Hong
Kong Med J 2018 Dec;24(6):602–9 | Epub 3 Dec 2018
DOI: 10.12809/hkmj187513
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE
Epidemiology of myopia and prevention of myopia
progression in children in East Asia: a review
CY Mak, MB, BS, MRCSEd (Ophth)1,2;
Jason CS Yam, FRCS (Edin), FCOphth HK2; LJ Chen, MRCSEd
(Ophth), PhD1,2; SM Lee, MB BCh BAO, DFM3; Alvin L
Young, FRCOphth, FHKAM (Ophthalmology)1,2
1 Department of Ophthalmology and Visual
Sciences, Prince of Wales Hospital, Shatin, Hong Kong
2 Department of Ophthalmology and Visual
Sciences, The Chinese University of Hong Kong, Shatin, Hong Kong
3 Private Practice
Corresponding author: Prof Alvin L Young (youngla@ha.org.hk)
Abstract
Introduction: Myopia
(short-sightedness) exhibits high prevalence in East Asia. Methods to
mitigate myopia progression are important in preventing the
vision-threatening complications associated with high myopia. In this
review, we examine the regional epidemiology of myopia and provide
updated evidence regarding interventions to slow myopia progression in
children.
Methods: We performed a
literature search using PubMed from the date of inception through 25
June 2018. Studies involving myopia epidemiology and control of myopia
progression were selected; only studies published in English were
reviewed. Preference was given to prospective studies, as well as those
conducted in Hong Kong or East Asia.
Results: Atropine eye drops and
pirenzepine eye gel are highly effective for controlling myopia
progression in children. Orthokeratology, peripheral defocus contact
lenses, bifocal or progressive addition spectacles, and increased
involvement in outdoor activities are also effective for controlling
myopia progression; however, myopia undercorrection and single vision
contact lenses are ineffective.
Conclusion: Although various
methods are effective for controlling myopia progression in children, no
curative remedy exists for myopia. Health care professionals should be
aware of the available methods, as well as their risks and benefits.
Treatment should be individualised and based on the preferences of the
patient’s family, after full discussion of the risks and
benefits of each modality.
Introduction
Myopia is a prevalent eye disorder in children and
adolescents in Hong Kong, which requires the use of spectacles or contact
lenses for optimal vision. The complications of high myopia can be
vision-threatening; therefore, clinicians and parents have great interest
in controlling myopia progression in children, which may prevent the
complications of myopia that can occur in adulthood. In this review, we
examine recent publications regarding myopia epidemiology and
interventions for controlling myopia progression in children.
Methods
We performed a literature search using PubMed from
the date of inception through 25 June 2018. Studies involving myopia
epidemiology and control of myopia progression were selected; only studies
published in English were reviewed. In the selection of representative
articles for each therapeutic intervention to control myopia progression,
prospective studies were ranked higher than retrospective studies. Among
prospective studies, preference was given to randomised and controlled
trials, as well as studies conducted in Hong Kong or East Asia.
Definition
Myopia is a refractive disorder in which distant
light entering a non-accommodating eye is focused in front of, rather than
on, the retina. Myopia is categorised as axial or refractive myopia. Axial
myopia is more common and results from an elongated eyeball; the onset and
progression of axial myopia occur during childhood and adolescence.
Conversely, refractive myopia is relatively uncommon, and involves the
refractive elements of the eye; examples include index myopia, observed in
patients with the nuclear sclerosis form of cataract, and curvature
myopia, observed in patients with abnormal corneal curvature. Because most
available studies were performed on axial myopia, this review solely
focuses on axial myopia.
Myopia is optically measured in terms of dioptres
(D). In Hong Kong, one dioptre of myopic refractive error (-1.0 D) is
colloquially referred as 100 “degrees” by opticians and the general
public. Another measure closely related to the refractive state of the eye
is the axial length, which is the length of the eyeball from anterior to
posterior poles. An adult emmetropic eye (without refractive error)
typically exhibits an axial length of 22 to 25 mm1;
as a reference value for East Asian populations, the mean axial length in
a large cohort of Chinese adults was 23.3 mm.2
High myopia is commonly defined as myopic
refraction greater than -6.0 D (600 “degrees”) or axial length >26 mm,3 whereas pathologic myopia is
defined as high myopia with the presence of myopic maculopathy, as
determined by an international photographic classification system.4
Regional epidemiology
The current epidemic of myopia is well-known in the
developed countries of East Asia. A high prevalence of myopia has been
reported by many countries with populations of Chinese ancestry.5 There is an increasing incidence of myopia in Hong Kong
children: a local study showed that the rate of myopia in preschool
children increased from 2.3% to 6.3% over 10 years.6 Additionally, there is a high prevalence of myopia in
Hong Kong children: 18.3% at 6 years of age and 61.5% at 12 years of age7; the prevalence of high myopia
(greater than -6.0 D) in the same cohort of Hong Kong children was 0.7% at
6 years of age and 3.8% at 12 years of age.7
There are minimal data regarding the prevalence of
myopia in Hong Kong adults, with the exception of a small study performed
20 years prior to this review, which showed a prevalence of 41.1% in Hong
Kong adults aged ≥40 years.8
Notably, the ongoing population-based epidemiological cohort of the Hong
Kong Children Eye Study will provide updated information regarding myopia
prevalence in schoolchildren 6 to 8 years of age, as well as their
parents. For comparison, the Beijing Eye Study showed a myopia prevalence
of 21.8% in adults aged ≥40 years9;
in Taiwan, a study of male military conscripts, aged 18 to 24 years,
demonstrated an extremely high prevalence of myopia (86.1%) with a mean
refractive error of -3.66 D.10
Regional population genetics
Myopia comprises a multifactorial disease, which is
affected by the interaction of environmental and genetic risk factors.
