© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REMINISCENCE: ARTEFACTS FROM THE HONG KONG MUSEUM OF
MEDICAL SCIENCES
Triturator for smallpox vaccine production
Harry YJ Wu, MD, DPhil
Medical Ethics and Humanities Unit, Li Ka Shing
Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong
The triturator that was used to produce smallpox
and rabies vaccines was donated by the Hong Kong Government Department of
Health in 1995. This decommissioned device witnessed an important moment
in the history of disease prevention in Hong Kong. According to the World
Health Organization, there have been no smallpox cases in Hong Kong since
1952. Hong Kong was further certified disease free in 1979, 2 years before
the worldwide eradication. Despite this, the story that the machine tells
is an unfinished one, owing to perpetual speculation about whether Hong
Kong would have been able to prevent contagious diseases on its own.
The triturator, measuring 32 cm tall and 21.5 cm in
diameter, was produced in Lausanne, Switzerland. It was used in the
processing of Semple-type vaccines, such as for smallpox and rabies
vaccine between 1940 and 1982. Usually, lymph pulp of calves was fed into
the machine with glycerine through the conical copper funnel on the top.
The tissue then passed through the central copper grinding spindle before
the emulsion was collected via a key in two lower crescent-shaped
stainless steel cups. The grinder was powered by an electric motor under
the marble table (Fig). To prevent contamination, the equipment was
protected with a wood-framed glass hood. In general, calves were the most
commonly used animals for producing smallpox vaccine. In Hong Kong,
buffalo calves were originally kept in the Animal House of the
Bacteriological Institute, before the house was demolished to become Caine
Lane Garden.
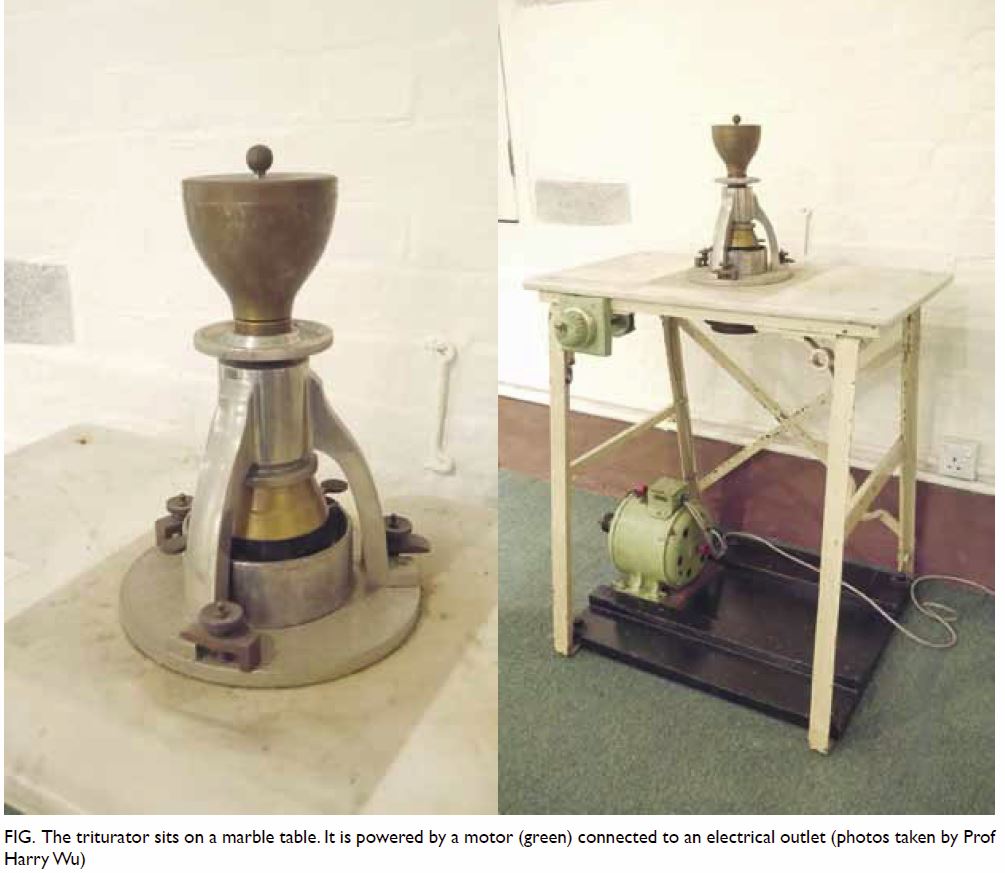
Figure. The triturator sits on a marble table. It is powered by a motor (green) connected to an electrical outlet (photos taken by Prof Harry Wu)
In Hong Kong’s medical history, credentials are
given to a number of individuals regarding the development of smallpox
vaccination technology, for example, Alexander Pearson, a surgeon working
for the East India Company in the early 19th century, who practised
vaccination in Macao; Pearson’s student, Yao Hochun, known as A-Hequa by
Westerners, who published a book on vaccination in 1817; and William James
Woodman, Medical Officer of Health, who scaled up the vaccination
campaigns among Chinese through Tung Wah Hospital and the Chinese Public
Dispensaries in 1916.1 Smallpox
vaccination could not have been successful without these important
figures. However, history tells us how disease onset, development, and
control were contingent upon factors beyond the individual sagas of these
heroes.
Smallpox had been a common disease among Chinese.
