DOI: 10.12809/hkmj144415
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Familial eruptive syringoma
Mahizer Yaldiz, MD1; Cihan Cosansu, MD1;
Mustafa T Erdem, MD1; Bahar S Dikicier, MD1; Zeynep
Kahyaoğlu, MD2
1 Department of Dermatology, Sakarya
University Training and Research Hospital, Sakarya, Turkey
2 Department of Pathology, Sakarya
University Training and Research Hospital, Sakarya, Turkey
Corresponding author: Dr Mahizer Yaldiz (drmahizer@gmail.com)
Case presentations
Case 1
A 20-year-old woman presented with a 4-year history
of progressive papular rash in January 2010. The rash had started on her
neck. The patient was otherwise healthy and had no other skin complaints
and no family history of any skin diseases. She reported that her brother
had similar lesions. Physical examination of the patient revealed widely
distributed flesh-coloured red-brown smooth papules of 1 to 5 mm on the
neck and supraclavicular region (Fig 1a). Skin biopsy and subsequent
histopathological examination revealed dermis that was filled with
multiple ducts embedded in a dense collagenous stroma. The ducts were
lined by an inner layer of flattened epithelial cells that had a
comma-like appearance. Syringoma was diagnosed (Fig 1b).
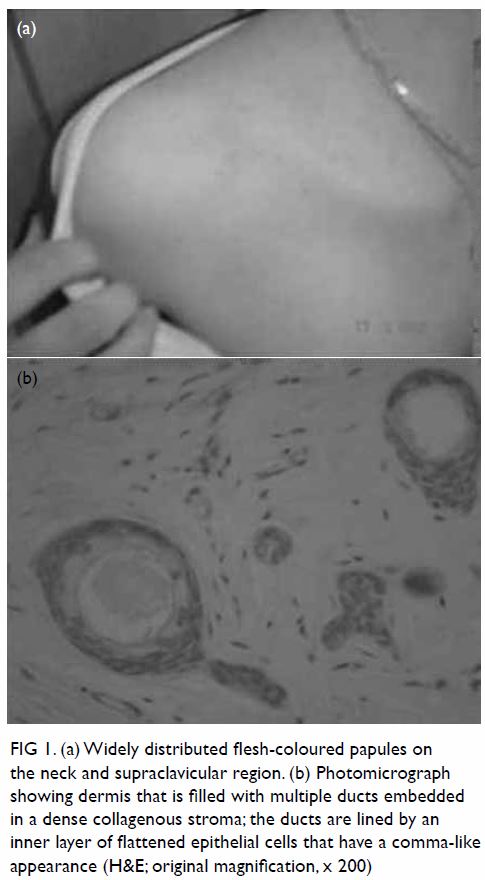
Figure 1. (a) Widely distributed flesh-coloured papules on the neck and supraclavicular region. (b) Photomicrograph showing dermis that is filled with multiple ducts embedded in a dense collagenous stroma; the ducts are lined by an inner layer of flattened epithelial cells that have a comma-like appearance (H&E; original magnification, x 200)
Case 2
A 25-year-old man, the brother of the patient in
case 1, presented with a 10-year history of progressive papular rash in
January 2010. The rash had started on the back and upper chest. The
patient was otherwise healthy, with no other skin complaints and a
negative family history for any skin diseases, other than his sister.
Physical examination revealed widely distributed, flesh-coloured brown
papules of 1 to 5 mm on the anterior and posterior aspect of the trunk (Fig 2a). Histopathological examination revealed that
the dermis was filled with multiple ducts embedded in a collagenous stroma
and the ducts were lined by an inner layer of flattened epithelial cells
that had a comma-like appearance (Fig 2b).
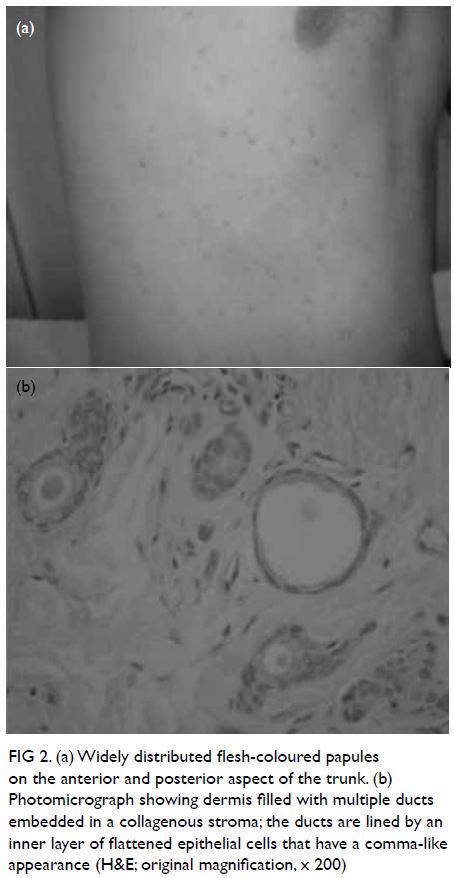
Figure 2. (a) Widely distributed flesh-coloured papules on the anterior and posterior aspect of the trunk. (b) Photomicrograph showing dermis filled with multiple ducts embedded in a collagenous stroma; the ducts are lined by an inner layer of flattened epithelial cells that have a comma-like appearance (H&E; original magnification, x 200)
On the basis of the clinical and histopathological
findings, both cases were diagnosed as familial eruptive syringoma.
