4.91 years; 51.7% boys). Furthermore, 121 patients were aged ≤2 years, while 131 patients were aged >2 years.
Age-related changes in skin hydration
Table 1 shows that, among children with eczema (n=132), the mean SH of boys aged ≤2 years was significantly higher than the mean SH of boys aged >2 years (P<0.001). Similarly, the mean SH of girls aged ≤2 years was significantly higher than the mean SH of girls aged >2 years (P<0.001). Among children without eczema (n=120), the mean SH of boys aged ≤2 years was significantly higher than the SH of boys aged >2 years (P=0.046). However, no statistically significant difference in SH (P=0.980) was observed in comparisons between girls aged ≤2 years and girls aged >2 years. These results demonstrated that SH significantly differed in an age-related manner among both boys and girls with eczema.
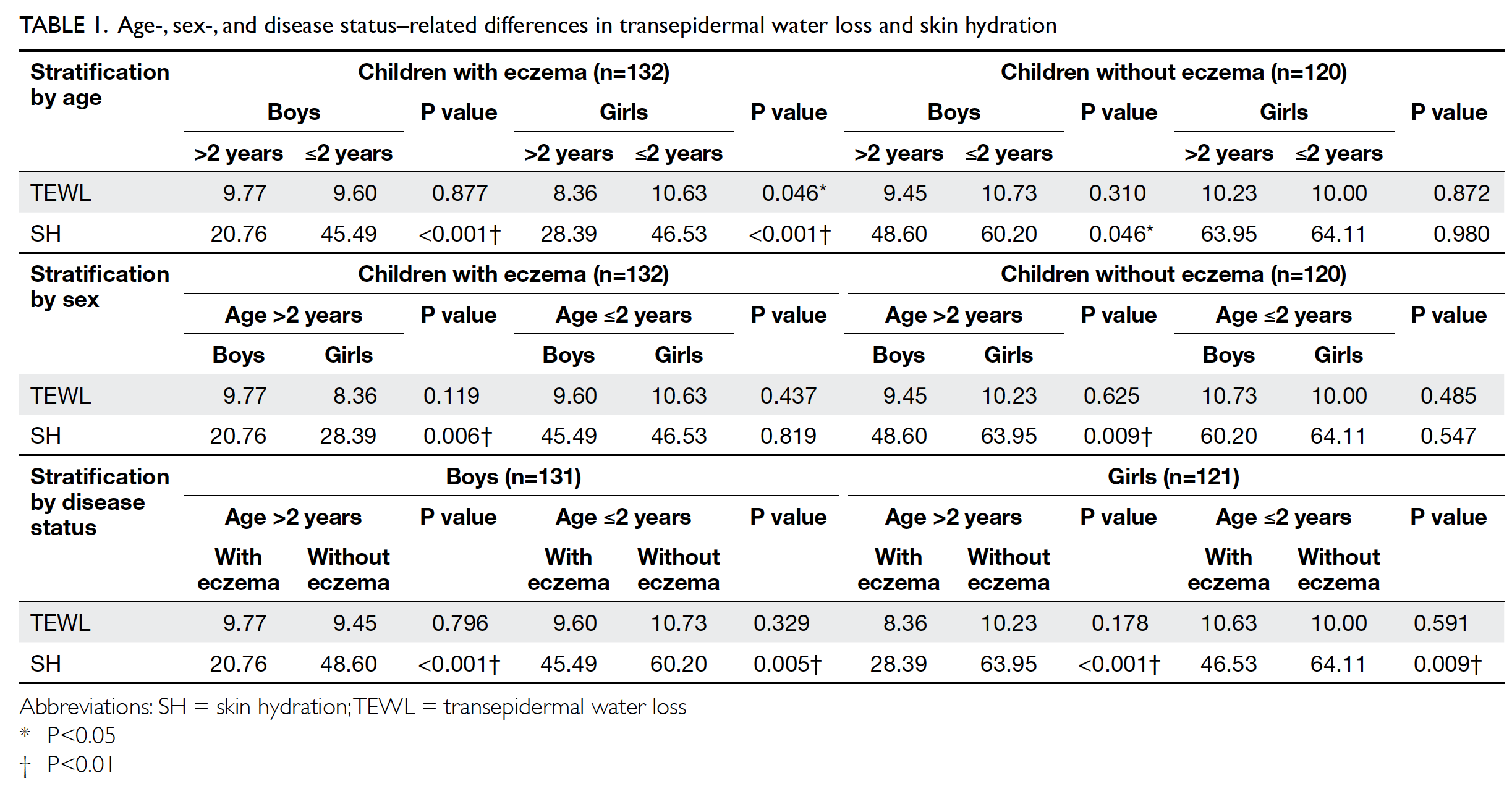
Table 1. Age-, sex-, and disease status–related differences in transepidermal water loss and skin hydration
Sex-related changes in skin hydration
Table 1 shows that, among children with eczema (n=132), the mean SH of girls aged >2 years was significantly higher than the mean SH of boys aged >2 years (P=0.006). Similarly, among children without eczema, the mean SH of girls aged >2 years was significantly higher than the mean SH of boys aged >2 years (P=0.009). However, in both children with eczema and children without eczema, there were no sex-related differences in SH among patients aged ≤2 years. These results demonstrated that SH significantly differed in a sex-related manner among patients aged >2 years, regardless of the presence or absence of eczema.
