Hong Kong Med J 2018 Apr;24(2):158–65 | Epub 4 Apr 2018
DOI: 10.12809/hkmj176823
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Endobronchial valve for treatment of persistent air
leak complicating spontaneous pneumothorax
WC Yu, MB, BS, FHKCP1; Ellen LM Yu, MSc2;
HC Kwok, MB, BS, FHKCP1; HL She, MB, BS, FRCR3; KK
Kwong, MB, BS, FHKCP1; YH Chan, MB, BS, FHKCP1; YL
Tsang, BSc4; YC Yeung, MB, BS, FHKCP1
1 Department of Medicine and Geriatrics,
Princess Margaret Hospital, Laichikok, Hong Kong
2 Clinical Research Centre, Princess
Margaret Hospital, Laichikok, Hong Kong
3 Department of Radiology, Princess
Margaret Hospital, Laichikok, Hong Kong
4 Central Endoscopy Unit, Princess
Margaret Hospital, Laichikok, Hong Kong
Corresponding author: Dr WC Yu (h7537800@connect.hku.hk)
Abstract
Introduction: Endobronchial
one-way valves have been proposed as treatment for persistent air leak
complicating spontaneous pneumothorax in which surgical intervention is
not feasible. However, published data on efficacy, safety, and factors
associated with success are scanty.
Methods: This is a retrospective
study of 37 patients at a general hospital from 2008 to 2016. The impact
of endobronchial valve implantation on the time to air-leak cessation
after bronchoscopy was evaluated.
Results: The median patient age
was 71 years. The majority of patients were males (92%), were
ever-smokers (83%), had at least one co-morbidity (97%), and had
secondary spontaneous pneumothorax (89%). Nineteen patients (51%) had a
mean of 2.6 endobronchial valves implanted (range, 1-6). The air leak
ceased within 72 hours for only eight patients (22% of the complete
cohort), with immediate air-leak cessation after completion of
endobronchial valve implantation. All six successful cases that had
computed tomographic data of the thorax were shown to have bilateral
intact interlobar fissures. The median (interquartile range) Charlson
co-morbidity index was 1 (0.25-1) and 2 (1-3) for the success group and
failure group, respectively (P=0.029). All patients in the
no-endobronchial valve group survived, whereas three patients in the
endobronchial valve group died within 30 days of endobronchial valve
implantation.
Conclusion: Only a small
proportion of cases of endobronchial valve implantation for air leak
complicating pneumothorax had unequivocal success. Intact bilateral
interlobar fissures appear to be a necessary, though not sufficient,
condition for success. Patients with fewer medical co-morbidities and
immediate air-leak cessation after endobronchial valve implantation have
a higher likelihood of success.
New knowledge added by this study
- Only a small proportion of cases (22%) of persistent air leak complicating spontaneous pneumothorax can be successfully treated by endobronchial valve (EBV).
- Cases in which the air leak does not cease immediately after completion of EBV implantation are likely to fail.
- Patients with any non-intact interlobar fissures are likely to experience treatment failure.
- EBV treatment may be attempted in patients with persistent air leak complicating spontaneous pneumothorax who are not candidates for surgery, have intact interlobar fissures, and do not have severe medical comorbidities.
- Plain computed tomography of the thorax should be performed to routinely assess patients who are candidates for EBV treatment.
- Cases of completed EBV implantation that still have an air leak may have the EBVs removed.
Introduction
Persistent air leak is a common complication of
spontaneous pneumothorax being treated by chest tube drainage. In one
report, the median time for spontaneous cessation of air leak was 7 days
for primary spontaneous pneumothorax and 11 days for secondary spontaneous
pneumothorax.1 In another report,
75% and 100% of cases of primary spontaneous pneumothorax resolved by 7
days and 14 days, respectively, whereas the corresponding proportions for
secondary spontaneous pneumothorax were 61% and 79%, respectively.2 It is generally recommended that surgical intervention
be considered when an air leak continues for 7 to 14 days after chest tube
insertion. Unfortunately, some patients are poor candidates for surgery,
and some patients may refuse surgery. Prolonged chest tube in situ,
however, is undesirable because of an increased risk of complications,
prolonged immobilisation and its consequences, and increased duration of
hospital stay. Alternative means to shorten the duration of air leakage
are thus needed.
Endobronchial one-way valves (EBVs) have been used
to treat persistent air leak complicating pneumothorax. The rationale is
that air leakage will stop if air is prevented from entering the airway
leading to the leak site. Preliminary case reports showed encouraging
results.3 4 5 6 7 8 9 10 11 12 13 14 Larger case series showed similarly favourable
results.15 16 17 18 19 20 21 22 23 However,
most of these reports include a mix of post-surgical pneumothoraces,
spontaneous pneumothoraces, and other aetiologies. Moreover, there is
scanty information on overall efficacy, short-term safety, and factors
related to favourable clinical outcomes.