Differences in myopia prevalence between East Asia and Western nations may
arise as a result of lifestyle discrepancies, as well as differences in
ethnicity and in population genetics. Thus far, a large number of
myopia-linked genetic loci have been identified by genome-wide association
studies and candidate gene-based association studies; detailed information
regarding the prevalences of these loci in different populations has
recently been reviewed.11 Genetic
loci associated with myopia in the Hong Kong Chinese include PAX6,11 12 ZFHX1B,13 VIPR2,14 SNTB1,14
TGIF,15 13q12.12,16 and 5p15.17
The roles of these genes and loci in myopia pathogenesis and clinical
manifestation are not yet known. Further investigations of the
relationships between genotype and phenotype, as well as functional
characterisations of these genes and loci, are warranted.
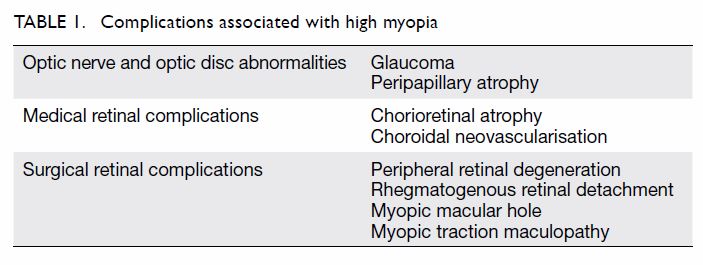
Complications of myopia
Myopia is associated with a wide range of
complications, many of which are vision-threatening and may cause
blindness. A large, population-based study in Beijing revealed that
degenerative myopia was the most common cause of visual impairment and
blindness in adults aged 40 to 49 years; it was the second most common
cause (after cataract) in adults aged ≥50 years.18
The specific pathogenic mechanisms of myopia-related complications have
not yet been elucidated. Mechanical stretching may play a major role,
because progressive elongation of the globe in high myopia places strain
on the sclera, peripapillary region, choroid, and retina.19 Thinning of these structures can cause many of the
degenerative complications observed in high myopia; these complications
are summarised in Table 1.
Pharmacological agents to control myopia progression
Atropine eye drops
Atropine eye drops have been widely used by
ophthalmologists for pupil dilation and cycloplegic refraction. Atropine
is a non-specific muscarinic acetylcholine receptor antagonist, available
as a 1% topical solution; the earliest reports of its clinical effect on
myopia progression were published in the 1970s—monocular application of
atropine in children caused a significant reduction of myopia progression,
compared with the fellow eye.20 21 The mechanism of atropine is not
entirely known. Through experimental animal models, two theories have been
hypothesised to explain the effect of atropine.22
The first theory is that atropine interacts with M1/M4 receptors in the
retina and inhibits eyeball elongation via a neurochemical cascade; the
second theory is that atropine directly inhibits glycosaminoglycan
synthesis by scleral fibroblasts.
The Atropine for the Treatment of Myopia study
(ATOM1) was a double-masked, randomised placebo-controlled trial of
atropine eye drops, which involved 400 Singaporean children with myopia.23 Application of 1% atropine eye
drops in one eye each night significantly reduced myopia progression and
axial elongation over the 2-year study period, compared with control
(-0.28 D vs -1.2 D and -0.02 mm vs +0.38 mm, respectively). No theoretical
anticholinergic systemic adverse effects of dry mouth, skin flushing,
constipation, or urinary difficulty were reported. However, adverse
effects were reported, such that some children were withdrawn from the
study; these included allergic reaction, glare due to pupil dilation, and
blurred near vision due to cycloplegia. Of note, children in the ATOM1
study wore photochromatic spectacles, because the pupil dilation effect of
1% atropine can cause photophobia. A follow-up study of ATOM1 participants
revealed that the effect of atropine on cycloplegia was fully reversible
after cessation of eye drops.24
A subsequent trial, the ATOM2 study, evaluated
lower concentrations of atropine: 0.5%, 0.1%, and 0.01%.25 Dose-related control of myopia was shown with
administration of atropine, but the differences were clinically small.