Disease status–related changes in skin hydration
Table 1 shows that, among boys in this study (n=131), the mean SH of children with eczema aged >2 years was significantly lower than the mean SH of children without eczema aged >2 years (P<0.001). Furthermore, the mean SH of boys with eczema aged ≤2 years was significantly lower than the mean SH of boys without eczema aged ≤2 years (P=0.005). Similarly, among girls in this study (n=121), the mean SH of children with eczema aged >2 years was significantly lower than the mean SH of children without eczema aged >2 years (P<0.001). In addition, the mean SH of girls with eczema aged ≤2 years was significantly lower than the mean SH of girls without eczema aged ≤2 years (P=0.009). The results showed that SH was consistently higher in children without eczema than in children with eczema, regardless of age and sex.
Relationships of skin hydration with clinical scores and objective measurements
Among children with eczema (Table 2; n=132), Pearson correlation demonstrated that SH was significantly negatively correlated with objective SCORAD (P<0.001), overall SCORAD (P<0.001), oedema/papulation (P=0.041), lichenification (P=0.002), dryness (P<0.001), and intensity (P=0.025). In addition, Pearson correlation demonstrated that TEWL was significantly positively correlated with objective SCORAD (P=0.018), overall SCORAD (P=0.015), and lichenification (P=0.043). No significant correlation was observed between TEWL and SH (P=0.565) in children with eczema, whereas a correlation was present in children without eczema (P<0.001).