The Princess Margaret Hospital, an acute-care
general hospital in Hong Kong, has been using EBV for persistent air leak
complicating pneumothorax on compassionate grounds since 2008, and its
preliminary experience on three apparently successful cases was reported
in 2009.11 However, it was
subsequently found that in many cases, the leak site could not be
identified, so EBV could not be deployed. In some other cases, despite
leak site identification and EBV deployment, the air leak may not resolve
completely, or it may recur after a few hours. We therefore hypothesise
that EBV treatment has a low success rate in real-life situations. To test
this hypothesis, we retrospectively compared the clinical course of
patients with and without EBV use for persistent air leak complicating
spontaneous pneumothorax during an 8-year period at a single centre.
Methods
Patients
This retrospective chart review was based on
patients who were managed at the Princess Margaret Hospital from May 2008
to April 2016. Eligible patients were those with spontaneous pneumothorax
who were undergoing chest tube drainage and who had had an air leak
lasting more than 1 week. All showed bubbling in the drainage bottle
during both expiration and inspiration, with water suction at -20 cm.
Patients either refused surgery or were considered by the thoracic surgeon
to be unsuitable for surgical intervention owing to advanced age, poor
lung function, major medical co-morbidities, or a combination of these.
Intervention
Bronchoscopy with the intention of EBV implantation
to stop the air leak was suggested to eligible patients. Some were
reluctant at first but consented after further days of air leakage.
Procedures for identifying the leak site and deploying EBV were as
described previously.11 Briefly,
an endobronchial inflatable balloon was used to occlude lobar or segmental
bronchi sequentially. If bubbling from the chest drainage bottle stopped,
or was greatly reduced, then the lobe or segment was selected for
endobronchial valve implantation. The Zephyr EBV (Emphasys Inc, now
Pulmonx Inc, Redwood City [CA], United States) was used throughout.
Patients were observed closely for continued air leak after bronchoscopy.
Chest tubes were removed as soon as possible after air-leak cessation,
typically within 1 or 2 days, as is usual clinical practice.
Data collection and outcome measures
Data on demographic and disease characteristics,
details of bronchoscopy, and survival after bronchoscopy were recorded.
Spirometry data were analysed if available within 1 year of bronchoscopy.
Spirometry was performed according to the American Thoracic Society /
European Respiratory Society criteria24
and using reference values for Hong Kong adults.25
No spirometry was performed during the period of chest tube drainage or
with EBV in situ. Computed tomography images, if available, were viewed in
axial, sagittal, and coronal planes by a single radiologist who was
blinded to other study data. The integrity of the fissures was defined as
more than 90% completeness on at least one axis.26
Outcome measures included whether EBV was implanted, time to air-leak
cessation, and 30-day all-cause mortality after bronchoscopy.
Definition of therapeutic success
Therapeutic success was defined as cessation of the
air leak within 72 hours of EBV implantation. Cases with EBV implanted but
with the air leak lasting more than 72 hours afterwards, cessation of air
leak within 72 hours of bronchoscopy owing to other interventions (such as
surgery), cases without EBV implantation, and cases of chest tube removal
while the air leak persisted (such as following unintended displacement)
were considered cases of failure.
Statistical analysis
The Mann-Whitney U test and Fisher’s exact
test were used to examine differences between groups. The Kaplan-Meier
log-rank test and Gehan-Breslow-Wilcoxon test were used to analyse time to
air-leak cessation after first bronchoscopy among patients with and
without EBV implantation. The association between EBV implantation and
air-leak cessation was assessed in a multivariable Cox proportional
hazards regression model that was adjusted for ‘days on chest tube before
first bronchoscopy’ and factors with P<0.2 in univariable regression
analyses. The accuracy, sensitivity, specificity, and positive and
negative predictive values of using the presence of an intact interlobar
fissure as an indicator of a successful outcome were calculated.
Statistical analyses were performed using SPSS 22.0 for Windows (IBM
Corp., Armonk [NY], United States) and OpenEpi: Open Source Epidemiologic
Statistics for Public Health, version 3.01 (http://www.openepi.com).
Statistical significance was set at P<0.05.
This study was approved by the Research Ethics
Committee of the Kowloon West Cluster of the Hong Kong Hospital Authority,
with the requirement for patient consent waived. This report conforms to
the STROBE 2008 guidelines.27
Results
Baseline characteristics
During the study period, 38 patients underwent
bronchoscopy for persistent air leak complicating spontaneous pneumothorax
at our institution. One patient was excluded because the air leak was
subsequently found to result from the chest tube having been inserted into
an airway. Of the remaining 37 patients, 35 were assessed by the surgeon
and considered unfit for surgery, and two patients with primary
spontaneous pneumothorax refused surgery. The median patient age was 71
years and most (34; 92%) were males. The majority (83%) were ever-smokers.
All but one (97%) had at least one co-morbidity and the median Charlson
co-morbidity index was 1. Fifteen patients (41%) had a left pneumothorax.
Thirty-three (89%) had secondary spontaneous pneumothorax, of which 23 had
chronic obstructive pulmonary disease with or without other lung diseases.
