DOI: 10.12809/hkmj144439
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Intracoronary thrombus in an 18-year-old teenager. Why?
Mert I Hayiroglu, MD; Adnan Kaya, MD; Sahin Avsar, MD; Nijat Bakishaliev, MD; Emrah Bozbeyoglu, MD
Department of Cardiology, Dr Siyami Ersek Cardiovascular and Thoracic Surgery Hospital, Istanbul, Turkey
Corresponding author: Dr Adnan Kaya (adnankaya@ymail.com)
Case report
In August 2014, an 18-year-old boy with no prior history of coronary or cardiac disease presented
to our tertiary cardiovascular and thoracic surgery
hospital in Turkey with crushing substernal chest
pain, nausea, and vomiting that had persisted for 1
hour. He had started work as a barman at a beach
club 3 months earlier and denied any use of off-label
drugs. His first electrocardiography (ECG) was
normal with sinus rhythm (heart rate, 90 beats/min;
Fig 1a). The patient, however, was tachypnoeic and reported a heavy squeezing chest discomfort. On
physical examination, the pain was not relieved
by position change and increased continuously.
Blood pressure was 142/75 mm Hg and pulse
oximetry showed oxygen saturation to be 94%.
Chest auscultation was normal, as was chest X-ray.
Cardiomegaly and pneumothorax were absent and
the mediastinum was not widened.
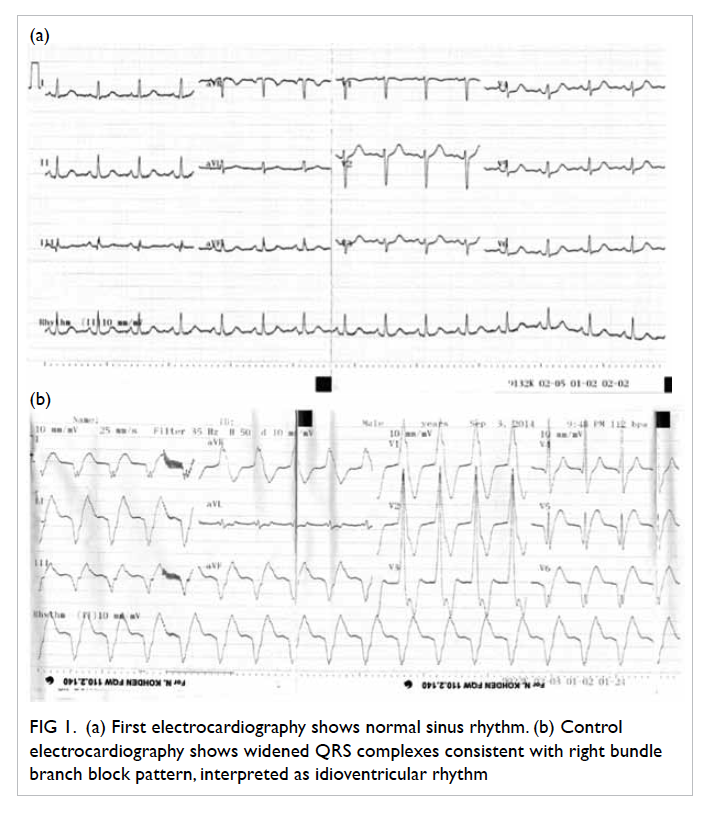
Figure 1. (a) First electrocardiography shows normal sinus rhythm. (b) Control electrocardiography shows widened QRS complexes consistent with right bundle branch block pattern, interpreted as idioventricular rhythm
Smoking was the only risk factor for developing
coronary artery disease in this young patient.
Hypertension, diabetes mellitus, hyperlipidaemia,
family history of heart disease, and obesity were
absent as risk factors for coronary artery disease.
The patient was thought to have myocarditis
and ibuprofen was prescribed for symptom relief. The
pain worsened, however, and ECG showed widened
QRS complexes (right bundle branch block pattern in
precordial derivations) with a rate of 112 beats/min
(Fig 1b). The ECG was interpreted as idioventricular rhythm. Bedside transthoracic echocardiography
was performed and left ventricular anterior wall
hypokinesis with 40% ejection fraction was observed.