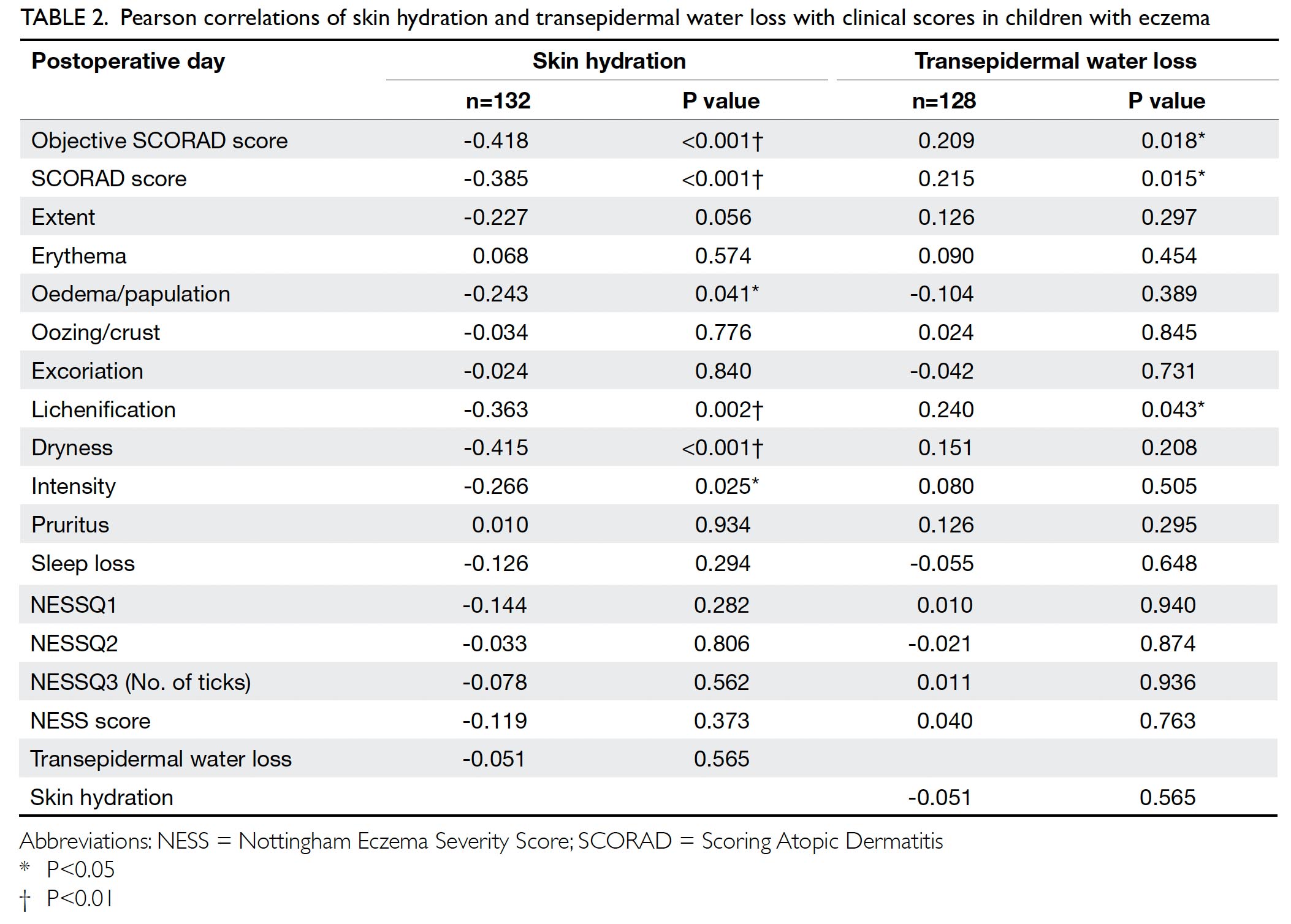
Table 2. Pearson correlations of skin hydration and transepidermal water loss with clinical scores in children with eczema
Effects of age on skin hydration
Trend analysis revealed a marked decline in SH during the first 50 months of life among children with eczema, relative to children without eczema (Fig). Beginning at 51 months of age, the magnitude of SH began to gradually decline. Conversely, for children without eczema, a slight, steady decline in SH was observed in the first 50 months of life.