Two-year measurements of myopia progression were -0.30 D, -0.38 D and
-0.49 D in the 0.5%, 0.1% and 0.01% atropine groups, respectively (P=0.02
between 0.5% and 0.01% groups; P>0.05 between other concentrations).
However, 0.01% atropine showed a negligible effect with respect to
accommodation and pupil size; its effect on near visual acuity was nearly
absent. Therefore, the investigators concluded that 0.01% atropine had
minimal adverse effects, compared with 0.1% and 0.5% atropine, and that it
retained a comparable effect on myopia progression. Importantly, the ATOM2
study was limited by the lack of a placebo group; thus, the role of
low-concentration atropine in myopia control is uncertain.
Recently, the Low-concentration Atropine for Myopia
Progression study was conducted in Hong Kong.26
This was the first-ever placebo-controlled trial of low-concentration
atropine eye drops to confirm their efficacy in myopia control. A total of
438 Chinese children, 4 to 12 years of age, were randomly assigned in a
1:1:1:1 ratio to receive 0.05%, 0.025% or 0.01% atropine, or placebo eye
drops, respectively, once nightly to both eyes, for 1 year. After 1 year,
the mean measurements of myopia progression were -0.27 D, -0.46 D, -0.59 D
and -0.81 D in the atropine 0.05%, 0.025%, 0.01% and placebo groups,
respectively (P<0.001); the respective mean increases in axial length
were 0.20 mm, 0.29 mm, 0.36 mm, and 0.41 mm (P<0.001). There were no
effects on distant or near visual acuity, or on vision-related quality of
life, in any of the groups. The authors concluded that 0.05%, 0.025%, and
0.01% atropine eye drops could reduce myopia progression in a
dose-dependent manner. Of the three concentrations used, 0.05% atropine
was most effective for controlling myopia progression and axial elongation
during the study period.
Following demonstration of the efficacy of various
concentrations of atropine by ATOM1 and ATOM2, it was important to
determine whether the treatment effect remained after cessation of
therapy. A follow-up study of ATOM1 participants demonstrated that 1 year
after cessation of 1% atropine drops, myopia progression in the
atropine-treated group was -1.14 D, compared with -0.38 D in the
placebo-treated group24; thus,
there was a clear rebound phenomenon. A similar rebound phenomenon with
respect to myopia progression was also observed among ATOM2 subjects;
notably, this effect was dose-related—greater rebound was observed in
groups that had used higher concentrations of atropine.27
To investigate prevention of the onset of myopia, a
retrospective study in Taiwan compared pre-myopic children who received
0.025% atropine over a 1-year period with those who did not. Myopic shift
was significantly lower in the atropine-treated group (-0.14 D vs -0.58
D).28
The ATOM1 and ATOM2 studies led to increased
interest in the use of atropine among Hong Kong ophthalmologists. However,
the sole concentration of atropine eye drops commercially available in
Hong Kong public hospitals is 1%; the usage of this dose has been
associated with significant adverse effects, as noted above. At this
stage, the use of atropine eye drops as a measure to mitigate myopia
progression is not yet readily available in the public sector, as none of
the drugs are registered with the Department of Health.
Lower-concentration eye drops either must be ordered on an individual
patient basis, or prepared in collaboration with pharmacies and used in an
off-label manner.
Pirenzepine eye gel
Pirenzepine is a selective muscarinic M1
acetylcholine receptor antagonist. A randomised placebo-controlled
multicentre study, including 353 myopic children from Hong Kong,
Singapore, and Thailand, showed myopia progression of -0.47 D, -0.70 D and
-0.84 D in the 2% gel twice daily, 2% gel once daily and placebo twice
daily groups, respectively.29 The
difference between the pirenzepine 2% gel twice daily and placebo twice
daily groups reached statistical significance (P<0.001). However,
pirenzepine is not commercially available.
Optical means to control myopia progression
Myopia undercorrection
Early animal models30
showed that convex lens–induced myopic defocus could inhibit axial
elongation of the globe; thus, researchers attempted to control myopia
progression in humans via undercorrection with spectacles. Prospective
randomised clinical trials showed that undercorrection of myopia, such as
by under-prescription of spectacles by 0.5 D to 0.75 D, either did not
significantly affect myopia control31
or worsened myopia progression32
compared with full spectacle prescription; this lack of effect was
supported by data from a recent non-interventional large-scale prospective
Chinese cohort.33
Contact lenses
In the 1990s, contact lens usage received
substantial interest as a method to control myopia progression. At the
time, it was speculated that by flattening the cornea, the contact lens
might slow axial elongation. However, randomised controlled trials (RCTs)
showed that both soft contact lenses34
and rigid gas permeable (RGP) lenses35
were ineffective in slowing myopia progression, compared with spectacles
as control.