Clopidogrel and acetylsalicylic acid were started
and immediate coronary angiography (CAG) was
performed to identify the cause. A significant stenosis
of the mid-segment of the left anterior descending
(LAD) artery with a fresh thrombus image was
present with distal TIMI-3 flow (Thrombolysis
In Myocardial Infarction grade 3, which implies
normal flow that fills the distal coronary bed
completely) [Fig 2a]. Right coronary artery and left circumflex artery were normal. Since the patient’s
haemodynamic parameters were stable with TIMI-3
distal blood flow in the LAD, conservative treatment
with intravenous glycoprotein 2b/3a (GP-2b3a)
inhibitor was prescribed. After successful infusion
of GP-2b3a without any complications, control CAG
was performed (Fig 2b). Complete dissolution of thrombus was observed and left ventricular anterior
hypokinesis was reversed.
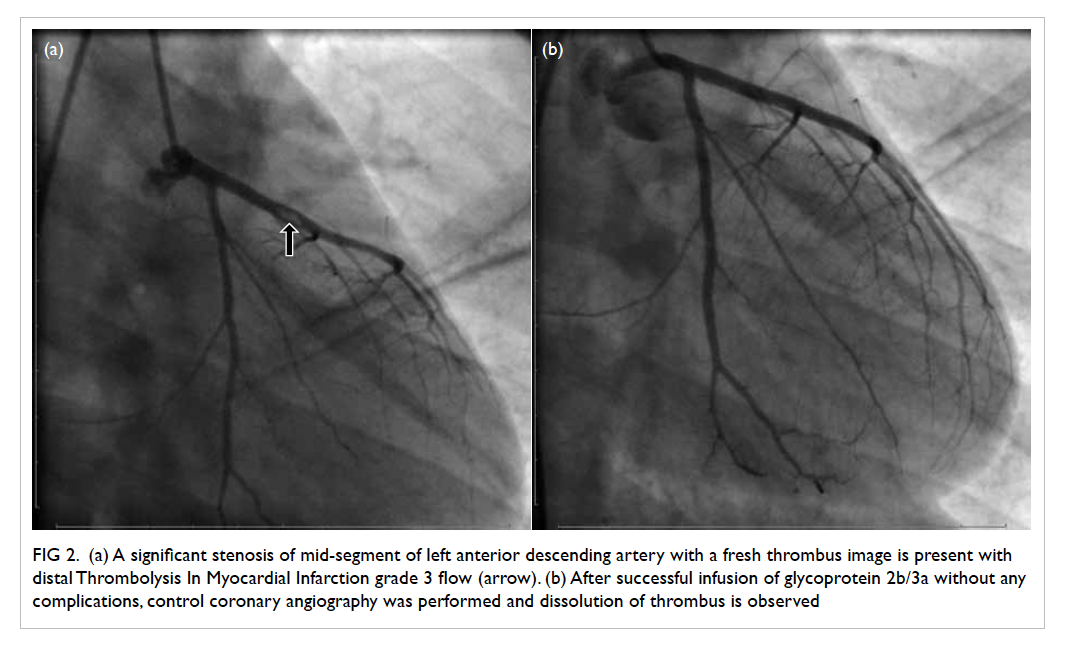
Figure 2. (a) A significant stenosis of mid-segment of left anterior descending artery with a fresh thrombus image is present with distal Thrombolysis In Myocardial Infarction grade 3 flow (arrow). (b) After successful infusion of glycoprotein 2b/3a without any complications, control coronary angiography was performed and dissolution of thrombus is observed
The patient’s laboratory findings were all
within normal range except markers of myocardial
damage. Troponin I level was 24 µg/L. Platelet
count and liver function tests were normal, as was
clotting panel. The patient’s blood was screened
for factor V Leiden mutation, prothrombin gene
mutation, MTHFR gene mutation, protein C activity,
protein S activity, plasminogen activator inhibitor–1
activity, homocysteine levels, and anti-cardiolipin
antibodies. No secondary aetiology was evident that
could account for such thrombus formation in an
18-year-old boy so he was further questioned about
drug use. This time he admitted the use of marijuana
1 hour prior to the onset of intense chest pain.