Of the 22 secondary spontaneous pneumothorax cases with spirometric data,
the median forced expiratory volume in 1 second (FEV1) was 0.94
L; median percentage of predicted FEV1 was 43.5%; and median
FEV1 to forced vital capacity ratio was 0.45. Eleven patients
(30%) had at least one attempt at talc pleurodesis before bronchoscopy.
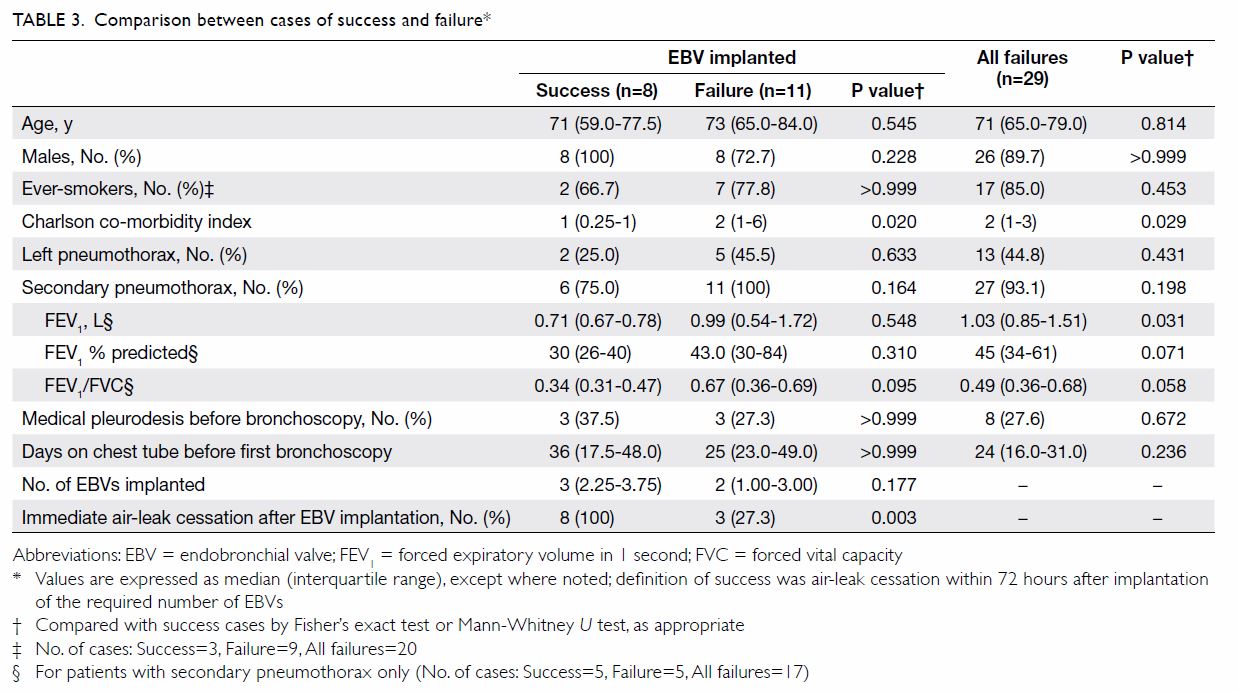
The median number of days off chest tube use before bronchoscopy was 25 (Table 1).
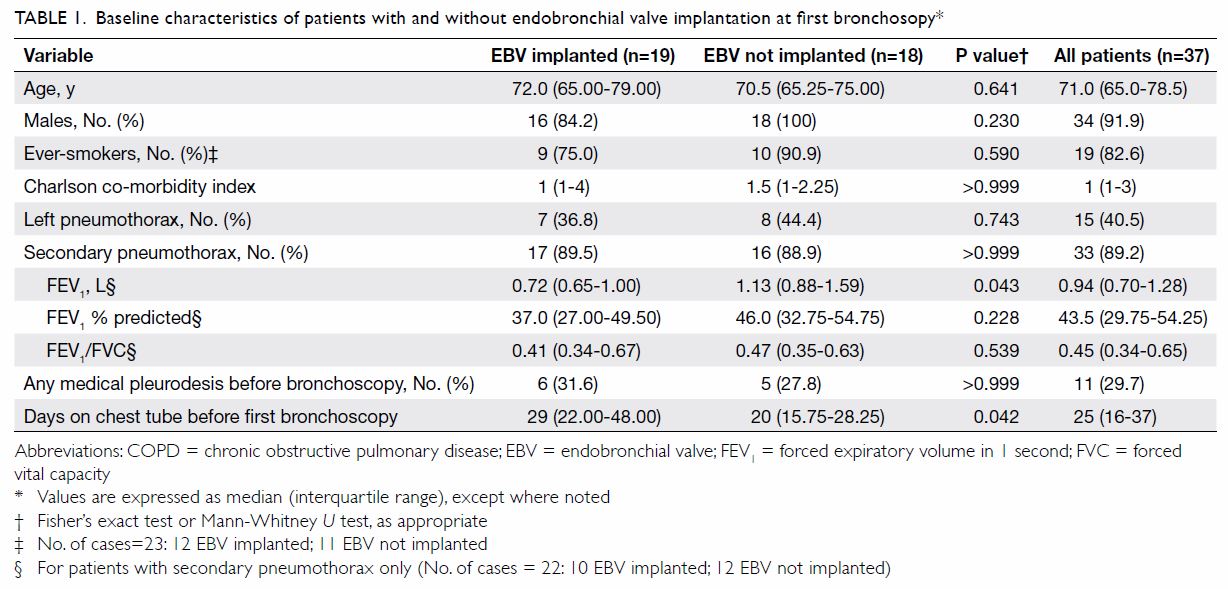
Table 1. Baseline characteristics of patients with and without endobronchial valve implantation at first bronchosopy
Endobronchial one-way valve implantation and time to
air-leak cessation
Nineteen patients (51%) had a mean of 2.6 EBVs
implanted (range, 1-6). The sites of EBV implantation were as follows: 11
in the right upper lobe, one in the right middle lobe, none in the right
lower lobe, five in the left upper lobe, and two in the left lower lobe.
