© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REMINISCENCE: ARTEFACTS FROM THE HONG KONG MUSEUM OF
MEDICAL SCIENCES
Vaccination knife
Moira Chan-Yeung, FRCP, FRCPC
Member of the Education and Research Committee, Hong Kong
Museum of Medical Sciences Society
Smallpox is a highly infectious disease that is
spread by droplets via contact with an infected individual or by direct
contact with infected bodily fluids or contaminated objects. The onset of
smallpox is acute with a fever that can increase to or exceed 38.3°C
followed by the appearance of a rash. The rash is characterised by firm,
deep-seated vesicles or pustules at the same stage of development. Case
fatality can be as high as 50%.
Smallpox is an ancient disease, first documented in
medical writings from ancient India as early as 1500 BC. The disease was
carried to China during the first century AD. By the mid-18th century,
smallpox had spread worldwide and a major cause of death in affected
countries.1
The disease is caused by the variola virus,
belonging to the family of orthopoxvirus. There are four orthopoxviruses:
variola, vaccinia, cowpox, and monkeypox. Variola virus infects only
humans, while the other three orthopoxviruses can infect both humans and
animals.2 Long before the discovery
of the virus, it was recognised that a person who contracted one form of
the virus became immune against all other forms, which is the basic
principle of variolation and vaccination.
Variolation against smallpox was introduced in
China in the late 10th century. Several methods of inoculation were used
including blowing powdered smallpox scabs or placing a pledget of cotton
impregnated with smallpox scabs into the nose of a child, or wearing the
unwashed undergarment of a child with smallpox for 2 to 3 days.
Nonetheless severe reactions sometimes occurred with variolation.3
In 1718, Lady Mary Wortley Montagu, who observed
variolation during her stay in the Ottoman Empire, became an enthusiastic
proponent on her return to England. As a result, variolation became widely
practised in England, Europe, and the North America. In 1796, Edward
Jenner, a doctor in Gloucestershire, England, first used the material from
a cowpox lesion, which he called ‘vaccine’, for inoculation to produce
immunity to smallpox in humans. Vaccination, which produced effective
immunity but only caused a mild reaction, was much safer than variolation
and soon replaced the latter.1
Jennerian vaccination was introduced in China in
1805 via Macao and Guangzhou by Alexander Pearson, a surgeon to the East
India Company.3 He wrote a pamphlet
on the technique of vaccination, which was translated into Chinese, and he
also trained several Chinese employees of the British factory. One of his
first trainees, Qiu Xi (邱熺), became wealthy as a vaccinator and passed on
the technique to his children and grandchildren making it a family
business.3
Qiu Xi published his own book in 1817. He described
the method of Pearson using the language of acupuncture, naming the
meridian points on the arm where incisions were to be made and explaining
the pustules as “fetal toxin” being liberated. He even provided aftercare
using traditional Chinese medicine.3
Qiu performed vaccination by making an incision and introducing a foreign
substance into the body, thus breaking the rules of Chinese traditional
medicinal practice. Despite this, vaccination became widely accepted in
Southern China in the early 19th century as a result of his efforts and
those of other early vaccinators.
Lymph supply throughout the year in those days was
ensured by the “charitable vaccination dispensary”, where poor children
were vaccinated and the lymph extracted from the resultant lesions was
directly applied on the child to be vaccinated. Because of the possibility
of transmitting diseases such as leprosy by this arm-to-arm transmission
method, vaccinators improvised ways to produce lymph including inoculation
of young buffaloes through the nostrils with powdered human smallpox
scabs.3
When Hong Kong became a British colony in 1842,
traditional variolation was extensively performed.4 Although Benjamin Hobson, a missionary doctor, was the
first to vaccinate Chinese children at the Medical Missionary Society
Hospital on Morrison Hill,5 it was
only after the founding of Tung Wah Hospital in 1872 that employed Chinese
vaccinators that vaccination became accepted by the local community. Dr
PBC Ayers, Colonial Surgeon (1873-1897), praised Tung Wah Hospital for its
efforts in vaccination. Although he vaccinated the European community and
patients under his care, he did not have a programme for the Chinese
community because of the extensive vaccination work carried out by Tung
Wah.6
Pearson practised the single linear cut/scratch
method using a lancet as illustrated in the Figure. He made only one
incision in one arm. Qiu modified his method by making two incisions on
both arms along the meridian of acupuncture points. The vaccine was
introduced onto the incisions using ivory points shaped like a lancet
blade.3 To prevent secondary
infection, rigid guards, shields, or cages were placed over the
vaccination sites to allow natural healing. It is likely that the
vaccinators of Tung Wah Hospital used Qiu’s method as they were trained in
South China by Qiu’s descendants or by trainees of the early vaccinators
taught by Pearson.