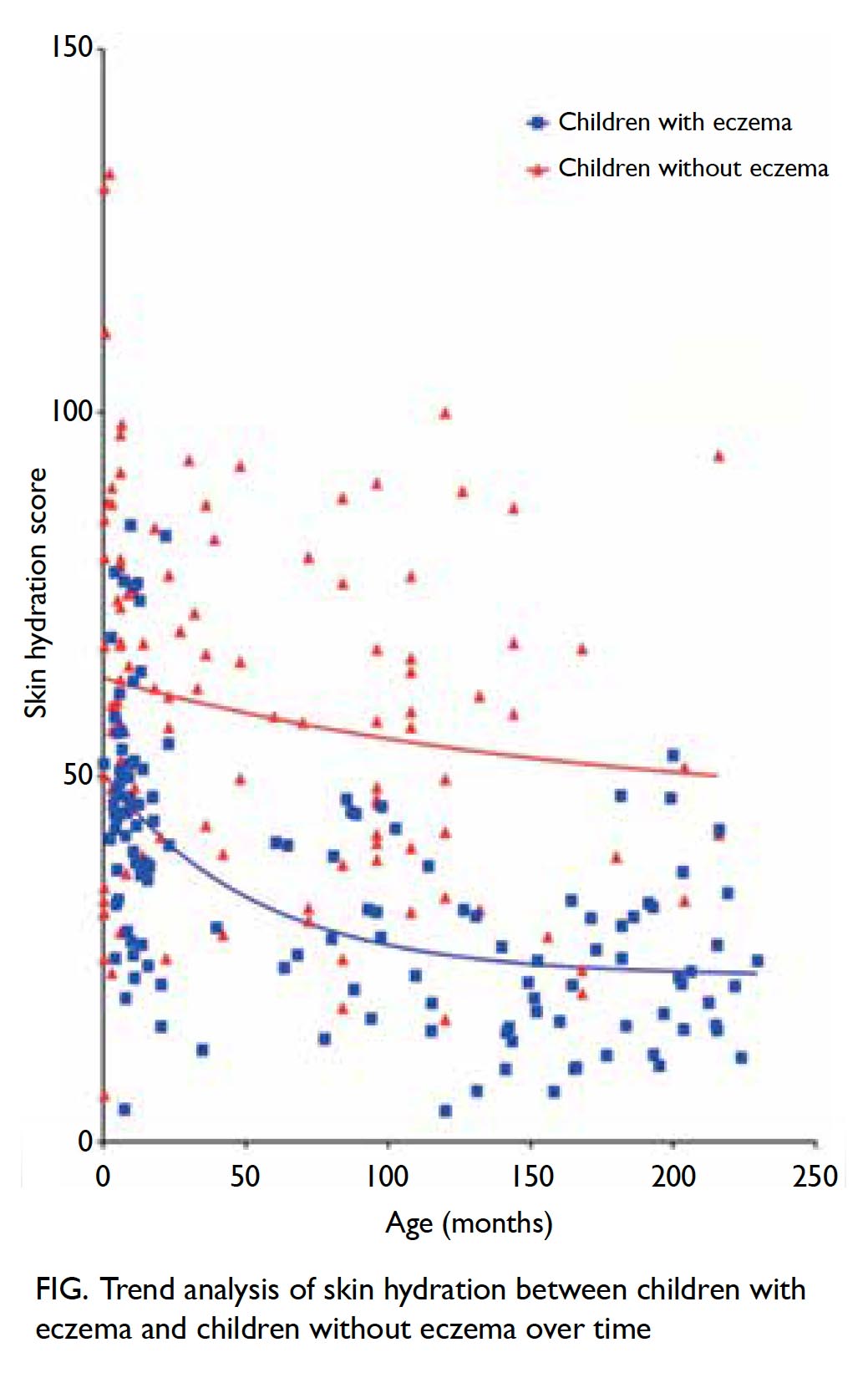
Figure. Trend analysis of skin hydration between children with eczema and children without eczema over time
Age-related changes in transepidermal water loss
Table 1 shows that, among children with eczema (n=132), the mean TEWL of girls aged ≤2 years was significantly higher than the mean TEWL of girls aged >2 years (P=0.046). However, no statistically significant difference in TEWL (P=0.877) was observed in comparisons between boys aged ≤2 years and boys aged >2 years. Similarly, among both boys and girls without eczema in this study, no statistically significant difference in TEWL was found between children aged ≤2 years and children aged >2 years. The findings demonstrated that TEWL was affected by age only among girls with eczema.
Sex- and disease status–related changes in transepidermal water loss
Regardless of age and disease status, no statistically significant difference in TEWL was found between boys and girls (Table 1). Likewise, regardless of age and sex, no statistically significant difference in TEWL was found between children with eczema and children without eczema. The results showed that TEWL did not significantly differ among patients based on sex, age, or disease status.