A randomised study comparing RGP lenses and soft
contact lenses found significant reduction in myopia progression over 3
years in the RGP lens group (-1.56 D vs -2.19 D).36
However, axial elongation did not significantly differ between the two
groups, suggesting that the apparent slowing of myopia progression might
be a result of corneal flattening by RGP lenses, which is reversible upon
discontinuation of RGP lens usage.
Bifocal or progressive addition spectacles
Bifocal or progressive addition spectacles contain
multifocal lenses of two or more distinct optical powers. They are more
commonly used in people aged ≥40 years with presbyopia, because differing
optical powers allow clear vision at various distances. The use of these
spectacles has also been evaluated for control of myopia in children.
Notably, bifocal or progressive addition spectacles are speculated to
reduce accommodative effort during near work, which may reduce peripheral
retinal hyperopic defocus and slow myopia progression.
A meta-analysis from the Cochrane Library37 evaluated eight studies, including one from Hong
Kong,38 which investigated the
effect of bifocal or progressive addition spectacles in slowing myopia
progression. Pooled data suggested that average myopia progression at 1
year was 0.16 D slower for wearers of multifocal spectacles than for
wearers of single vision spectacles. Although the effect was statistically
significant, it was regarded as insufficient for clinical use. A targeted
trial was then designed to evaluate the effect of progressive addition
lenses in children with a high lag of accommodation, a condition suspected
to respond best to multifocal lenses39;
the results showed a similar statistically significant, but clinically
modest, 0.18 D reduction in myopia progression at 1 year in the
progressive addition lens group, compared with the single vision lens
group.
Despite its clinically modest effect, the use of
multifocal lenses is a popular myopia control modality advocated by some
Hong Kong optometrists, because it is readily available and safe.
Orthokeratology
Orthokeratology, known in Hong Kong as
orthokeratology lens, consists of reverse geometry contact lenses which
are worn by children overnight and removed upon waking. This method
provides the convenience of spectacle-free vision during daytime, as it
flattens the cornea during nighttime wear. An RCT conducted in Hong Kong,
the Retardation of Myopia in Orthokeratology study,40 showed a significant effect of orthokeratology in
controlling axial elongation at 2 years, compared with control (single
vision glasses), in children with low-to-moderate myopia (+0.36 mm vs
+0.63 mm). Another RCT in Hong Kong showed a significant effect of
orthokeratology in children with high myopia, compared with control, in
limiting axial elongation at 2 years (+0.19 mm vs +0.51 mm).41
Although orthokeratology has shown promising
results in controlling axial elongation, the long-term effects of this
method remain unknown. In particular, whether discontinuation may result
in rebound of myopia is unclear. The application of contact lenses in
children may be difficult; this difficulty is greater among younger
children. In addition, during the nocturnal usage of any contact lens,
there is an inherent increased risk of corneal infection. Moreover, the
natural rebound to its original corneal contour during the daytime
complicates the use of orthokeratology in high myopes, as there is a
myopic shift towards the end of the day, which leads to deteriorating
vision over time. The vision-threatening complication of infectious
keratitis remains an important concern, as there have been reports of
corneal ulcers in Hong Kong children using orthokeratology lenses.42 More than 160 cases of orthokeratology-associated
infectious keratitis have been reported in the literature; Pseudomonas
aeruginosa and Acanthamoeba are the most common aetiological
agents.43 In addition, children
with atopy are likely to be intolerant of contact lenses.
Orthokeratology is unavailable in public hospitals
in Hong Kong, but is a common practice by many optometrists and some
private ophthalmologists in Hong Kong. The potential benefits of
orthokeratology in slowing myopia progression must be weighed against the
risks of vision-threatening infectious keratitis.
Peripheral retinal defocus
Research in animal models has shown that the
refractive state of the peripheral retina can affect eye growth.44 45
Peripheral retinal myopic defocus, achieved by imposing a convex
refractive element, can inhibit axial elongation in growing animals.
An RCT was performed involving 221 myopic children
in Hong Kong to evaluate the effect of defocus incorporated soft contact
(DISC) lenses, compared with single vision contact lenses as control.46 The DISC lenses achieve peripheral retinal defocus by
incorporating concentric rings that provide an addition of +2.5 D, in a
manner that alternates with normal distance correction. Over a 1-year
period, significant reductions in myopia progression and axial elongation
were noted in the DISC group (-0.30 D vs -0.40 D and +0.13 mm vs +0.18 mm,
respectively). Importantly, achievement of myopia progression slowing of
46% required wearing the DISC lenses for a minimum of 5 hours per day.
