Hong Kong Med J 2017 Apr;23(2):207.e3–4
DOI: 10.12809/hkmj164956
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Urothelial carcinoma with paraneoplastic leukocytosis
CW Hsu, MD, PhD;
HY Su, MD
Department of Emergency Medicine, E-Da Hospital and I-Shou University,
Kaohsiung, Taiwan
Previously presented at the 8th Asian Conference on Emergency
Medicine, Taiwan, 7-10 November 2015.
Corresponding author: Dr HY Su (hys927@hotmail.com)
An 88-year-old male with no underlying disease
presented to our emergency department in
March 2015 with a 2-week history of right flank
pain but no fever or urinary tract symptoms.
He was conscious, alert, and well-oriented. His
blood pressure was 145/89 mm Hg, with a heart
rate of 82 beats/min and respiratory rate of 16
breaths/min on arrival. Physical examination
revealed obvious right flank knocking tenderness.
Laboratory testing revealed white blood cell (WBC)
count of 34.7 x 109 /L (reference range [RR], 4.5-11.0 x 109 /L), haemoglobin level of 95 g/L (RR,
135-175 g/L), platelet count of 496 x 109 /L (RR, 150-450 x 109 /L), C-reactive protein level of
24.3 mg/L (RR, 0-10 mg/L), and serum
calcium level of 3.31 mmol/L (RR, 2.18-2.58 mmol/L). Urinalysis demonstrated no pyuria,
but 50 to 75 red blood cells per high-power field.
Prothrombin time, activated partial thromboplastin
time, and fibrinogen were within normal limits.
An abdominal plain film revealed a mass lesion
with a concealing right lower psoas shadow (Fig 1). Subsequent abdominal computed tomographic (CT) scan demonstrated a cyst-like lesion with
irregular surface, involving adjacent tissues in the
retroperitoneal cavity (Fig 2).

Figure 1. A plain abdominal film revealing a mass lesion (arrows) with obliteration of right lower psoas shadow (arrowheads)
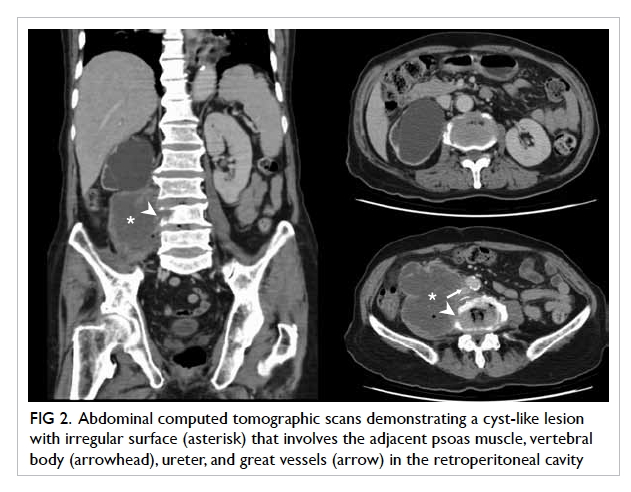
Figure 2. Abdominal computed tomographic scans demonstrating a cyst-like lesion with irregular surface (asterisk) that involves the adjacent psoas muscle, vertebral body (arrowhead), ureter, and great vessels (arrow) in the retroperitoneal cavity
A CT-guided biopsy was performed because
the discrepancy between clinical presentation and
laboratory tests and image study made it difficult
for physicians to discriminate psoas muscle
abscess from malignancy. Ultimate pathology of
biopsy specimens revealed a high-grade urothelial
carcinoma with tumour necrosis. The TNM staging
was stage IV (cT4N0M0). Blood and urine cultures
were all negative. Follow-up 1 month later revealed a
WBC count of 34.7 x 109 /L.
Urothelial carcinoma originates in the urinary
system. Paraneoplastic leukocytosis, defined by
a WBC count of >20.0 x 109 /L on more than two
occasions 30 days apart, occurs in 0.6% of urothelial
carcinoma cases.1 The aetiology of paraneoplastic
leukocytosis is considered to be related to the
production of granulocyte colony-stimulating factor
by tumour cells.2 3 Hypercalcaemia, anaemia and thrombocytosis, as seen in this case, are also frequently
seen in paraneoplastic syndrome. It is associated
with advanced urothelial cancer and indicates a poor
prognosis.1 3 Muscle invasion is also frequently found in cases of urothelial cancer with paraneoplastic
leukocytosis.1 The cyst-like pattern of urothelial
cancer on abdominal CT scan in combination with the
paraneoplastic leukocytosis can mislead physicians
into making an incorrect diagnosis, such as pyogenic
psoas muscle abscess. We advise physicians to always
be aware of urothelial cancer with paraneoplastic
leukocytosis while managing a cyst-like lesion in the
retroperitoneal cavity.
References
1. Izard JP, Gore JL, Mostaghel EA, Wright JL, Yu EY.
Persistent, unexplained leukocytosis is a paraneoplastic
syndrome associated with a poor prognosis in patients
with urothelial carcinoma. Clin Genitourin Cancer
2015;13:e253-8. Crossref
2. Ito N, Matsuda T, Kakehi Y, Takeuchi E, Takahashi T,
Yoshida O. Bladder cancer producing granulocyte colony-stimulating
factor. N Engl J Med 1990;323:1709-10. Crossref
3. Kumar AK, Satyan MT, Holzbeierlein J, Mirza M, Van
Veldhuizen P. Leukemoid reaction and autocrine growth
of bladder cancer induced by paraneoplastic production
of granulocyte colony-stimulating factor—a potential
neoplastic marker: a case report and review of the
literature. J Med Case Rep 2014;8:147. Crossref