Impacts of age and sex on skin hydration
Multiple regression models were constructed with TEWL and SH as the outcome variables, using age and sex as independent predictors, to examine the effects of the age and sex interaction on TEWL and SH in children with and without eczema. Table 3 shows that, among children without eczema, the age×sex interaction term could explain 40.9% of the variance in SH (P=0.031); however, the age×sex interaction term could not explain the variance in SH (P=0.290) among children with eczema. In addition, when used as a predictive variable, age could not explain the variance in SH among children with eczema (P=0.364) or among children without eczema (P=0.143). Similarly, when used as a predictive variable, sex could not explain the variance in SH among children with eczema (P=0.377) or among children without eczema (P=0.132). These results showed that the interaction between age and sex significantly affected SH among children without eczema, but not among children with eczema; when considered alone, neither age nor sex significantly affected SH among any of the children in the study.
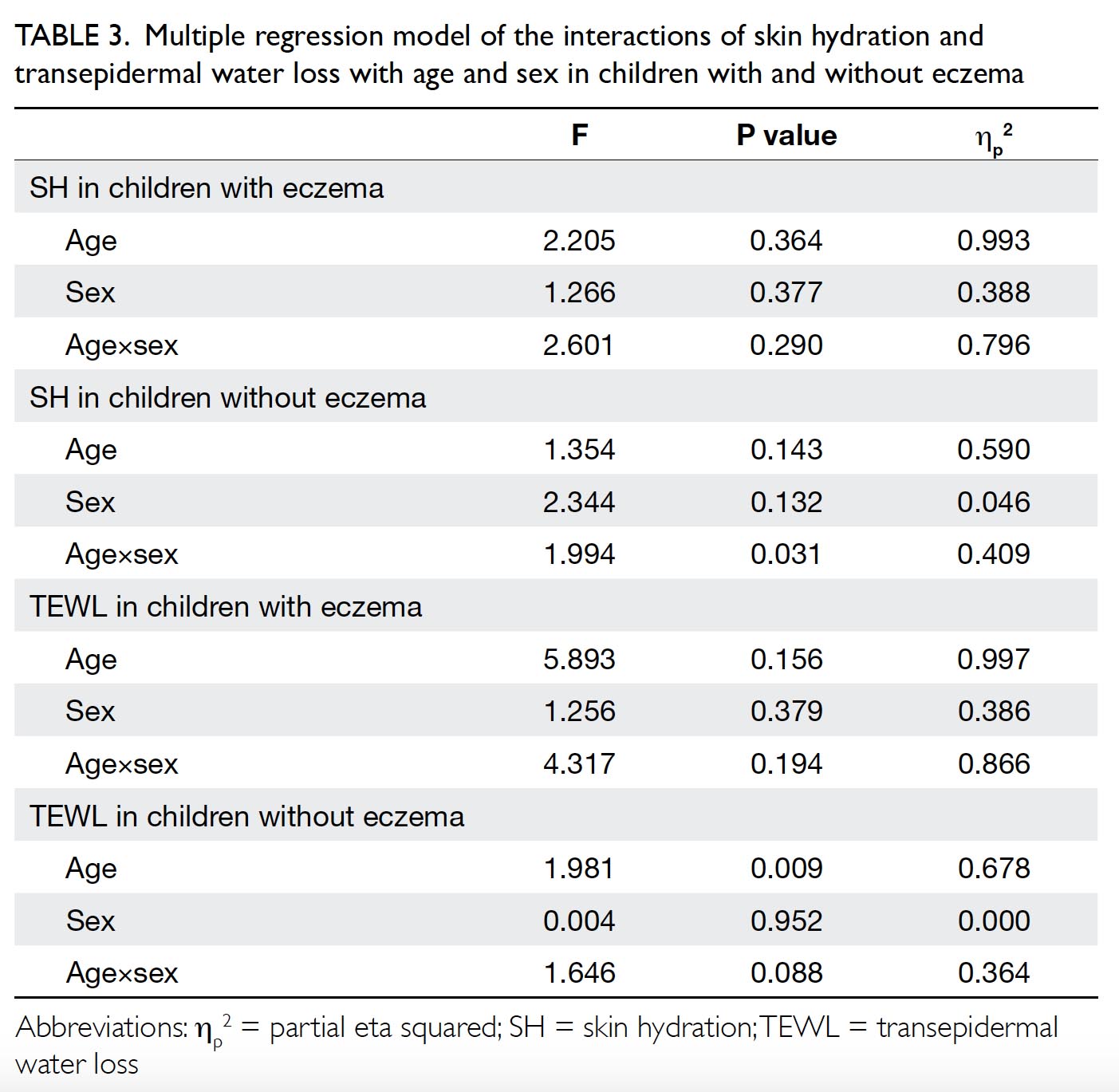
Table 3. Multiple regression model of the interactions of skin hydration and transepidermal water loss with age and sex in children with and without eczema
Impacts of age and sex on transepidermal water loss
In contrast, Table 3 shows that, when used as a predictive variable, age could explain 67.8% of the variance in TEWL (P=0.009) among children without eczema, but could not explain the variance in TEWL (P=0.156) among children with eczema. In addition, when used as a predictive variable, sex could not explain the variance in TEWL among children with eczema (P=0.379) or among children without eczema (P=0.952). Similarly, the age×sex interaction term could not explain the variance in TEWL among children with eczema (P=0.194) or among children without eczema (P=0.088). These results showed that age alone significantly affected TEWL among children without eczema, but not among children with eczema; sex alone and the age×sex interaction term did not significantly affect TEWL among any of the children in the study.
Discussion
Skin hydration and TEWL are useful auxiliary tools in assessment of adult eczema for research purposes.8 13 21 The findings in this study confirmed our previous observations that SH and TEWL were correlated with disease severity (ie, objective SCORAD and overall SCORAD) in paediatric patients with eczema.13 As SH declines (ie, skin dryness increases), the clinical scores of objective SCORAD and overall SCORAD increase, indicating more