However, there was a high dropout rate of 42% in the study, likely because
of the practical difficulties associated with contact lens use in
children. The potential risk of infectious keratitis was also a major
concern for clinicians involved in the study.
Because of the inconvenience and risk of contact
lens use in children, defocus incorporated multiple segments (DIMS)
spectacle lenses have been developed by a local university in Hong Kong.
The lenses comprise a central optical zone used to correct myopia,
combined with multiple segments of myopic defocus around the central zone,
which extend to the mid-periphery of the lens. Preliminary results suggest
a significant effect of DIMS in slowing myopia progression and axial
elongation, compared with control.47
Thus far, DIMS spectacles are not yet commercially available in Hong Kong.
Lifestyle modification for control of myopia
progression
Outdoor activity
Epidemiological studies have demonstrated a
difference in the prevalence of myopia in urban and rural areas; thus,
outdoor activity has been hypothesised to affect myopia onset and
progression, because much less time is spent outdoors in many urban areas.
A meta-analysis of seven cross-sectional studies reported a 2% reduction
in the odds of myopia per additional hour of time spent outdoors per week.48
Prospective studies have been conducted to examine
the effect of outdoor activity as an intervention. A recent randomised
study in Taiwan included 16 schools: intervention schools implemented a
programme to remove children from the classroom during recess and
encourage them to participate in outdoor activities.49 Myopia progression and axial elongation were
significantly reduced in the intervention group, compared with control
(-0.35 D vs -0.47 D and +0.28 mm vs +0.33 mm, respectively). A similar
study in Taiwan, which compared two neighbouring schools, found a
significantly lower rate of myopia onset in the intervention group (8.41%
vs 17.65%).50 A similar
significant effect on incident myopia was revealed in a prospective study
in Guangzhou, China: intervention schools had a 40-minute outdoor activity
class added to each school day.51
Three-year cumulative incident myopia was significantly lower in the
intervention group (30.4% vs 39.5%); however, there were no significant
differences in axial elongation between the intervention and control
groups (+0.95 mm vs +0.98 mm; P=0.07). Thus, outdoor activity may slow
myopia onset, but its effect on myopia progression is not yet clear.
The aetiology of this protective effect against
myopia onset is uncertain. Animal models suggest that light exposure can
stimulate retinal dopaminergic pathways, which then interfere with eye
growth signalling pathways, preventing excessive elongation of the
eyeball.52 Given the academic
pressures and generally urban lifestyle among Hong Kong children, this
intervention may be effective, but is likely to be difficult to implement
in the greater context of public health.
Near work
Near work is regarded by the general public as a
risk factor for myopia development and myopia progression. However,
evidence is conflicting, and the quantification of near work is often
difficult. A meta-analysis of 27 studies (including 14 from Asia) found
higher odds of myopia (odds ratio=1.14) associated with longer periods of
time devoted to near work.53
However, reports from Beijing54
and Singapore55 showed no
significant effect of near work on myopia.
Thus far, there have been no prospective controlled
trials regarding near work reduction as an intervention to control myopia
progression.
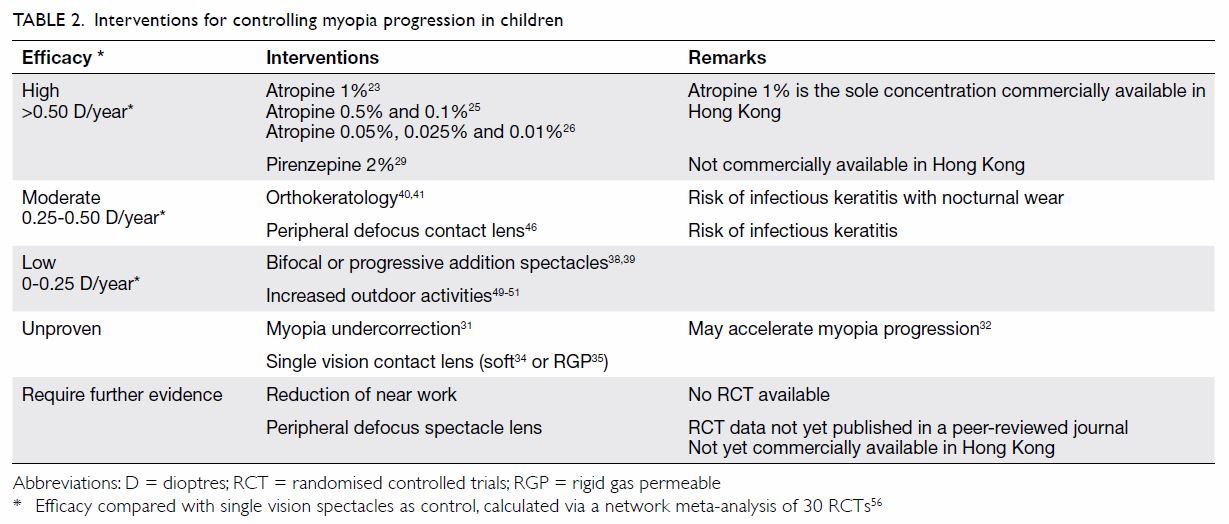
Summary of interventions to control myopia progression
Cross-comparisons between interventions for
controlling myopia progression are difficult, owing to intrinsic
