DOI: 10.12809/hkmj166321
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Portomesenteric vein thrombosis following
laparoscopic sleeve gastrectomy in a
Chinese patient
KM Kwok, FHKCP, FHKAM (Medicine)1; KL Lee, FHKCP, FHKAM (Medicine)1; YS Poon, FHKCP, FHKAM (Medicine)1; SY Lam, FHKCP, FHKAM (Medicine)1; T Liong, FHKCP, FHKAM (Medicine)1; HM Wong, MBChB, MRCP1; NK Chiu, MBChB, FHKAM (Surgery)2; KI Law, FHKCP, FHKAM (Medicine)1
1 Department of Intensive Care, United Christian Hospital, Kwun Tong, Hong Kong
2 Department of Surgery, United Christian Hospital, Kwun Tong, Hong Kong
Corresponding author: Dr KM Kwok (lawki@ha.org.hk)
Case Report
A 51-year-old morbidly obese Chinese man was
scheduled for laparoscopic sleeve gastrectomy in
October 2016. He had a body mass index of 34 kg/m2
complicated by metabolic syndrome. He had no
history of thromboembolism. Surgery was performed
using a 5-port technique. A liver retractor was
inserted under direct vision. The greater curvature
was mobilised up to the angle of His and the gastric
sleeve was created. The operation lasted 125 minutes.
The patient was mobile on postoperative day 2 and
was discharged on day 5.
On day 6 postoperatively, he presented to
the surgical ward with nausea, vomiting, and
epigastric pain. No peritoneal signs were elicited
during physical examination. White cell count had
increased to 10.1 x 109/L (reference range, 4-11 x
109/L), and serum creatinine level to 248 µmol/L
(reference range, 67-109 µmol/L). He was kept nil by
mouth and prescribed broad-spectrum antibiotics.
A computed tomographic (CT) scan of the abdomen
and pelvis with intravenous contrast was performed
on postoperative day 8. The portal vein was not
opacified and a wedge-shaped hypoenhancing
area was seen at subcapsular S4 of the liver. These
were attributed by the radiologist to the timing of
acquisition and perfusion artefacts. Ascites was also
identified on the CT scan.
His condition deteriorated and he was
transferred to the intensive care unit on postoperative
day 9. A repeat contrast-enhanced CT on the same
day, arranged in view of his rapid deterioration
and the presence of unexplained ascites, revealed
extensive thrombosis of the superior mesenteric
vein, splenic vein, portal trunk, and portal veins
(Fig). A long segment of small bowel appeared
ischaemic. Hypoenhancement in the liver and spleen
was evident and likely related to impaired perfusion.
Emergent laparotomy was performed immediately
and revealed small bowel gangrene extending from
the proximal jejunum to mid-ileum with mesenteric
vein thrombosis. The distal ileum showed venous
congestion. The surgical team attempted to perform
clot retrieval by insertion of a Fogarty catheter to
the ileal branch of the mesenteric vein but was
unsuccessful due to the extensive thrombosis.
A gangrenous segment of small bowel was then
resected. The operation took 5 hours; the patient
remained anuric and required escalating pressor
support intra-operatively.
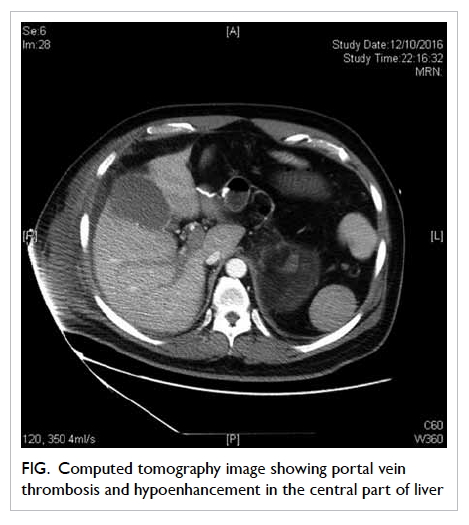
Figure. Computed tomography image showing portal vein thrombosis and hypoenhancement in the central part of liver
He was kept intubated and transferred back to
the intensive care unit postoperatively. He had severe
metabolic acidosis with arterial blood gas pH of
7.16 (reference range, 7.35-7.45). He required renal
support by continuous venovenous haemofiltration
from postoperative day 1 to 3. Renal function later
recovered and no further renal replacement therapy
was needed. The patient was weaned off vasopressors
on day 4 and was extubated on day 6.
Due to the presence of coagulopathy,
anticoagulation was not prescribed immediately
postoperatively. Intravenous unfractionated heparin
was introduced on postoperative day 3 with close
monitoring of activated partial thromboplastin time.
The infusion was withheld on day 6 as the patient
passed malaena. Oesophagogastroduodenoscopy
and colonoscopy did not reveal any sites of bleeding.
Heparin infusion was then resumed and on day 8
changed to subcutaneous low-molecular-weight
heparin.