Of the 18 patients without an EBV implanted, the target site for EBV
implantation could not be identified in 17. In the remaining patient,
despite identification of the air leak in the left upper lobe, EBV
implantation was followed by severe oxygen desaturation and had to be
abandoned.
There were eight successful cases among patients
with EBVs implanted. Among these, seven patients had immediate and lasting
cessation of the air leak, and the chest tube was removed within 2 days.
One patient had immediate air-leak cessation but there was recurrence
after 2 hours. The air leak subsided completely within 72 hours, and the
chest tube was removed on day 4. Among the 11 cases of failure after EBV
implantation, the air leak stopped immediately in three cases but recurred
soon after and persisted beyond 72 hours. In the other eight cases, the
air leak was reduced temporarily but was present beyond 72 hours. In the
group without an implanted EBV, the earliest time for air-leak cessation
was day 5, and the chest tube was removed on day 8. In a Kaplan-Meier
comparison of the EBV and no-EBV groups in the number of days from first
bronchoscopy to air-leak cessation, the EBV group did better in the first
30 days, but the no-EBV group caught up by day 45. There was a
statistically significant difference between the two groups according to
the Gehan-Breslow-Wilcoxon test (P=0.027), but not the log-rank test
(P=0.138) [Fig Part a]. When the same comparison was done with
the eight successful cases removed from the EBV group, the two curves
overlapped throughout and there was no statistically significant
difference between the two groups (P=0.881 by Gehan-Breslow-Wilcoxon test
and P=0.976 by log-rank test) [Fig Part b].
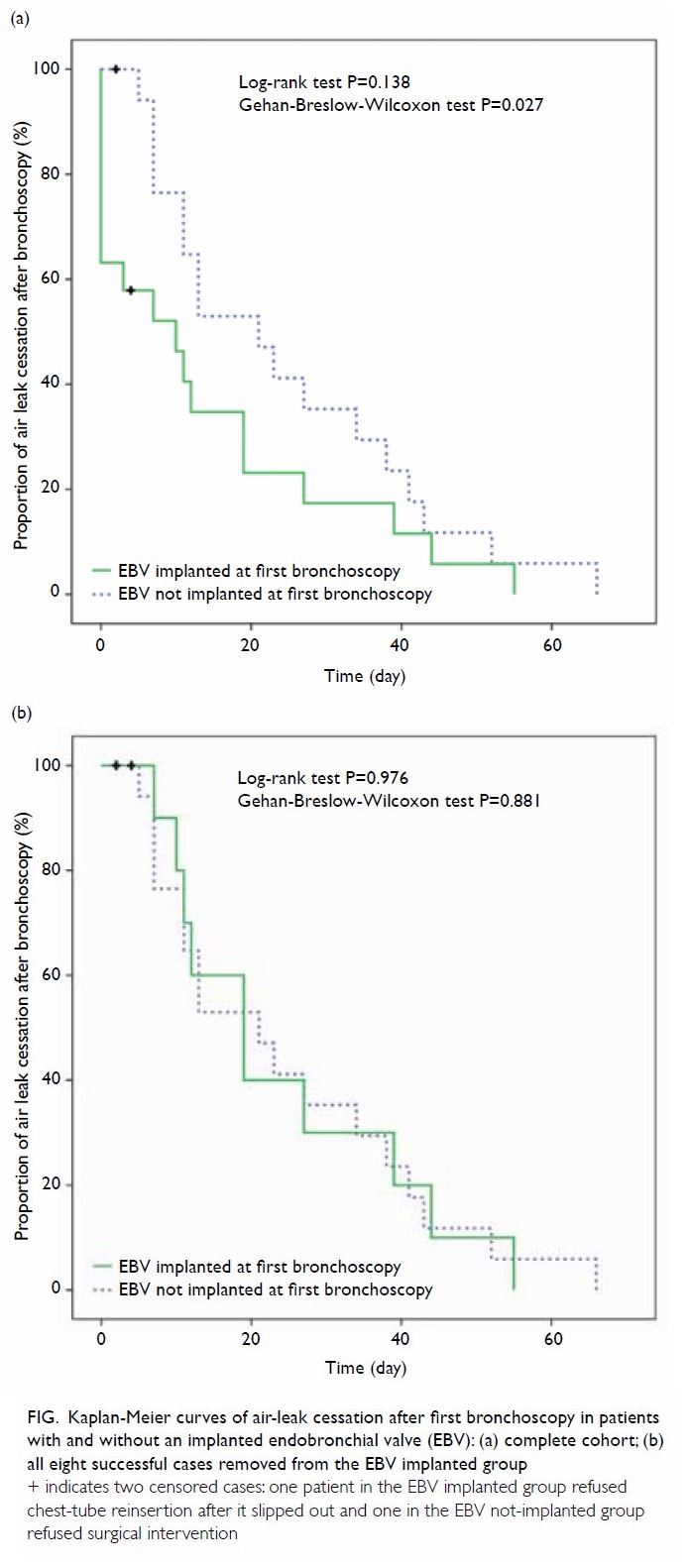
Figure. Kaplan-Meier curves of air-leak cessation after first bronchoscopy in patients with and without an implanted endobronchial valve (EBV): (a) complete cohort; (b) all eight successful cases removed from the EBV implanted group
In a comparison of demographic and clinical
characteristics between the EBV group and the no-EBV group, the former had
a significantly poorer FEV1, but not percentage of predicted
FEV1. This group also had the chest tube in place for a
significantly longer duration before bronchoscopy (Table 1).