differences in study design and baseline patient characteristics. A recent
network meta-analysis included 30 RCTs in attempt to cross-compare the
efficacies of interventions for slowing myopia progression in children.56 The most effective interventions
were atropine and pirenzepine, followed by orthokeratology and peripheral
defocus contact lenses. Multifocal spectacles and increased periods of
outdoor activity were also found to be useful, but these effects were
modest. Notably, combinations of these modalities have not been assessed
to determine whether they might have additional effects. Interventions for
controlling myopia progression discussed in this review are summarised in
Table 2.23 25 26
29 31
32 34
35 38
39 40
41 46
49 50
51 56
Conclusion
There is an epidemic of myopia in East Asia, and
local data suggest a high prevalence of myopia in Hong Kong children.
Genetic studies have revealed a few loci associated with myopia in Hong
Kong Chinese; however, the exact mechanisms of these loci are not yet
known. Clinical trials have provided strong evidence regarding the
efficacy of several interventions to control myopia progression in
children. However, there are practical concerns, because some
interventions (eg, concentrations of atropine <1%, as well as
pirenzepine) are not currently available in Hong Kong. Moreover, some
interventions (eg, orthokeratology and peripheral defocus contact lens)
have potential visionthreatening adverse effects.
Author contributions
Concept and design: CY Mak, AL Young.
Acquisition of data: CY Mak, JCS Yam, LJ Chen.
Analysis and interpretation of data: CY Mak, JCS Yam, LJ Chen.
Drafting of the article: All authors.
Critical revision for important intellectual content: All authors.
Acquisition of data: CY Mak, JCS Yam, LJ Chen.
Analysis and interpretation of data: CY Mak, JCS Yam, LJ Chen.
Drafting of the article: All authors.
Critical revision for important intellectual content: All authors.
Declaration
All authors have disclosed no conflicts of
interest. All authors had full access to the data, contributed to the
study, approved the final version for publication, and take responsibility
for its accuracy and integrity.
References
1. Bhardwaj V, Rajeshbhai GP. Axial length,
anterior chamber depth-a study in different age groups and refractive
errors. J Clin Diagn Res 2013;7:2211-2. Crossref
2. Yin G, Wang YX, Zheng ZY, et al. Ocular
axial length and its associations in Chinese: the Beijing Eye Study. PLoS
One 2012;7:e43172. Crossref
3. Ohno-Matsui K. Pathologic myopia. Asia
Pac J Ophthalmol (Phila) 2016;5:415-23. Crossref
4. Ohno-Matsui K, Kawasaki R, Jonas JB, et
al. International photographic classification and grading system for
myopic maculopathy. Am J Ophthalmol 2015;159:877-83.e7. Crossref
5. Wu PC, Huang HM, Yu HJ, Fang PC, Chen
CT. Epidemiology of myopia. Asia Pac J Ophthalmol (Phila) 2016;5:386-93. Crossref
6. Fan DS, Lai C, Lau HH, Cheung EY, Lam
DS. Change in vision disorders among Hong Kong preschoolers in 10 years.
Clin Exp Ophthalmol 2011;39:398-403. Crossref
7. Lam CS, Lam CH, Cheng SC, Chan LY.
Prevalence of myopia among Hong Kong Chinese schoolchildren: changes over
two decades. Ophthalmic Physiol Opt 2012;32:17-24. Crossref
8. van Newkirk MR. The Hong Kong vision
study: a pilot assessment of visual impairment in adults. Trans Am
Ophthalmol Soc 1997;95:715-49.
9. Xu L, Li J, Cui T, et al. Refractive
error in urban and rural adult Chinese in Beijing. Ophthalmology
2005;112:1676-83. Crossref
10. Lee YY, Lo CT, Sheu SJ, Lin JL. What
factors are associated with myopia in young adults? A survey study in
Taiwan military conscripts. Invest Ophthalmol Vis Sci 2013;54:1026-33. Crossref
11. Tang SM, Rong SS, Young AL, Tam PO,
Pang CP, Chen LJ. PAX6 gene associated with high myopia: a meta-analysis.