severe eczema. Furthermore, as TEWL increases (ie, skin loses water through the epidermis), the clinical scores of objective SCORAD and overall SCORAD increase, indicating more severe eczema. In our study, SH and TEWL were also correlated with lichenification, which is an indicator of the chronicity of eczema.13 21 This study also demonstrated that age and sex could influence SH, but not TEWL. First, SH was significantly lower in children with eczema than in children without eczema, regardless of age or sex; no such difference was demonstrated with respect to TEWL. Second, SH was generally higher in young children, whereas TEWL did not differ on the basis of age. Hence, researchers should consider these relationships when interpreting SH measurements in infants.
Skin hydration was lower in children with eczema than in children without eczema (Fig). Trend analysis showed that SH declined more markedly in children with eczema than in children without eczema during the first 2 years of life. This phenomenon might reflect the onset and progression of eczema in early life. Skin hydration was correlated with skin dryness and lichenification (Table 2). With disease progression, skin dryness increases and lichenification develops as a sign of chronicity. Therefore, age is a key factor that affects SH and eczema severity. Among children aged >2 years, SH was higher in girls than in boys, regardless of the presence or absence of eczema. This universal phenomenon might be related to sex differences in cutaneous physiology. Furthermore, the observation of a sex difference in SH suggests that skin is less dry and more manageable with emollients in girls, compared with boys. We previously studied quality of life in children with eczema and found that not all aspects of quality of life were affected equally in children with eczema.22 Age and sex were important in that clothes/shoes caused more problems for girls, whereas itching and sleep disturbance primarily affected younger children. In addition, eczema damaged the epidermal layer of skin and caused greater self-image difficulties in girls than in boys, especially during childhood and adolescence. These findings indicated that psychosocial influences should be considered among patients with eczema. Notably, age influenced SH and TEWL among children without eczema. Although regression analysis showed that age was not a significant predictor of SH or TEWL among children with eczema, the partial eta squared (ηp2) for age was high, which suggested that it may explain some variance in both SH and TEWL. Thus, age should be considered in further studies of SH and/or TEWL.