It mostly affected young children and people who did not have strong
immune systems. It is documented that in the Ming and Qing
dynasties in China, measures were taken to survey the disease and avoid
infection.2 More precisely, around
the 16th or 17th centuries, inoculation techniques had already been
developed for prevention. Methods, such as insufflating powdered smallpox
crusts, stuffing a cotton pledget impregnated with smallpox scabs into the
nostrils of a child or making a child wear a patient’s unwashed
undergarment for 2 to 3 days, were common. However, when the first
Government Bacteriologist, William Hunter, arrived in Hong Kong, he
considered that such practices, famously known as ‘variolation’, were a
culprit for spreading disease. He also believed that the annual recurrence
of epidemic smallpox would continue in Hong Kong unless China finally
recognised the importance of providing the means for general vaccination
and re-vaccination.3 Such
accusations of Chinese antipathy towards Western vaccination measures
continued throughout various outbreaks.4
In the early days, compliance with public health measures could not have
been smoothed without the support of well-organised neighbourhood
organisations (kaifong) and public health educators from Chinese
Public Dispensaries.1
Between 1858 and 1952—the respective dates of the
first and the last reports of smallpox cases in Hong Kong—vaccination was
just one of many measures taken to deal with the endemics resulting from a
variety of social conditions. The effective control and exacerbation of
infectious diseases were both attributed to Hong Kong’s unique geographic
environment. For example, as a peninsula connecting Canton, commercial
travelling was common between the inland and the port, accelerating the
spread of diseases. As an archipelago, smallpox patients had, for a long
period of time, been isolated in the jail on Stonecutters Island. And as a
growing financial and transport hub, Hong Kong had to digest innumerable
travellers en route from rural southern China to Southeast Asia, or across
the Pacific to the United States, at the risk of becoming a
‘redistributive depot’ of diseases.5
In 1938, Tung Wah Smallpox Hospital, which was established in 1908 in
Kennedy Town, was no longer able to accommodate the surging numbers of
smallpox victims caused by refugees fleeing the Sino-Japanese War. The
shutdown of connections between Hong Kong and the important surrounding
ports in the Straits Settlements,6
Amoy,7 and Formosa,8 became one of the inevitable measures for preventing a
foreseeable pandemic.
The vaccine institute in Hong Kong was established
under Governor Des Voeux’s rule in 1891 before it was incorporated into
the Bacteriological Institute in 1906. Within 20 years, the Institute was
already able to produce vaccines against typhoid, paratyphoid, cholera and
meningococcal antiserum.1 During
wartime, Hong Kong had to seek help from the League of Nations for the
supply of smallpox vaccines.9
Products had to arrive by airmail to Hong Kong, passing airports where
quarantines were not implemented to ensure the quality and potency of
vaccines. For example, in February 1938, as reported in the Hong Kong
Telegraph, a shipment of vaccine left Bandung on a KLM plane and was
transhipped to Imperial Airways at Bangkok before arriving in Hong Kong.2 In addition to importation, local
vaccine production and vaccination became more extensive with lymph
obtained locally. Hong Kong even delivered vaccine to naval and military
authorities for the use in neighbouring ports.10
The rise, fall, and eventual disappearance of
smallpox and other contagious diseases in Hong Kong attest to the
complexity of disease prevention. Owing to the drastic decline in smallpox
cases in Hong Kong, the Pathological Institute (the original
Bacteriological Institute) ceased smallpox vaccine production in 1973.11 However, using the smallpox vaccine as an example, we
can see how a simple technological object functioned and how its nature
manifested in a complex society. In 1923, the Vaccination Ordinance
required that ‘any person, who in his opinion [of the Medical Officer of
Health] has been subjected to the risk of infection from smallpox, should
be vaccinated or re-vaccinated’.12
Now, the vaccination policy has become one that emphasises the citizen’s
own health insights and risk-bearing capacity. From an antipathic society
to a hub receiving Chinese medical tourists for various types of
vaccination, Hong Kong is now facing other problems that accompany novel
types of immigration, a more complicated cultural and societal
composition, and growing tension between necessary population flow and the
protection of its own citizens.
References
1. Chan-Yeung MM. A Medical History of Hong
Kong: 1842-1941. Hong Kong: Chinese University of Hong Kong Press; 2017.
2. Hsiung PJ. Ill or Well: Diseases and
Health of Young Children in Late Imperial China. Taipei: Lien-ching; 1999.
3. Hunter W. Report of the Government
Bacteriologist, for the year 1902. Hong Kong: Government Public Mortuary;
1903.
4. New Cases of Smallpox Vaccine Flow Here
by Daedalus. The Hong Kong Telegraph. 2 Feb 1938.
5. Peckham R. Epidemics in Modern Asia.
Cambridge: Cambridge University Press; 2016. Crossref
6. Hong Kong declared an infected port by
the Government of Straits Settlements. Hong Kong Government Gazette 1939
(Supplement), No 7, 6 Jan 1939.
7. Hong Kong declared an infected port by
Amoy. Hong Kong Government Gazette 1938 (Supplement), No 31, 4 Feb 1938.
8. Hong Kong declared an infected port by
the Government of Formosa. Hong Kong Government Gazette 1938 (Supplement),
No 48, 18 Feb 1938.
9. 4,000,000 Smallpox Vaccine Doses. Hong
Kong Sunday Herald. 18 Dec 1938.
10. Wong S. The calf vaccinating table.
Hong Kong Med J 2017;23:101-3.
11. The Bacteriological Institute and its
contributions to Hong Kong. In: Hong Kong Museum of Medical Sciences
Society. Plague, SARS and the Story of Medicine in Hong Kong. Hong Kong:
Hong Kong University Press; 2006:147-224.
12. Legislative Council, Draft Bill: An
Ordinance to consolidate and amend the law relating to Vaccination. Hong
Kong Government Gazette; 1922:176.