Optom Vis Sci 2014;91:419-29. Crossref
12. Tang SM, Ma L, Lu SY, et al.
Association of the PAX6 gene with extreme myopia rather than lower grade
myopias. Br J Ophthalmol 2018;102:570-4. Crossref
13. Khor CC, Miyake M, Chen LJ, et al.
Genome-wide association study identifies ZFHX1B as a susceptibility locus
for severe myopia. Hum Mol Genet 2013;22:5288-94. Crossref
14. Shi Y, Gong B, Chen L, et al. A
genome-wide meta-analysis identifies two novel loci associated with high
myopia in the Han Chinese population. Hum Mol Genet 2013;22:2325-33. Crossref
15. Lam DS, Lee WS, Leung YF, et al.
TGFbeta-induced factor: a candidate gene for high myopia. Invest
Ophthalmol Vis Sci 2003;44:1012-5. Crossref
16. Shi Y, Qu J, Zhang D, et al. Genetic
variants at 13q12.12 are associated with high myopia in the Han
Chinese population. Am J Hum Genet 2011;88:805-13. Crossref
17. Lam CY, Tam PO, Fan DS, et al. A
genome-wide scan maps a novel high myopia locus to 5p15. Invest Ophthalmol
Vis Sci 2008;49:3768-78. Crossref
18. Xu L, Wang Y, Li Y, et al. Causes of
blindness and visual impairment in urban and rural areas in Beijing: the
Beijing Eye Study. Ophthalmology 2006;113:1134.e1-11. Crossref
19. Ohno-Matsui K, Lai TY, Lai CC, Cheung
CM. Updates of pathologic myopia. Prog Retin Eye Res 2016;52:156-87. Crossref
20. Bedrossian RH. The effect of atropine
on myopia. Ann Ophthalmol 1971;3:891-7.
21. Bedrossian RH. The effect of atropine
on myopia. Ophthalmology 1979;86:713-9. Crossref
22. Tan D, Tay SA, Loh KL, Chia A. Topical
atropine in the control of myopia. Asia Pac J Ophthalmol (Phila)
2016;5:424-8. Crossref
23. Chua WH, Balakrishnan V, Chan YH, et
al. Atropine for the treatment of childhood myopia. Ophthalmology
2006;113:2285-91. Crossref
24. Tong L, Huang XL, Koh AL, Zhang X, Tan
DT, Chua WH. Atropine for the treatment of childhood myopia: effect on
myopia progression after cessation of atropine. Ophthalmology
2009;116:572-9. Crossref
25. Chia A, Chua WH, Cheung YB, et al.
Atropine for the treatment of childhood myopia: safety and efficacy of
0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2).
Ophthalmology 2012;119:347-54. Crossref
26. Yam JC, Jiang Y, Tang SM, et al.
Low-concentration Atropine for Myopia Progression (LAMP) study: a
randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025% and
0.01% atropine eye drops in myopia control. Ophthalmology. Available from:
https://www.aaojournal.org/article/S0161-6420(18)30285-9/abstract. In
press.
27. Chia A, Chua WH, Wen L, Fong A, Goon
YY, Tan D. Atropine for the treatment of childhood myopia: changes after
stopping atropine 0.01%, 0.1% and 0.5%. Am J Ophthalmol 2014;157:451-7.e1.
