Hong Kong Med J 2017 Apr;23(2):207.e1–2
DOI: 10.12809/hkmj164938
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Extraluminal location of a Foley catheter balloon
CL Cho, FRCS Ed (Urol), FHKAM (Surgery);
Wayne KW Chan, FRCS Ed (Urol), FHKAM (Surgery);
Ringo WH Chu, FRCS Ed (Urol), FHKAM (Surgery);
IC Law, FRCS Ed (Urol), FHKAM (Surgery)
Division of Urology, Department of Surgery, Kwong Wah Hospital,
Yaumatei, Hong Kong
Corresponding author: Dr CL Cho (chochaklam@yahoo.com.hk, ccl296@ha.org.hk)
Indwelling urinary catheters are generally safe but
may be associated with complications. Although
intraperitoneal or extraperitoneal perforation
is rare, the condition can be life-threatening.1
Abdominopelvic computed tomography (CT) is
commonly performed in hospitalised patients. In
many cases the urinary bladder is catheterised and
included in the scan; CT scan is a reliable method to
evaluate many pathologies of the urinary bladder.2
The apparent extraluminal position of a Foley
catheter tip or balloon can be misleading, however.3
We present a case in which a Foley catheter balloon
was inflated in a bladder diverticulum mimicking an
extraluminal location on a CT scan.
Case
A 68-year-old man was admitted with abdominal
distension and suprapubic pain in April 2016. He was
a visitor to Hong Kong and had a history of recurrent
acute urinary retention. A urethral Foley catheter
had been inserted in his home country a week before
presentation and he travelled to Hong Kong with
the catheter in situ. A urological assessment was
scheduled on his return home. He had a history of
open left nephrectomy performed over 20 years ago
for urinary stone disease but otherwise had good
medical history.
On presentation he was afebrile and
normotensive. The abdomen was grossly distended
with suprapubic tenderness and a general surgeon
was consulted. Digital rectal examination revealed a
grossly enlarged non-suspicious prostate. Clear urine
and good urine outputs from the Foley catheter were
noted. Laboratory tests showed an elevated white blood
cell count of 14.5 x 109 /L and normal creatinine level
of 125 µmol/L. A nasogastric tube was inserted with a
working diagnosis of intestinal obstruction. An urgent
contrast CT scan revealed grossly dilated small bowel
loops with free fluid in the pelvis and paracolic gutters.
The wall of the urinary bladder was thickened with
a large prostate and intravesical prostatic protrusion
(Fig 1). The tip of the Foley catheter appeared to be at
an extravesical location (Fig 2).
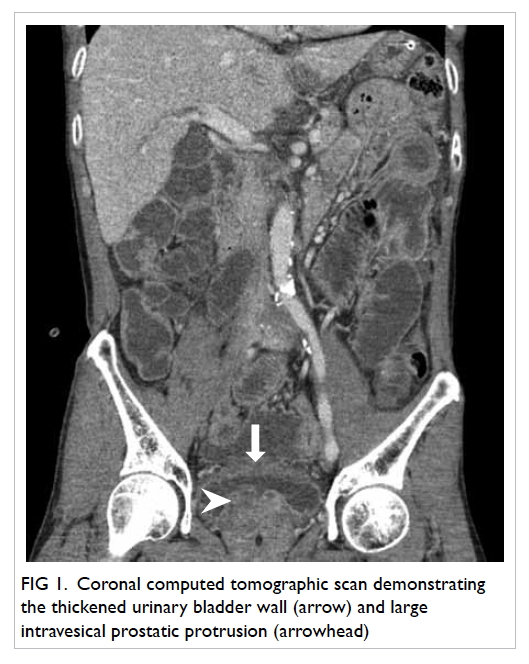
Figure 1. Coronal computed tomographic scan demonstrating the thickened urinary bladder wall (arrow) and large intravesical prostatic protrusion (arrowhead)

Figure 2. Axial computed tomographic scan of the pelvis demonstrating (a) the Foley catheter through the thickened urinary bladder wall (arrow) and extraluminal location of balloon (arrowhead); and (b) the extraluminal location of balloon and Foley catheter tip (arrowhead)
A urological opinion was sought and the
patient underwent exploratory laparotomy. Intra-operatively,
the tip of the Foley catheter and balloon
were noted inside a large 5-cm bladder diverticulum
at the dome of the urinary bladder. There was a 5-mm
concealed perforation at the bladder diverticulum
with surrounding dusky tissue covered by slough.
Bladder diverticulectomy was performed. The
urinary bladder was closed in a two-layer fashion and
confirmed water-tight. No bowel injury was evident
and an extensive washout was performed. A pelvic
drain and 18F Foley catheter were inserted.
Postoperatively, the patient progressed well.
Diet was resumed on postoperative day 3 and
the drain was removed. There were no wound
complications and the patient was fit for discharge
on day 5. He returned to his home country with the
Foley catheter in situ. We advised maintenance of
bladder drainage until surgery for benign prostate
hyperplasia could be performed.
This case concurs with a previous report that
extraluminal location of a Foley catheter balloon on
imaging can be misleading.3 Exploratory laparotomy
based on the radiological findings alone may not be
appropriate, especially when the clinical suspicion of
bladder perforation is low. Further studies including
cystogram should be considered in case of doubt.
References
1. White SA, Thompson MM, Boyle JR, Bell PR.
Extraperitoneal bladder perforation caused by an
indwelling urinary catheter. Br J Surg 1994;81:1212. Crossref
2. Caoili EM, Cohan RH, Korobkin M, et al. Urinary tract
abnormalities: initial experience with multi-detector row
CT urography. Radiology 2002;222:353-60. Crossref
3. Abadi S, Brook OR, Solomonov E, Fischer D. Misleading
positioning of a Foley catheter balloon. Br J Radiol
2006;79:175-6. Crossref