Factors associated with a successful outcome
We further examined factors related to air-leak
cessation after first bronchoscopy by Cox proportional hazards regression
analysis. The implantation of an EBV was significantly associated with
air-leak cessation (adjusted hazard ratio=2.39, 95% CI=1.13-5.05;
P=0.023), whereas the Charlson co-morbidity index was significantly
associated with delayed air-leak cessation (adjusted hazard ratio=0.78,
95% CI=0.63-0.97; P=0.026). The number of days of chest tube use before
first bronchoscopy was not associated with air-leak cessation (Table
2).
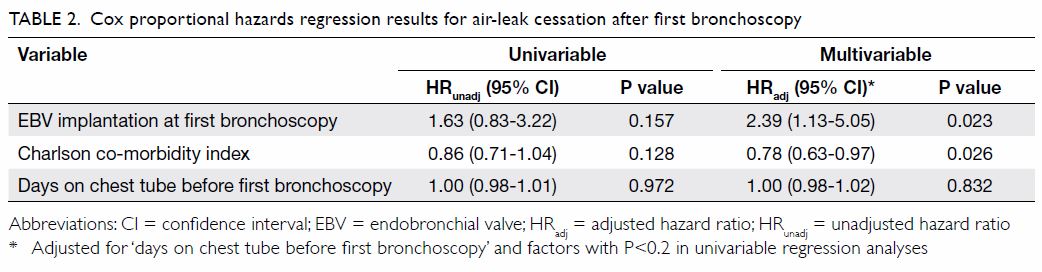
Table 2. Cox proportional hazards regression results for air-leak cessation after first bronchoscopy
When comparing the eight successful cases with the
11 failed cases among those with implanted EBVs, we found no difference in
any of the demographic or disease variables between the two groups, apart
from the Charlson co-morbidity index, which was significantly lower for
the success group (Table 3). Additionally, all eight patients (100%) in
the success group had air-leak cessation immediately after EBV
implantation, versus only three of 11 (27%) in the failure group
(P=0.003). When we compared the eight successful cases with all 29 failed
cases, again the median (interquartile range) Charlson co-morbidity index
was significantly lower for the success group: 1 (0.25-1) vs 2 (1-3)
[P=0.029]. This group also had significantly poorer FEV1, but
not in percentage of predicted FEV1, and showed a trend towards
more severe airflow obstruction, although this did not reach statistical
significance (Table 3).
Twenty-three patients had thoracic computed
tomography performed to examine the integrity of interlobar fissures. For
the 13 patients with all fissures intact, six had an EBV implanted and
were classed as successful cases, four had EBV implanted but were classed
as failed cases, and three did not have an EBV implanted. There were five
patients each in the group with any non-intact ipsilateral fissure and in
the group with any non-intact contralateral fissure. Both groups had two
patients with an implanted EBV and three without, and all experienced
treatment failure.
When using the presence of all intact fissure(s) to
screen for successful EBV treatment among the 23 patients who had
undergone thoracic computed tomography, the accuracy was 69.6%, the
sensitivity and negative predictive value were both 100%, and the
specificity and positive predictive value were 58.8% and 46.2%,
respectively (Table 4). When the criterion for success was
immediate air-leak cessation after EBV implantation, the accuracy among
the 19 patients with an implanted EBV was 84.2%, the sensitivity and
negative predictive value remained at 100%, and both the specificity and
positive predictive value were 72.7% (Table 4).