Because this condition is benign, treatment modalities were discussed with
both patients, with particular reference to ‘poor’ cosmetic outcome and
the risk of recurrence. Both patients opted for no intervention. They were
advised to avoid hot environments as much as possible and were given an
open appointment at the dermatology department.
Discussion
The word syringoma is derived from the Greek word syrinx
meaning pipe or tube.1 Syringoma is
a benign adnexal neoplasm that is formed by well-differentiated ductal
elements. Lesions have largely cosmetic significance and affect
approximately 1% of the population.1
2 Syringomas usually first appear
at puberty and are generally asymptomatic; additional lesions can develop
later. Neither of our patients had any symptoms, although rarely
individuals may experience pruritus, especially during perspiration.2 Clinically, syringomas manifest as small skin-coloured
or slightly pigmented papules. Although the peri-orbital region is the
most commonly involved site, the neck, supraclavicular region, and the
anterior and posterior aspect of the trunk may also be affected,
especially in the eruptive form, as seen in our patients.
Syringomas are classified into four clinical types:
localised, familial, generalised, and Down’s syndrome–associated. The
generalised type encompasses multiple and eruptive syringomas.3 Eruptive syringoma is a rare variant that was first
described by Jacquet and Darier in 1887.4
The lesions in eruptive syringoma occur in large numbers and in successive
crops at puberty or during childhood. They can occur on the anterior
chest, neck, upper abdomen, axillae, and the periumbilical region. They
are almost always multiple and most frequently occur on the eyelids and
upper cheeks. Eruptive syringomas are described more frequently in
patients with Down’s syndrome and Ehlers-Danlos syndrome.5 In our patients, there was no such association.
Rarely, a patient with eruptive syringomas may have
a family history of similar lesions. Familial eruptive syringoma is a rare
condition that is likely to be inherited in an autosomal dominant manner.
To the best of our knowledge, only a few cases of familial eruptive
syringoma have been reported worldwide. Our two patients represent typical
cases of familial eruptive syringomas. Reed6
described a family in which seven females and one male in four generations
were affected. Patrone and Patrizi7
reported on a family (mother, daughter, and son) with dominantly inherited
eruptive syringoma. Marzano et al2
reported on a family with multiple syringomas that affected members of
three successive generations, and described in detail a 36-year-old woman
and her 17-year-old son. Lau and Haber8
reported two cases of eruptive syringoma within a family, in which the
lesions were widely distributed over the trunk of a healthy 16-year-old
female and her 19-year-old brother.
Skin biopsies of the lesions are the best means of
diagnosing syringoma, because the microscopic appearance is characteristic
of the condition. Histologically, syringomas are characterised by dilated
cystic spaces lined by two layers of cuboidal cells and epithelial strands
of similar cells. Some of the cysts have what resemble small tails that
look like commas or tadpoles, and in a group they produce a distinctive
paisley-like pattern. There is also a dense fibrous stroma.
The differential diagnosis of eruptive syringomas
must be made while considering other papular dermatosis that frequently
appear during childhood—for example, plane warts, acne vulgaris, lichen
planus, granuloma annulare, papular sarcoidosis, milia, sebaceous
hyperplasia, eruptive xanthoma, urticaria pigmentosa, Darier’s disease,
pseudoxanthoma elasticum, or hidrocystoma. Histological differential
diagnoses include sclerosing (morphea-like) basal-cell carcinoma and
desmoplastic trichoepithelioma. Importantly, syringoma must be
distinguished from microcystic adnexal carcinoma, which has similar
histological features but tends to infiltrate the deep dermis and
subcutaneous tissue.
Despite the availability of numerous treatment
options, their efficacy is limited because the tumours are located in the
dermis and the risk of recurrence is high. Treatment is difficult,
although many lesions respond to very light electrodessication or removal
by shaving. Carbon dioxide laser treatment by the pinhole method and
fractional thermolysis have been reported to be effective in removal. For
larger lesions, surgical removal may be considered. Other treatment
modalities that have been used include cryosurgery, chemical peeling,
dermabrasion, and oral and topical retinoids.9
Our two patients initially requested treatment but then opted for no
intervention.
References
1. Haubrich W. Medical Meaning: A Glossary
of Word Origins. US: American College of Physicians; 2003: 233.
2. Marzano AV, Fiorani R, Girgenti V,
Crosti C, Alessi E. Familial syringoma: report of two cases with a
published work review and the unique association with steatocystoma
multiplex. J Dermatol 2009;36:154-8. Crossref
3. Friedman SJ, Butler DF. Syringoma
presenting as milia. J Am Acad Dermatol 1987;16:310-4. Crossref
4. Jacquet L, Darier J. Hiydradénomes
éruptifs, épithéliomes adénoides des glandes sudoripares ou adénomes
sudoripares. Ann Dermatol Syph 1887;8:317-23.
5. Hertl-Yazdi M, Niedermeier A, Hörster S,
Krause W. Penile syringoma in a 14-year-old boy. Eur J Dermatol
2006;16:314-5.
6. Reed WB. Genetic aspects in dermatology
[in German]. Hautarzt 1970;21:8-16.
7. Patrone P, Patrizi A. Familial eruptive
syringoma [in Italian]. G Ital Dermatol Venereol 1988;123:363-5.
8. Lau J, Haber RM. Familial eruptive
syringomas: case report and review of the literature. J Cutan Med Surg
2013;17:84-8. Crossref
9. Garrido-Ruiz MC, Enguita AB, Navas R,
Polo I, Rodríguez Peralto JL. Eruptive syringoma developed over a waxing
skin area. Am J Dermatopathol 2008;30:377-80. Crossref

