Hong
Kong Med J 2018 Dec;24(6):579–83 | Epub 19 Nov 2018
DOI: 10.12809/hkmj187227
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Post-fracture care gap: a retrospective
population-based analysis of Hong Kong from 2009 to 2012
MY Cheung, MB, ChB; Angela WH Ho, MB, ChB, FHKAM
(Orthopaedic Surgery); SH Wong, MB, BS, FHKAM (Orthopaedic Surgery)
Department of Orthopaedics and Traumatology,
Caritas Medical Centre, Sham Shui Po, Hong Kong
Corresponding author: Dr Angela WH Ho (angelaho@alumni.cuhk.net)
Abstract
Introduction: Patients who
sustain an osteoporotic fracture are at increased risk of sustaining
further osteoporotic fracture. The risk can be reduced by prescription
of anti-osteoporosis medication. The aim of the present study was to
determine the current practice in Hong Kong regarding secondary drug
prevention of fragility fractures after osteoporotic hip fracture.
Methods: Dispensation of
anti-osteoporosis medication records from patients with new fragility
hip fractures aged ≥65 years were retrieved using the Hospital Authority
Clinical Data Analysis and Reporting System from 2009 to 2012. The
intervention rate each year was determined from the percentage of
patients receiving anti-osteoporosis medication within 1 year after hip
fracture.
Results: A total of 15 866
patients with osteoporotic hip fracture who met the criteria were
included. The intervention rate differed each year from 2009 to 2012,
ranging between 9% and 15%. Orthopaedic surgeons initiated 63% of
anti-osteoporosis medication, whereas physicians initiated 37%. The
anti-osteoporosis drugs being prescribed included alendronic acid (76%),
ibandronic acid (12%), strontium ranelate (5%), and zoledronic acid
(4%).
Conclusion: Most patients with
hip fracture remained untreated for 1 year after the osteoporotic hip
fracture. The Hospital Authority should allocate more resources to
implement a best practice framework for treatment of patients with hip
fracture at high risk of secondary fracture.
New knowledge added by this study
- Few patients receive anti-osteoporosis medication after hip fracture.
- Implementation of secondary drug prevention of osteoporotic fractures differs among hospitals and specialties.
- The Hong Kong government should allocate more resources for secondary drug prevention of osteoporotic fractures.
- By reducing subsequent fractures, the government can realise substantial cost-savings.
Introduction
There are increasing numbers of geriatric hip
fractures among the ageing population in Hong Kong.1 Patients who sustain an osteoporotic fracture are at
increased risk of sustaining further osteoporotic fractures.2 3 The
cumulative incidence of second hip fracture was 5.1% at 2 years and 8.6%
at 8 years.4 This situation can be
improved by implementing better guidelines for secondary drug prevention
of fragility fractures. Appropriate treatment of patients with fragility
fractures has been shown to reduce subsequent risk of fragility fracture
by up to 50%.5 6 7
Many countries in the world have well-established
guidelines to close this post-fracture care gap. However, this problem has
been overlooked in Hong Kong and the situation is not improving. Diagnosis
and treatment of osteoporosis differs among hospitals and specialties.
There are no standardised guidelines for treating this particular group of
elderly patients. The aim of the present study was to determine the
current practice in Hong Kong regarding secondary drug prevention of
fragility fractures after osteoporotic hip fracture, in order to make
recommendations to implement better guidelines.
Methods
In Hong Kong, about 98% of all hospital admissions
for hip fracture were admitted to public hospitals rather than private
hospitals.8 Patient records from
2009 to 2012, including data on the dispensation of anti-osteoporosis
medication to patients aged ≥65 years with new fragility hip fractures,
were retrieved from the Hospital Authority Clinical Data Analysis and
Reporting System. Patients with hip fracture were identified using
International Classification of Diseases, Ninth Revision, Clinical
Modification (ICD-9-CM) codes 81.52, 81.51, 81.40, 79.15, 79.35, or 78.55
under subdivision Operation Theatre Management System–linked diagnosis.
Patients who took anti-osteoporosis medication before the fracture and
those with pathological fractures were excluded. For the remaining
patients who were eligible for secondary drug prevention, we determined
the intervention rate each year by determining the percentage of patients
receiving anti-osteoporosis medication within 1 year after hip fracture.