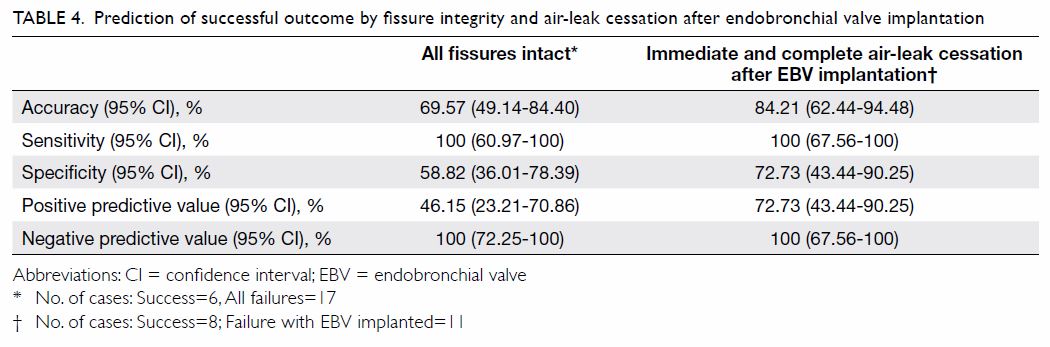
Table 4. Prediction of successful outcome by fissure integrity and air-leak cessation after endobronchial valve implantation
Adverse events and mortality
There was no incident of valve displacement,
bleeding, or post-obstructive pneumonia. Three patients died within 30
days of EBV implantation and all had advanced age and multiple
co-morbidities (Table 5). In two patients, the causes of death were
clearly related to ongoing pre-existing disease. One patient had a sudden
cardiac arrest on day 29 after being successfully treated with EBV,
although the relationship of death to EBV was uncertain. The earliest
death in the no-EBV group occurred on day 43 after bronchoscopy and the
cause of death was lung cancer.
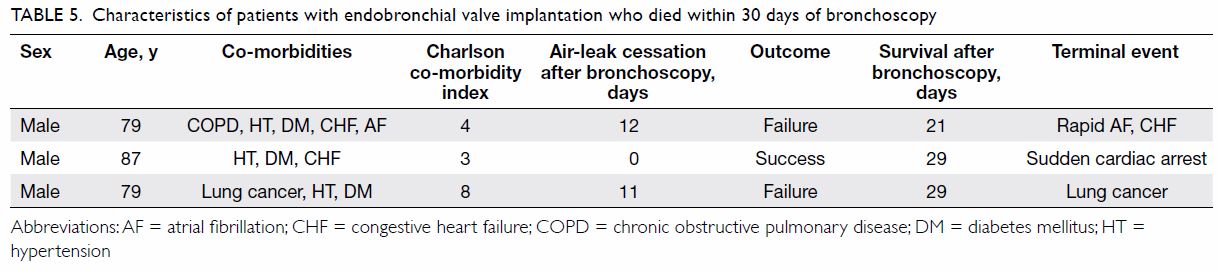
Table 5. Characteristics of patients with endobronchial valve implantation who died within 30 days of bronchoscopy
Subsequent treatments
Three patients underwent a second bronchoscopy
after the first one failed, with one success and two failures. Sixteen
patients received talc pleurodesis (median, 2 times; range, 1-5 times).
One young patient with primary spontaneous pneumothorax underwent surgery
2 days after failed identification of the leak site by bronchoscopy.
Seventeen patients did not receive any further treatment, mostly owing to
early air-leak cessation.
Implant removal
Thirteen patients had their implanted EBVs removed
after a median of 43 days (range, 21-155 days). For the remaining six
patients, three died within 30 days before EBV removal was considered.
Another patient had a second bronchoscopy with an additional EBV implanted
but died within 30 days of the second bronchoscopy. The fifth patient had
advanced lung cancer and removal of EBV was deemed unnecessary; she died 9
months after bronchoscopy. The sixth patient had severe chronic
obstructive pulmonary disease and there was subjective improvement of
respiratory and health status after EBV implantation, so it was decided
that the EBV should remain in situ indefinitely.
Discussion
We have reported the first real-life cohort study
that consisted entirely of spontaneous pneumothorax cases with persistent
air leak treated with EBV. Our results confirm those of previous reports
that EBV can be useful in hastening air-leak cessation in patients with
this condition. Nonetheless, it also highlights the fact that failures are
common. A site for EBV implantation was not identified in nearly half of
the patients. For the 19 patients with an EBV implanted, only eight (42%)
had a clear success. The overall success rate was thus only 22%.
In this retrospective study, we attempted to assess
the efficacy of EBV treatment by comparing those who had an EBV implanted
with those in whom EBV implantation was denied owing to inability to
identify an implantation site or lung function that was too poor. This
design is obviously inferior to a prospective randomised design.
Nevertheless, the two study groups had a similar number of patients who
were similar in many demographic and disease aspects. The Kaplan-Meier
comparison suggested that EBV treatment is efficacious in hastening
air-leak cessation. The significantly longer duration of air leakage
before first bronchoscopy for the EBV group is a potential confounder,
because the longer the air leak exists, the higher the probability that
spontaneous resolution will occur. Nonetheless, the Cox hazards regression
analysis suggested that it was not a significant factor. This finding also
lends further support to the efficacy of EBV implantation in enabling
early air-leak cessation.