The design and findings of this study were quite different from those in studies by Walters et al and Kong et al.23 24 The participants in the study by Walters et al were mainly Caucasian, while those in the study by Kong et al were mainland Chinese.23 In addition, the study by Kong et al was conducted in winter, such that the temperature and relative humidity were extremely low.24 Hong Kong is a subtropical climate and the skin measurements in the present study were performed using an established standard protocol. In addition, both prior studies focused on comparisons between children without eczema and their mothers. In contrast, our study compared SH and TEWL between children with eczema and children without eczema. Furthermore, our study showed the following: SH was significantly higher among both boys and girls aged ≤2 years than among boys and girls aged >2 years, regardless of the presence or absence of eczema; this age-related difference was not observed with respect to TEWL. Among children aged >2 years, SH was higher among girls with and without eczema than among boys with and without eczema; this sex-related difference was not observed with respect to TEWL. Regardless of age and sex, SH was lower among children with eczema than among children without eczema; this disease status-related difference was not observed with respect to TEWL. Hence, we concluded that age and sex affect SH. Kong et al24 also demonstrated a more permeable skin barrier in younger children, compared with both older children and adults. Potential underlying reasons for the findings in our study require further investigation because of the cross-sectional study design and limited sample size.
There were some limitations in this study. First, the sample size was small and did not allow in-depth subgroup analysis of children with eczema or children without eczema; thus, our findings cannot be used to establish age-based population norms for the assessment parameters used in this study. Second, the recruitment of patients was restricted to a single site; thus the sample may not have been representative of the population, and the generalisability of the results may be limited. Finally, the efficacy of skin barrier treatment was not evaluated. Future studies should address these limitations and confirm our findings.
Conclusion
This study investigated the effects of age and sex on SH and TEWL in children with and without eczema. Skin hydration was lower in children with eczema than in children without eczema and generally decreased with age, especially during infancy and in patients with more severe disease. Among children aged >2 years, SH was generally higher in girls than in boys. Thus, we presume that SH can be used to distinguish clinical differences in eczema based on age, sex, and disease status.
Author contributions
Concept or design: KL Hon.
Acquisition of data: PH Lam, WG Ng, JS Kung.
Analysis or interpretation of data: PH Lam.
Drafting of the article: KL Hon, PH Lam.
Critical revision for important intellectual content: KL Hon, WG Ng, JS Kung, NS Cheng, ZX Lin, CM Chow, TF Leung.
Acquisition of data: PH Lam, WG Ng, JS Kung.
Analysis or interpretation of data: PH Lam.
Drafting of the article: KL Hon, PH Lam.
Critical revision for important intellectual content: KL Hon, WG Ng, JS Kung, NS Cheng, ZX Lin, CM Chow, TF Leung.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the peer review process. Other authors have no conflicts of interest to disclose.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical Research Ethics Committee (Ref CRE.2016.118). Written informed consent to participate was obtained from patients or caregivers before enrolment in the study.
References
1. Leung TN, Hon KL. Eczema therapeutics in children: what do the clinical trials say? Hong Kong Med J 2015;21:251-60. Crossref
2. Hon KL, Yong V, Leung TF. Research statistics in atopic eczema: what disease is this? Ital J Pediatr 2012;38:26. Crossref
3. Leung AK, Hon KL, Robson WL. Atopic dermatitis. Adv Pediatr 2007;54:241-73. Crossref
4. Hon KL, Kam WY, Lam MC, Leung TF, Ng PC. CDLQI, SCORAD and NESS: are they correlated? Qual Life Res 2006;15:1551-8. Crossref
5. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol 1980;92(Suppl):44-7.