The patient was discharged from the intensive
care unit on postoperative day 12. Closure of the
ileostomy was performed in January 2017. Oral
anticoagulation was prescribed for at least 6 months
and follow-up CT scan was arranged to monitor the
progress of portomesenteric vein thrombosis (PMVT).
Discussion
Portomesenteric vein thrombosis is an infrequent
but potentially life-threatening complication
following laparoscopic bariatric surgery. To the
best of our knowledge, this is the first case report
of PMVT as a complication of laparoscopic bariatric
surgery in the Chinese population. Previous
retrospective studies have reported an incidence of
0.3% to 1%,1 2 3 although this was likely underestimated
due to the presence of asymptomatic cases. Most
patients run an indolent course and do not require
any surgical intervention. Nonetheless some cases
may be fulminant as in our patient with mesenteric
ischaemia and infarction.1 2 3 4 5
The initial manifestation of PMVT can be
subtle so early diagnosis requires a high index of
suspicion. Patients usually present 7 to 14 days
postoperatively with nausea, vomiting, abdominal
pain, and fever.1 4 5 Physical examination is mostly
unrevealing. Apart from leukocytosis and mild
elevation of liver enzymes, most laboratory tests are
normal. Only when it is associated with mesenteric
ischaemia do patients present with peritonitis and
septic shock. Initially, our patient presented typically
with non-specific gastrointestinal upset but then
deteriorated rapidly once bowel ischaemia occurred.
Various mechanisms of PMVT following
laparoscopic bariatric surgery have been proposed.
The use of a reverse Trendelenburg position and
carbon dioxide pneumoperitoneum may cause a
decrease in portal blood flow leading to stasis.1 4 5
The change in blood flow due to ligation of the
short gastric vessels may promote the occurrence of
PMVT.1 2 Direct contact with the splenic vein during
surgery may result in intimal damage and subsequent
thrombosis.1 2 4 The use of a liver retractor can lead to
blood stasis within the liver; retrograde thrombosis
may occur.2 Finally, patients may have difficulty
in maintaining adequate fluid intake following
bariatric surgery. Dehydration will increase the risk
of thrombotic complications.1 2
Contrast-enhanced CT scan is used to
diagnose PMVT with a sensitivity of 90%.2 Ascites
is present in approximately one third of patients
with PMVT.4 The presence of unexplained ascites
following laparoscopic bariatric surgery should not
be overlooked.
Treatment of PMVT depends on its severity.
Therapeutic anticoagulation is recommended in
patients without mesenteric ischaemia with an aim to
recanalise the portomesenteric veins.6 Nonetheless
the optimal duration of anticoagulation is not well
defined. Gandhi et al7 suggested 3 to 6 months of
anticoagulation, and extended further if signs and
symptoms persist. Other studies have recommended
longer treatment, ranging from 6 to 12 months.4 8
In cases with underlying thrombophilia, lifelong
anticoagulation is required. Prompt anticoagulation
can reduce the future risk of extrahepatic portal
hypertension with the associated complications
such as variceal gastrointestinal bleeding.2 In severe
cases of PMVT complicated with bowel ischaemia,
immediate exploration and bowel resection is
mandated. Direct portomesenteric thrombectomy
or thrombolysis is possible in selected cases.1
References
1. Goitein D, Matter I, Raziel A, et al. Portomesenteric
thrombosis following laparoscopic bariatric surgery:
incidence, patterns of clinical presentation, and etiology in
a bariatric patient population. JAMA Surg 2013;148:340-6. Crossref
2. Villagrán R, Smith G, Rodriguez W, et al. Portomesenteric
vein thrombosis after laparoscopic sleeve gastrectomy:
incidence, analysis and follow-up in 1236 consecutive
cases. Obes Surg 2016;26:2555-61. Crossref
3. Salinas J, Barros D, Salgado N, et al. Portomesenteric vein
thrombosis after laparoscopic sleeve gastrectomy. Surg
Endosc 2014;28:1083-9. Crossref
4. Rosenberg JM, Tedesco M, Yao DC, Eisenberg D. Portal
vein thrombosis following laparoscopic sleeve gastrectomy
for morbid obesity. JSLS 2012;16:639-43. Crossref
5. Muneer M, Abdelrahman H, El-Menyar A, et al.
Portomesenteric vein thrombosis after laparoscopic sleeve
gastrectomy: 3 case reports and a literature review. Am J
Case Rep 2016;17:241-7. Crossref
6. Condat B, Pessione F, Hillaire S, et al. Current outcome
of portal vein thrombosis in adults: risk and benefit of
anticoagulant therapy. Gastroenterology 2001;120:490-7. Crossref
7. Gandhi K, Singh P, Sharma M, Desai H, Nelson J, Kaul
A. Mesenteric vein thrombosis after laparoscopic gastric
sleeve procedure. J Thromb Thrombolysis 2010;30:179-83. Crossref
8. Kumar S, Sarr MG, Kamath PS. Mesenteric venous
thrombosis. N Engl J Med 2001;345:1683-8. Crossref