Version 4 of the strengthening the reporting of observational studies in
epidemiology (STROBE) guidelines for cross-sectional studies was used in
the preparation of this manuscript.
Results
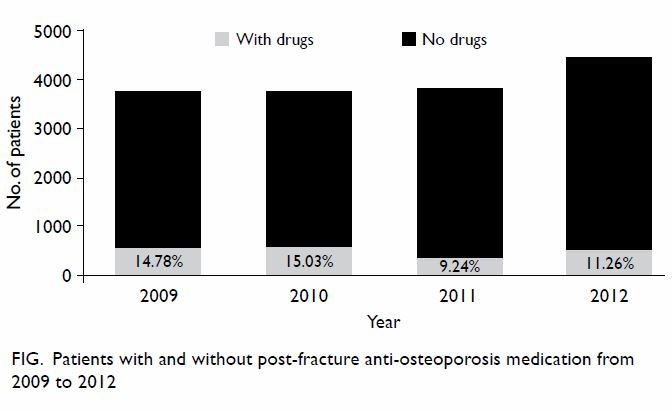
A total of 15 866 patients with osteoporotic hip
fracture who met the criteria were included. From records on
anti-osteoporosis medicine initiation, the intervention rate between 2009
and 2012 was found to be different each year, from as low as 9% in 2010
and as high as 15% in 2009 (Fig). The prescription rate for anti-osteoporosis
medication was 14.78% in 2009, 25.03% in 2010, 9.24% in 2011, and 11.26%
in 2012. Among the specialties prescribing anti-osteoporosis medication,
orthopaedic surgeons initiated 63% of the prescriptions, whereas
physicians initiated 37%. The anti-osteoporosis drugs prescribed in
descending order were alendronic acid (76%), ibandronic acid (12%),
strontium ranelate (5%), zoledronic acid (4%), risedronic acid (1%),
teriparatide (1%), and denosumab (1%). The rate of anti-osteoporosis
medication prescription was between 7% and 31% among the seven public
acute hospitals with orthopaedic emergency admission included in the
study.
Discussion
A 2015 study of geriatric hip fractures showed that
there had been a steady increase in the incidence of geriatric hip
fracture in Hong Kong.1 The
worldwide incidence of geriatric hip fractures is also projected to
increase.9 We expect to see more
patients with fragility fractures in our daily practice with the growing
ageing population.
Patients with geriatric hip fracture carry a high
mortality rate; the overall 30-day mortality is 3.01% and 1-year mortality
is 18.56%.1 Older age and male sex are associated with an increase in
mortality and a higher excess mortality rate following surgery.1 Patients with a second episode of hip fracture have
been found to have an even higher mortality rate.4
By initiating anti-osteoporosis medication, those subsequent fragility
fractures could be prevented.
The British Orthopaedic Association sets standards
for surgeons to comply with in order to improve the quality and outcomes
of care and also to reduce costs.2
Bone health management includes calcium and vitamin D supplement,
osteoporosis treatment, and bone densitometry measurement. According to
the American Society for Bone and Mineral Research Task Force 2012,
patients with hip fracture should receive pharmacological treatment to
prevent additional fractures, because they are clearly at risk for
recurrent hip or other osteoporotic fractures, and initiation of
bisphosphonate therapy after hip fracture has been shown to reduce the
risk of a second hip fracture.10
The main limitation of the present study was that
the data were mainly retrieved from a database of patient records. The
accuracy of these records depends on the correct entry by clinicians of
the diagnosis of hip fracture. Another limitation is that the government
drug dispensation record does not included data from patients who choose
to receive anti-osteoporosis medication in the private sector. This may
create an underestimation of the treatment rate.
Although the treatment rate may have been
underestimated in the present study, worldwide rates of osteoporosis
treatment after hip fracture have been reported to be as low as 10% to 20%
within 1 year.11 12 13 14 15 16 17 18 19 20 A recent study in Hong Kong showed that 33% of
patients with hip fracture were prescribed medication for osteoporosis in
the 6 months after discharge from the hospital.21
There are also wide discrepancies in drug prescription rates among
different hospitals.