A definition of success for using EBV implantation
to treat persistent air leak complicating pneumothorax is difficult to
formulate and has seldom been discussed in previous studies. Our criteria
of cessation of air leak within 72 hours was arbitrary but is supported by
our observation that patients who did not meet the criteria behaved almost
exactly as if no EBV was implanted. This finding suggests that for cases
in which EBV is implanted but fails, other forms of treatment should be
sought early.
One interesting finding is that higher co-morbidity
burden seemed to be a risk factor for delayed air-leak cessation,
irrespective of EBV implantation status. Delayed cessation of air leak may
be translated as delayed healing of the lesion responsible for the air
leak, which is expected in patients with more co-morbidities and who are
thus usually sicker. Nonetheless, our study was not designed to examine
this association, and a properly designed study would be needed to provide
definitive answers.
It has been widely accepted that fissure
completeness of the target lobe is strongly correlated with significant
lobar collapse after implantation of EBVs for volume reduction in severe
pulmonary emphysema.28 29 The same is probably true for EBV treatment of
persistent air leak complicating pneumothorax, although as far as we are
aware there are no published data on this. Not surprisingly, our results
showed that intact interlobar fissures were a necessary, but not
sufficient, condition for a successful outcome. However, an interesting
and unexpected finding is that patients with a non-intact fissure in the
contralateral lung, but intact fissure in the ipsilateral lung, behaved
similarly to those with a non-intact fissure in the ipsilateral lung. We
have no explanation for this, and these findings need to be confirmed with
larger studies.
Immediate cessation of air leak after completion of
EBV implantation was strongly predictive of a successful outcome.
Importantly, all eight patients with an implanted EBV and without
immediate cessation of air leak failed to respond to treatment. In such
cases, the EBV should have been removed immediately to save costs and to
avert possible adverse events associated with EBVs. A further implication
is that stringent balloon testing of cessation of air leak should be
performed and, in the presence of any uncertainty, EBVs should not be
implanted.
In all our patients, we encountered no adverse
events directly attributable to EBVs. Nonetheless, the three early deaths
within 30 days of EBV implantation is worrying. The causes of death in two
cases were clearly the severe pre-existing illness, but the possibility
that recent EBV implantation hastened the terminal event cannot be
excluded. The case of sudden cardiac death raises suspicion that the
implanted EBV was implicated. More data are needed to determine whether
EBV implantation is associated with increased early mortality.
There were several limitations to our study. First,
it was a retrospective one, so some data were unavailable. Second, it was
not a randomised controlled study. Third, it was a single-centre study,
making the data less generalisable to a wider setting. Still,
single-centre retrospective case series do have the advantage that
practices are more uniform and results easier to interpret. Fourth, our
case series was small, making it difficult to identify definitive factors
associated with clinical outcomes. Fifth, some groups had a very small
number of patients, and especially of females, patients with primary
spontaneous pneumothorax, and patients with a lesion in the lower lobes.
Finally, chart review and data collection (besides radiological data) were
performed by an investigator who was not blinded to the study outcomes,
and this may have been a source of bias.
We conclude that EBV implantation via the flexible
bronchoscope can be useful in hastening air-leak cessation in patients
with persistent air leak complicating spontaneous pneumothorax. Only about
one-fifth of subjects, however, showed unequivocal benefit, and safety of
this form of treatment needs further evaluation. Bilateral intact
interlobar fissures seem to be a necessary, though not sufficient,
condition for treatment success, and patients with fewer medical
co-morbidities and immediate air-leak cessation after completion of EBV
implantation seem to have a higher likelihood of treatment success.
Further evaluation by randomised controlled trials is warranted.
Acknowledgements
We thank the doctors and nurses of the Respiratory
Team, Princess Margaret Hospital, for taking care of the patients, and
nurses of the Central Endoscopy Unit, Princess Margaret Hospital, for
providing technical support for the bronchoscopy procedures.
Declaration
The authors have no conflicts of interest to
disclose.