Discussion
Acute myocardial infarction (AMI) is the leading
cause of death in North America and Europe.1 Despite
this, AMI in an 18-year-old teenage boy is very rare.
In our case the possible causes of thrombophilia
were excluded and smoking of cannabis was thought
to be the main cause of AMI.
Recent cannabis use is associated with
acute coronary syndrome and can lead to severe
cardiovascular problems and sudden death, not only
in people at increased cardiovascular risk but also
in young people without any medical history or risk
factors.2 The effects of cannabinoids are primarily
mediated by the activation of cannabinoid receptors
that are present in a variety of tissues including the
brain (basal ganglia, pars reticulata of the substantia
nigra, entopeduncular nucleus, globus pallidus,
putamen, cerebellum, hippocampus, and cerebral
cortex) and cells of the immune system, spleen,
blood vessels, and the heart.3
The pharmacological effects of marijuana,
based on stimulation of cannabinoid receptors
CB1 and CB2 that are widely distributed in the
cardiovascular system, have been well described. A
dose-dependent increase in heart rate up to 100% of
basal rate occurs 10 to 30 minutes after beginning
to smoke.4 Most users experience an increase in
blood pressure especially while supine4 although
postural hypotension after smoking marijuana is
common. Tolerance to this drug can occur with
frequent repeated use.5 Another harmful effect of
smoked marijuana is associated with an increase in
carboxyhaemoglobin, resulting in decreased oxygen-carrying
capacity6 and subsequent demand-supply
mismatch by decreasing oxygen transportation
to the heart. This mechanism is suggested to
underlie atherosclerotic stable coronary disease
and concomitant cannabinoid use. Nonetheless in
our case, the patient was too young and the lesion
appearance on CAG was suggestive of a small plaque
rupture with superimposed thrombus formation
rather than stable atherosclerotic disease. Acute
myocardial infarction associated with cannabinoid
use and with normal coronary artery has been
reported in the literature. Ours is an interesting
case report associated with cannabinoid inhalation
and superimposed thrombus formation detected by
CAG. In our patient, implantation of a stent in the
LAD artery was not an option because the lesion
was thought to be thrombotic. Dissolution of the
thrombus was achieved with GP-2b3a infusion.
Clinicians are reminded of this very rare
aetiology of acute coronary syndrome and its
management among young patients. Bearing in mind
the increasing use of drugs such as marijuana and
other synthetic cannabinoids among young people,
management of associated cardiac problems is vital.
A CAG should be performed whenever drug abuse
is suspected in any patient who presents with chest
pain. If a thrombotic lesion is detected on CAG,
infusion of GP-2b3a may dissolve the thrombus.
References
1. Griffin BP, editor. Manual of cardiovascular medicine. 3rd
ed. Philadelphia: Lippincott Williams and Wilkins; 2009: 1.
2. Casier I, Vanduynhoven P, Haine S, Vrints C, Jorens PG.
Is recent cannabis use associated with acute coronary
syndromes? An illustrative case series. Acta Cardiol
2014;69:131-6.
3. Járai Z, Wagner JA, Varga K, et al. Cannabinoid-induced
mesenteric vasodilation through an endothelial site
distinct from CB1 or CB2 receptors. Proc Natl Acad Sci
USA 1999;96:14136-41. Crossref
4. Johnson S, Domino EF. Some cardiovascular effects of
marihuana smoking in normal volunteers. Clin Pharmacol
Ther 1971;12:762-8. Crossref
5. Benowitz NL, Jones RT. Cardiovascular effects of
prolonged delta-9-tetrahydrocannabinol ingestion. Clin
Pharmacol Ther 1975;18:287-97. Crossref
6. Aronow WS, Cassidy J. Effect of marihuana and placebo-marihuana
smoking on angina pectoris. N Engl J Med
1974;291:65-7. Crossref