Other more complicated instruments were designed
such as a spear-pointed lancet with a groove for holding the vaccine, or
spring-loaded lancet. These gave way to simpler, easily sterilised and/or
dispensable instruments such as surgical needles or even darning needles
used with special handles. The incision method was widely used as it was
simple and rapid, and could be used for multiple site inoculation.4
Another method of vaccination was by puncture, a
stabbing action at a right angle or acute angle to the site. A variety of
mechanical, spring-loaded devices that could control the depth of
penetration were developed but they were difficult to clean. In 1961, a
bifurcated needle was introduced; it was simple and could be used by
auxiliary workers after minimum training. This method saved 75% of the
volume of the vaccine and was widely used in the Eradication Programme
against Smallpox of the World Health Organization in the 1960s and 70s.7
The third was the multiple pressure method,
performed with the flat of an instrument such as the flat of a blade or a
Hagedorn needle, that was flattened on the sides and firm pressure was
applied to the skin of the upper forearm where a drop of vaccine was
placed. The pressure tore the stratum corneum slightly and the inoculum
was deposited in the epidermis.7
Hong Kong ran many major vaccination campaigns
during the early 20th century in an attempt to reduce the severity and
mortality from smallpox epidemics. The Vaccine Institute (1892-1906) and
the Bacteriology Institute, built in 1906, produced smallpox vaccine lymph
for use locally and in neighbouring areas such as Guangzhou. The massive
vaccination campaigns involved not only Tung Wah Hospital but all other
hospitals and Chinese public dispensaries.8
Vaccination campaigns continued after the Second World War. During the
post-war years, the government hired inoculators trained in China to carry
out smallpox vaccination and other immunisation in the field. According to
Patricia Ko-Woo, Chief Nursing Officer at the Department of Health in the
1950s and 1960s, the most common method employed then was to produce two
to three abrasions on the skin of the upper arm, or upper thigh and
occasionally on the sole of the foot, using a small blade similar to a
later version of one shown in the Figure. Only one site was inoculated at
one time. Later on, needles were used to produce five to six pricks on the
skin. In both methods, the drawing of blood was to be avoided.
Revaccination was recommended every 2 to 3 years.
The last case of smallpox in Hong Kong was recorded
in 1952 and Hong Kong was declared free of smallpox in 1979.9 In 1967, the World Health Organization set in motion a
global Smallpox Eradication Programme using intensive vaccination,
surveillance, contact tracing, and isolation/quarantine. The Programme
succeeded and the last naturally occurring case of smallpox was reported
on 26 October 1977. On 8 May 1980, the World Health Assembly announced
that the world was free of smallpox and recommended that all countries
cease vaccination.9
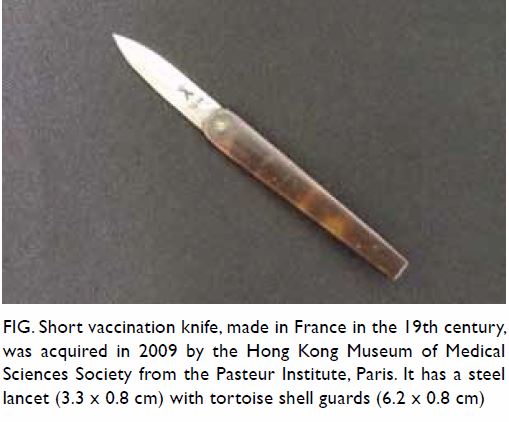
Figure. Short vaccination knife, made in France in the 19th century, was acquired in 2009 by the Hong Kong Museum of Medical Sciences Society from the Pasteur Institute, Paris. It has a steel lancet (3.3 x 0.8 cm) with tortoise shell guards (6.2 x 0.8 cm)
References
1. Riedel, S. Edward Jenner and the history
of smallpox and vaccination. Proc (Bayl Univ Med Cent) 2005;18:21-5.
2. Rao AR. Smallpox. Bombay: Kothari Book
Depot. 1972. OCLC 723806.
3. Leung AK. The business of vaccination in
nineteenth-century Canton. Late Imperial China 2008;29:7-39. Crossref
4. Hobson B. Report of the Medical
Missionary Society’s Hospital at Hong Kong under the care of Benjamin
Hobson. Chinese Repository 1844: 380.
5. Bowman ML. James Legge and the Chinese
classics: a brilliant Scot in the turmoil of colonial Hong Kong. 1st ed.
Victoria, BC, Canada: Friesen Press; 2016: 159.
6. Colonial Surgeon’s Report of 1876, Tung
Wah Hospital. Hong Kong Blue Book 1876.
7. Baxby D. Smallpox vaccination
techniques: from knives and forks to needles and pins. Vaccine
2002;20:2140-9. Crossref
8. Medical and Sanitary Report 1917. Tung
Wah Smallpox Hospital. Hong Kong Administrative Reports 1917: 48.
9. Lee SH. Infectious disease surveillance.
Hong Kong: Department of Health; 1994: 43-5.