There are several potential reasons for these
differences in drug prescription rates among hospitals. Firstly, different
hospitals follow different working guidelines for the treatment of
osteoporosis after hip fracture. Without standardisation of the
guidelines, there can be a lack of clarity regarding the responsibility to
undertake this care. Siris et al14
found that some physicians did not realise the significance of the
initiation of anti-osteoporosis medication after fragility fractures,
causing underdiagnosis and undertreatment of osteoporosis. Secondly, some
clinicians refer patients to physicians for initiating osteoporosis
treatment; especially in centres without geriatric support, these
follow-up appointments with physicians can be up to 1 year after discharge
from the hospital. Thirdly, many geriatric patients may have renal failure
and may be contra-indicated for certain first-line anti-osteoporosis
medication such as bisphosphonates. They may be unable to afford other
more expensive self-financed anti-osteoporosis medication. Other factors
that affect prescription rates include concerns about medication, and the
available time and funds for diagnosis and treatment.13
The prevalence of femoral neck osteoporosis based
on hip T-score of less than -2.5 was 47.8% in men and 59.1% in women in a
Hong Kong study of 239 geriatric hip fractures.21
In the present study, the intervention rate each year was found to be only
9% to 15% across 2009 to 2012. There is obviously still a huge
post-fracture gap in secondary prevention. Many patients with fragility
fracture do not receive osteoporosis treatment for >1 year after hip
fracture. Furthermore, there was little to no improvement in the
prescription rates among the 4 years studied. Huge improvements could be
achieved by raising the awareness of secondary drug prevention of
osteoporosis and increasing the motivation of physicians.
Improvements can only be achieved with involvement
of both the government and the individual specialties. The government
should allocate more resources and implement a best practice framework for
patients with hip fracture at high risk of secondary fracture. The
government should also subsidise more anti-osteoporosis medications, so
that better treatment can be provided in complicated and severe cases.
Because the treatment of osteoporosis differs among hospitals and
specialties, a fragility fracture committee or a fracture liaison service
can coordinate and standardise patient care by setting up and implementing
an easy-to-follow protocol. More education on the treatment of
osteoporosis should be provided for orthopaedic and medical departments,
to raise awareness and update the relevant knowledge in anti-osteoporosis
medication advancement. In some complicated cases of osteoporosis, the
involvement of different specialties is essential. The formation of
geriatric-orthopaedic working groups and their early involvement in the
perioperative and postoperative period can help ensure that optimal care
is provided to all patients. Even with anti-osteoporosis medication, a
good rehabilitation programme with fall prevention is required; this
should be set up in collaboration with allied health professionals. With
cooperation between the government and different hospital specialties,
more secondary fragility fractures can be prevented. Patients will benefit
from prevention of the morbidity and mortality associated with secondary
fragility fracture.
Recently there has been debate on osteoporosis
treatment and atypical femur fractures. Modi et al22 report that adherence to oral bisphosphonates is low,
estimating that, of patients who are prescribed oral bisphosphonates,
fewer than 40% are still taking them after 1 year. Although atypical femur
fractures have been reported at very low frequencies, not only with
bisphosphonate use but also following treatment with denosumab,23 patients are becoming increasingly reluctant to take
anti-osteoporosis medication. An analysis of three randomised controlled
trials of bisphosphonates concluded that treating 1000 women with
osteoporosis for 3 years with a bisphosphonate will prevent approximately
100 vertebral or non-vertebral fractures (number needed to treat: 10).24 Importantly, for the 100 fractures prevented,
bisphosphonates might cause 0.02 to 1.25 atypical femur fractures,
assuming the relative risk ranges from 1.2 to 11.8 (number needed to harm:
800 to 43 300).25 Hence the
beneficial effect of osteoporosis treatment still outweighs the risk for
atypical femur fracture.