References
1. Mathur R, Cullen J, Kinnear WJ, Johnston
ID. Time course of resolution of persistent air leak in spontaneous
pneumothorax. Respir Med 1995;89:129-32. Crossref
2. Chee CB, Abisheganaden J, Yeo JK, et al.
Persistent air-leak in spontaneous pneumothorax—clinical course and
outcome. Respir Med 1998;92:757-61. Crossref
3. Snell G, Holsworth L, Fowler S, et al.
Occlusion of a broncho-cutaneous fistula with endobronchial one-way
valves. Ann Thorac Surg 2005;80:1930-2. Crossref
4. Ferguson JS, Sprenger K, Van Natta T.
Closure of a bronchopleural fistula using bronchoscopic placement of an
endobronchial valve designed for the treatment of emphysema. Chest
2006;129:479-81. Crossref
5. Mitchell KM, Boley TM, Hazelrigg SR.
Endobronchial valves for treatment of bronchopleural fistula. Ann Thorac
Surg 2006;81:1129-31. Crossref
6. Feller-Kopman D, Bechara R, Garland R,
Ernst A, Ashiku S. Use of a removable endobronchial valve for the
treatment of bronchopleural fistula. Chest 2006;130:273-5. Crossref
7. Fann JI, Berry GJ, Burdon TA. The use of
endobronchial valve device to eliminate air leak. Respir Med
2006;100:1402-6. Crossref
8. Anile M, Venuta F, De Giacomo T, et al.
Treatment of persistent air leakage with endobronchial one-way valves. J
Thorac Cardiovasc Surg 2006;132:711-2. Crossref
9. Toma TP, Kon OM, Oldfield W, et al.
Reduction of persistent air leak with endoscopic valve implants. Thorax
2007;62:830-3. Crossref
10. Santini M, Fiorelli A, Vicidomini G,
Laperuta P, Di Crescenzo VG. Iatrogenic air leak successfully treated by
bronchoscopic placement of unidirectional endobronchial valves. Ann Thorac
Surg 2010;89:2007-10. Crossref
11. Yu WC, Yeung YC, Chang Y, et al. Use
of endobronchial one-way valves reveals questions on etiology of
spontaneous pneumothorax: report of three cases. J Cardiothorasc Surg
2009;4:63. Crossref
12. Schiavon M, Marulli G, Zuin A, et al.
Endobronchial valve for secondary pneumothorax in a severe emphysema
patient. Thorac Cardiovasc Surg 2011;59:509-10. Crossref
13. El-Sameed Y, Waness A, Al Shamsi I,
Mehta AC. Endobronchial valves in the management of broncho-pleural and
alveolo-pleural fistulae. Lung 2012;190:347-51. Crossref
14. Ambrosino N, Ribechini A, Allidi F,
Gabbrielli L. Use of endobronchial valves in persistent air leaks: a case
report and review of the literature. Expert Rev Respir Med 2013;7:85-90. Crossref
15. Travaline JM, McKenna RJ Jr, De
Giacomo T, et al. Treatment of persistent pulmonary air leaks using
endobronchial valves. Chest 2009;136:355-60. Crossref
16. Gillespie CT, Sterman DH, Cerfolio RJ,
et al. Endobronchial valve treatment for prolonged air leaks of the lung:
a case series. Ann Thorac Surg 2011;91:270-3. Crossref
17. Mahajan AK, Verhoef P, Patel SB, Carr
G, Kyle Hogarth D. Intrabronchial valves: a case series describing a
minimally invasive approach to bronchopleural fistulas in medical
intensive care unit patients. J Bronchol Intervent Pulmonol
2012;19:137-41. Crossref
18. Firlinger I, Stubenberger E, Müller
MR, Burghuber OC, Valipour A. Endoscopic one-way valve implantation in
patients with prolonged air leak and the use of digital air leak
monitoring. Ann Thorac Surg 2013;95:1243-9. Crossref
19. Dooms CA, Decaluwe H, Yserbyt J, De
Leyn P, Van Raemdonck D, Ninane V. Bronchial valve treatment for pulmonary
air leak after anatomical lung resection for cancer. Eur Respir J
2014;43:1142-8. Crossref
20. Cordovilla R, Torracchi AM, Novoa N,
et al. Endobronchial valves in the treatment of persistent air leak, an
alternative to surgery [in English, Spanish]. Arch Bronconeumol
2015;51:10-5. Crossref
21. Reed MF, Gilbert CR, Taylor MD, Toth
JW. Endobronchial valves for challenging air leaks. Ann Thorac Surg
2015;100:1181-6. Crossref
22. Hance JM, Martin JT, Mullett TW.
Endobronchial valves in the treatment of persistent airleaks. Ann Thorac
Surg 2015;100:1780-6. Crossref
23. Gilbert CR, Casal RF, Lee HJ, et al.
Use of one-way intrabronchial valves in air leak management after tube
thoracostomy drainage. Ann Thorac Surg 2016;101:1891-6. Crossref
24. Miller MR, Hankinson J, Bursasco V, et
al. Standardisation of spirometry. Eur Respir J 2005;26:319-38. Crossref
25. Ip MS, Ko FW, Lau AC, et al. Updated
spirometric reference values for adult Chinese in Hong Kong and
implications on clinical utilization. Chest 2006;129:384-92. Crossref
26. Sciurba FC, Ernst A, Herth FJ, et al.
A randomized study of endobronchial valves for advanced emphysema. N Engl
J Med 2010;363:1233-44. Crossref
27. von Elm E, Altman DG, Egger M, Pocock
SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening
the Reporting of Observational Studies in Epidemiology (STROBE) statement:
guidelines for reporting observational studies. J Clin Epidemiol
2008;61:344-9. Crossref
28. Koster TD, van Rikxoort EM, Huebner
RH, et al. Predicting lung volume reduction after endobronchial valve
therapy is maximized using a combination of diagnostic tools. Respiration
2016;92:150-7. Crossref
29. Schuhmann M, Raffy P, Yin Y, et al.
Computed tomography predictors of response to endobronchial valve lung
reduction treatment. Comparison with Chartis. Am J Respir Crit Care Med
2015;191:767-74. Crossref