Crossref
28. Fang PC, Chung MY, Yu HJ, Wu PC.
Prevention of myopia onset with 0.025% atropine in premyopic children. J
Ocul Pharmacol Ther 2010;26:341-5. Crossref
29. Tan DT, Lam DS, Chua WH, Shu-Ping DF,
Crockett RS; Asian Pirenzepine Study Group. One-year multicenter,
double-masked, placebo-controlled, parallel safety and efficacy study of
2% pirenzepine ophthalmic gel in children with myopia. Ophthalmology
2005;112:84-91. Crossref
30. Schaeffel F, Glasser A, Howland HC.
Accommodation, refractive error and eye growth in chickens. Vision Res
1988;28:639-57. Crossref
31. Adler D, Millodot M. The possible
effect of undercorrection on myopic progression in children. Clin Exp
Optom 2006;89:315-21. Crossref
32. Chung K, Mohidin N, O’Leary DJ.
Undercorrection of myopia enhances rather than inhibits myopia
progression. Vision Res 2002;42:2555-9. Crossref
33. Sun YY, Li SM, Li SY, et al. Effect of
uncorrection versus full correction on myopia progression in 12-year-old
children. Graefes Arch Clin Exp Ophthalmol 2017;255:189-95. Crossref
34. Horner DG, Soni PS, Salmon TO, Swartz
TS. Myopia progression in adolescent wearers of soft contact lenses and
spectacles. Optom Vis Sci 1999;76:474-9. Crossref
35. Katz J, Schein OD, Levy B, et al. A
randomized trial of rigid gas permeable contact lenses to reduce
progression of children’s myopia. Am J Ophthalmol 2003;136:82-90. Crossref
36. Walline JJ, Jones LA, Mutti DO, Zadnik
K. A randomized trial of the effects of rigid contact lenses on myopia
progression. Arch Ophthalmol 2004;122:1760-6. Crossref
37. Walline JJ, Lindsley K, Vedula SS,
Cotter SA, Mutti DO, Twelker JD. Interventions to slow progression of
myopia in children. Cochrane Database Syst Rev 2011;(12):CD004916. Crossref
38. Edwards MH, Li RW, Lam CS, Lew JK, Yu
BS. The Hong Kong progressive lens myopia control study: study design and
main findings. Invest Ophthalmol Vis Sci 2002;43:2852-8.
39. Berntsen DA, Sinnott LT, Mutti DO,
Zadnik K. A randomized trial using progressive addition lenses to evaluate
theories of myopia progression in children with a high lag of
accommodation. Invest Ophthalmol Vis Sci 2012;53:640-9. Crossref
40. Cho P, Cheung SW. Retardation of
myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical
trial. Invest Ophthalmol Vis Sci 2012;53:7077-85. Crossref
41. Charm J, Cho P. High myopia-partial
reduction ortho-k: a 2-year randomized study. Optom Vis Sci 2013;90:530-9.
Crossref
42. Young AL, Leung AT, Cheng LL, Law RW,
Wong AK, Lam DS. Orthokeratology lens-related corneal ulcers in children:
a case series. Ophthalmology 2004;111:590-5. Crossref
43. Kam KW, Yung W, Li GK, Chen LJ, Young
AL. Infectious keratitis and orthokeratology lens use: a systematic
review. Infection 2017;45:727-35. Crossref
44. Benavente-Pérez A, Nour A, Troilo D.
Axial eye growth and refractive error development can be modified by
exposing the peripheral retina to relative myopic or hyperopic defocus.
Invest Ophthalmol Vis Sci 2014;55:6765-73. Crossref
45. Liu Y, Wildsoet C. The effective add
inherent in 2-zone negative lenses inhibits eye growth in myopic young
chicks. Invest Ophthalmol Vis Sci 2012;53:5085-93. Crossref
46. Lam CS, Tang WC, Tse DY, Tang YY, To
CH. Defocus incorporated soft contact (DISC) lens slows myopia progression
in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trial.
Br J Ophthalmol 2014;98:40-5. Crossref
47. The Hong Kong Polytechnic University.
Spectacle lens designed by PolyU slows myopic progression by 60% and stops
in 21.5% of children. Appendix I. Available from:
https://www.polyu.edu.hk/web/filemanager/en/content_155/7027/Appendix.pdf.
Accessed 20 May 2018.
48. Sherwin JC, Reacher MH, Keogh RH,
Khawaja AP, Mackey DA, Foster PJ. The association between time spent
outdoors and myopia in children and adolescents: a systematic review and
meta-analysis. Ophthalmology 2012;119:2141-51. Crossref
49. Wu PC, Chen CT, Lin KK, et al. Myopia
prevention and outdoor light intensity in a school-based cluster
randomized trial. Ophthalmology 2018;125:1239-50. Crossref
50. Wu PC, Tsai CL, Wu HL, Yang YH, Kuo
HK. Outdoor activity during class recess reduces myopia onset and
progression in school children. Ophthalmology 2013;120:1080-5. Crossref
51. He M, Xiang F, Zeng Y, et al. Effect
of time spent outdoors at school on the development of myopia among
children in China: a randomized clinical trial. JAMA 2015;314:1142-8. Crossref
52. Feldkaemper M, Schaeffel F. An updated
view on the role of dopamine in myopia. Exp Eye Res 2013;114:106-19. Crossref
53. Huang HM, Chang DS, Wu PC. The
association between near work activities and myopia in children—a
systematic review and meta-analysis. PLoS One 2015;10:e0140419. Crossref
54. Lin Z, Vasudevan B, Jhanji V, et al.
Near work, outdoor activity, and their association with refractive error.
Optom Vis Sci 2014;91:376-82. Crossref
55. Saw SM, Shankar A, Tan SB, et al. A
cohort study of incident myopia in Singaporean children. Invest Ophthalmol
Vis Sci 2006;47:1839-44. Crossref
56. Huang J, Wen D, Wang Q, et al.
Efficacy comparison of 16 interventions for myopia control in children: a
network meta-analysis. Ophthalmology 2016;123:697-708. Crossref