In Hong Kong, about 98% of all hospital admissions
for hip fracture were admitted to public hospitals rather than private
hospitals.8 Public hospitals in
Hong Kong face a huge financial burden and lack of health care resources
for providing optimal care to the ageing population. The cost associated
with the prescription of anti-osteoporosis medication is of concern of the
government. However, the tremendous hospital expenditure related to hip
fracture care can be easily overlooked. In Hong Kong, the direct medical
cost for each hip fracture was US$8831.9 in 2018, with the projected
direct cost of US$84.7 million in total.26
In 2014, 84% of the drugs prescribed for osteoporosis were
bisphosphonates.27 The annual cost
of prescription of bisphosphonates per patient was approximately HK$174.
Although multiple patients must be treated to prevent a single fracture,
reducing the number of subsequent osteoporotic fractures can help the
government to achieve significant cost-savings.
Despite the numerous benefits of anti-osteoporosis
medication for patients with fragility fractures, the prescription rate
remains low not only in Hong Kong, but also in the other parts of the
world. Physicians should be aware of the benefits of anti-osteoporosis
medication for patients with fragility fractures and guidelines for
osteoporosis treatment should be developed and used more widely.
Conclusion
There is a large post-fracture care gap in
secondary drug prevention for patients with osteoporotic hip fracture in
Hong Kong. The majority of the patients are neither diagnosed nor tested
for osteoporosis. Most remained untreated for 1 year after the
osteoporotic hip fracture. The Hong Kong Hospital Authority needs to
allocate more resources to implement a best practice framework for
patients with hip fracture at high risk of secondary fracture, so that
they receive appropriate anti-osteoporosis medication. By reducing the
number of subsequent osteoporotic fractures, the Hospital Authority can
realise substantial cost-savings.
Author contributions
Concept and design: All authors.
Acquisition of data: MY Cheung, AWH Ho.
Analysis or interpretation of data: MY Cheung, AWH Ho.
Drafting of the article: MY Cheung, AWH Ho.
Critical revision for important intellectual content: MY Cheung, AWH Ho.
Acquisition of data: MY Cheung, AWH Ho.
Analysis or interpretation of data: MY Cheung, AWH Ho.
Drafting of the article: MY Cheung, AWH Ho.
Critical revision for important intellectual content: MY Cheung, AWH Ho.
Declaration
All authors have disclosed no conflicts of
interest. All authors had full access to the data, contributed to the
study, approved the final version for publication, and take responsibility
for its accuracy and integrity. An earlier version of this paper was
presented as a poster at the Annual Congress of the Hong Kong Orthopaedic
Association, 6 to 8 November 2015, Hong Kong; at the World Congress on
Osteoporosis, Osteoarthritis and Musculoskeletal Diseases, 26 to 29 March
2015, Milan, Italy; and at the 15th Regional Osteoporosis Conference, 24
to 25 May 2014, Hong Kong.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
References
1. Man LP, Ho AW, Wong SH. Excess mortality
for operated geriatric hip fracture in Hong Kong. Hong Kong Med J
2016;22:6-10. Crossref
2. British Orthopaedic Association. The
Care of Patients with Fragility Fracture. London: British Orthopaedic
Association; 2007.
3. Johnell O, Kanis JA, Odén A, et al.
Fracture risk following an osteoporotic fracture. Osteoporos Int
2004;15:175-9. Crossref
4. Lee YK, Ha YC, Yoon BH, Koo KH.
Incidence of second hip fracture and compliant use of bisphosphonate.
Osteoporos Int 2013;24:2099-104. Crossref
5. Lyles KW, Colón-Emeric CS, Magaziner JS,
et al. Zoledronic acid and clinical fractures and mortality after hip
fracture. N Engl J Med 2007;357:1799-809. Crossref
6. Harris ST, Watts NB, Genant HK, et al.
Effects of risedronate treatment on vertebral and nonvertebral fractures
in women with postmenopausal osteoporosis: a randomized controlled trial.
Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. JAMA
1999;282:1344-52. Crossref
7. Black DM, Cummings SR, Karpf DB, et al.
Randomised trial of effect of alendronate on risk of fracture in women
with existing vertebral fractures. Fracture Intervention Trial Research
Group. Lancet 1996;348:1535-41. Crossref
8. Chau PH, Wong M, Lee A, Ling M, Woo J.
Trends in hip fracture incidence and mortality in Chinese population from
Hong Kong 2001-09. Age Ageing 2013;42:229-33. Crossref
9. Gullberg B, Johnell O, Kanis JA.
World-wide projections for hip fracture. Osteoporos Int 1997;7:407-13. Crossref
10. Eisman JA, Bogoch ER, Dell R, et al.
Making the first fracture the last fracture: ASBMR task force on secondary
fracture prevention. J Bone Miner Res 2012;27:2039-46. Crossref
11. Andrade SE, Majumdar SR, Chan KA et
al. Low frequency of treatment of osteoporosis among postmenopausal women
following a fracture. Arch Intern Med 2003;163:2052-7. Crossref
12. Feldstein A, Elmer PJ, Orwoll E,
Herson M, Hillier T. Bone mineral density measurement and treatment for
osteoporosis in older individuals with fractures: a gap in evidence-based
practice guideline implementation. Arch Intern Med 2003;163:2165-72. Crossref
13. Elliot-Gibson V, Bogoch ER, Jamal SA,
Beaton DE. Practice patterns in the diagnosis and treatment of
osteoporosis after a fragility fracture: a systematic review. Osteoporos
Int 2004;15:767-78. Crossref
14. Siris ES, Bilezikian JP, Rubin MR, et
al. Pins and plaster aren’t enough: a call for the evaluation and
treatment of patients with osteoporotic fractures. J Clin Endocrinol Metab
2003;88:3482-6. Crossref
15. Kamel HK, Hussain MS, Tariq S, Perry
HM, Morley JE. Failure to diagnose and treat osteoporosis in elderly
patients hospitalized with hip fracture. Am J Med 2000;109:326-9. Crossref
16. Torgerson DJ, Dolan P. Prescribing by
general practitioners after an osteoporotic fracture. Ann Rheum Dis
1998;57:378-9. Crossref
17. Follin SL, Black JN, McDermott MT.
Lack of diagnosis and treatment of osteoporosis in men and women after hip
fracture. Pharmacotherapy 2003;23:190-8. Crossref
18. Juby AG, De Geus-Wenceslau CM.
Evaluation of osteoporosis treatment in seniors after hip fracture.
Osteoporos Int 2002;13:205-10. Crossref
19. Harrington JT, Broy SB, Derosa AM,
Licata AA, Shewmon DA. Hip fracture patients are not treated for
osteoporosis: a call to action. Arthritis Rheum 2002;47:651-4. Crossref
20. Gardner MJ, Brophy RH, Demetrakopoulos
D, et al. Interventions to improve osteoporosis treatment following hip
fracture. A prospective randomized trial. J Bone Joint Surg Am
2005;87:3-7. Crossref
21. Ho AW, Lee MM, Chan EW, et al.
Prevalence of pre-sarcopenia and sarcopenia in Hong Kong Chinese geriatric
patients with hip fracture and its correlation with different factors.
Hong Kong Med J 2016;22:23-9. Crossref
22. Modi A, Siris ES, Tang J, Sen S. Cost
and consequences of noncompliance with osteoporosis treatment among women
initiating therapy. Curr Med Res Opin 2015;31:757-65. Crossref
23. Selga J, Nuñez JH, Minguell J, Lalanca
M, Garrido M. Simultaneous bilateral atypical femoral fracture in a
patient receiving denosumab: case report and literature review. Osteoporos
Int 2016;27:827-32. Crossref
24. Black DM, Kelly MP, Genant HK, et al.
Bisphosphonates and fractures of the subtrochanteric or diaphyseal femur.
N Engl J Med 2010;362:1761-71. Crossref
25. Black DM, Rosen CJ. Clinical practice.
Postmenopausal osteoporosis. N Engl J Med 2016;374:254-62. Crossref
26. Cheung CL, Ang SB, Chadha M, et al. An
updated hip fracture projection in Asia: The Asian Federation of
Osteoporosis Societies study. Osteoporos Sarcopenia 2018;4:16-21. Crossref
27. Ho KC, Tsoi MF, Cheung TT, Cheung CL,
Cheung BM. Increase in prescriptions for osteoporosis and reduction in hip
fracture incidence in Hong Kong during 2005-2014. Hong Kong Med J
2016;22(Suppl 1):25S.