6. Hanifin JM. Diagnostic criteria for atopic dermatitis: consider the context. Arch Dermatol 1999;135:1551.
7. Hon KL, Kung JS, Tsang KY, Yu JW, Cheng NS, Leung TF. Do we need another symptom score for childhood eczema? J Dermatolog Treat 2018;29:510-4. Crossref
8. Hon KL, Kung J, Ng WG, Tsang K, Cheng NS, Leung TF. Are skin equipment for assessing childhood eczema any good? J Dermatolog Treat 2018;20:1-15. Crossref
9. Severity scoring of atopic dermatitis: the SCORAD index. Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology 1993;186:23-31. Crossref
10. Kunz B, Oranje AP, Labrèze L, Stalder JF, Ring J, Taïeb A. Clinical validation and guidelines for the SCORAD index: consensus report of the European Task Force on Atopic Dermatitis. Dermatology 1997;195:10-9. Crossref
11. Emerson RM, Charman CR, Williams HC. The Nottingham Eczema Severity Score: preliminary refinement of the Rajka and Langeland grading. Br J Dermatol 2000;142:288-97. Crossref
12. Hon KL, Ma KC, Wong E, Leung TF, Wong Y, Fok TF. Validation of a self-administered questionnaire in Chinese in the assessment of eczema severity. Pediatr Dermatol. 2003;20:465-9. Crossref
13. Hon KL, Wong KY, Leung TF, Chow CM, Ng PC. Comparison of skin hydration evaluation sites and correlations among skin hydration, transepidermal water loss, SCORAD Index, Nottingham Eczema Severity Score, and quality of life in patients with atopic dermatitis. Am J Clin Dermatol 2008;9:45-50. Crossref
14. Horimukai K, Morita K, Narita M, et al. Transepidermal water loss measurement during infancy can predict the subsequent development of atopic dermatitis regardless of filaggrin mutations. Allergol Int 2016;65:103-8.
15. Hon KL, Tsang YC, Pong NH, et al. Patient acceptability, efficacy, and skin biophysiology of a cream and cleanser containing lipid complex with shea butter extract versus a ceramide product for eczema. Hong Kong Med J 2015;21:417-25. Crossref
16. Luk NM, Lee HC, Hon KL, Ishida K. Efficacy and safety of pseudo-ceramide containing moisture cream in the treatment of senile xerosis. Hong Kong J Dermatol Venereol 2009;17:181-4.
17. Chopra R, Vakharia PP, Sacotte R, et al. Severity strata for Eczema Area and Severity Index (EASI), modified EASI, Scoring Atopic Dermatitis (SCORAD), objective SCORAD, Atopic Dermatitis Severity Index and body surface area in adolescents and adults with atopic dermatitis. Br J Dermatol 2017;177:1316-21. Crossref
18. Charman C, Williams H. Outcome measures of disease severity in atopic eczema. Arch Dermatol 2000;136:763-9. Crossref
19. du Plessis J, Stefaniak A, Eloff F, et al. International guidelines for the in vivo assessment of skin properties in non-clinical settings: Part 2. Transepidermal water loss and skin hydration. Skin Res Technol 2013;19:265-78. Crossref
20. Pinnagoda J, Tupker RA, Agner T, Serup J. Guidelines for transepidermal water loss (TEWL) measurement. A report from the Standardization Group of the European Society of Contact Dermatitis. Contact Dermatitis 1990;22:164-78. Crossref
21. Lio PA. Efficacy of a moisturizing foam in skin barrier regeneration and itch relief in subjects prone to atopic dermatitis. J Drugs Dermatol 2016;15:s77-80. Crossref
22. Hon KL, Leung TF, Wong KY, Chow CM, Chuh A, Ng PC. Does age or gender influence quality of life in children with atopic dermatitis? Clin Exp Dermatol 2008;33:705-9. Crossref
23. Walters RM, Khanna P, Chu M, Mack MC. Developmental changes in skin barrier and structure during the first 5 years of life. Skin Pharmacol Physiol 2016;29:111-8. Crossref
24. Kong F, Galzote C, Duan Y. Change in skin properties over the first 10 years of life: a cross-sectional study. Arch Dermatol Res 2017;309:653-8. Crossref

