Hong Kong Med J 2016 Jun;22(3):231–6 | Epub 11 Apr 2016
DOI: 10.12809/hkmj154672
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Acceptability of the combined oral contraceptive pill among Hong Kong women
Sue ST Lo, MD, FRCOG;
Susan YS Fan, MB, BS, MRCOG
The Family Planning Association of Hong Kong, 10/F, 130 Hennessy Road, Wanchai, Hong Kong
Corresponding author: Dr Sue ST Lo (stlo@famplan.org.hk)
Abstract
Objective: To evaluate the motivators and barriers
to the use of the combined oral contraceptive pill
among Hong Kong women.
Methods: The Family Planning Association of Hong
Kong commissioned the ESDlife to launch an online
survey and invited its female members aged 18 to
45 years who had used contraceptives in the past
12 months to participate in this survey. The online
survey was posted on the ESDlife website between
April 2015 and May 2015. Measurements included
contraceptive choice, and motivators and barriers to
the use of a combined oral contraceptive pill.
Results: A total of 1295 eligible women with a
median age of 32 years participated in this survey.
In the past 12 months, 76.1% of them used a male
condom, 20.9% practised coitus interruptus, 16.2%
avoided coitus during the unsafe period, and 12.6%
took a combined oral contraceptive pill. These
women chose a combined oral contraceptive for
convenience, effectiveness, and menstrual regulation, though 60.9% had stopped the pills because they were
worried about side-effects, experienced side-effects,
or consistently forgot to take the pills. Some women
had never tried a combined oral contraceptive pill
because they feared side-effects, they were satisfied
with their current contraceptive method, or pill-taking
was inconvenient.
Conclusions: The combined oral contraceptive pill is
underutilised by Hong Kong women compared with
those in many western countries. A considerable
proportion of respondents expressed concern about
actual or anticipated side-effects. This suggests that
there remains a great need for doctors to dispel the
underlying myths and misconceptions about the
combined oral contraceptive pill.
New knowledge added by this study
- Some women chose a combined oral contraceptive (COC) pill for convenience, effectiveness, and menstrual regulation.
- Some women had never tried a COC pill because they feared its side-effects, were satisfied with their current contraceptive method, or pill-taking was inconvenient.
- Some women stopped taking their COC pill because they feared its side-effects, experienced side-effects, or consistently forgot to take pills.
- During contraceptive counselling, doctors should educate women and dispel the myths and misconceptions about COC pills.
- Doctors should explain the side-effects of the COC pill, its absolute risk, and the underlying health conditions that might increase the risk of complications as well as the non-contraceptive benefits of COC thoroughly so that women can make an informed decision and use it safely.
- To help women stay on the pill, doctors should inform women that different pills have slightly different side-effect profiles and they can switch to another formulation if they experience any problem with their current COC. Improving accessibility by allowing walk-in consultations for problems with the COC pill gives women additional support.
Introduction
According to the Family Planning Knowledge, Attitude and Practice in Hong Kong Survey 2012 among
Hong Kong couples,1 the male condom was the most
popular contraceptive. The proportion of couples
who used a male condom doubled from 32.2% in
1987 to 69.6% in 2012. Combined oral contraceptive
(COC) pill was the second most common form of
contraception, though the proportion of women
using a COC pill declined from 20.3% in 1987 to
10.8% in 2012. The failure rate of the male condom
when used correctly is 6 times higher than that for the
COC pill.2 Although the low-dose COC pill has a low
incidence of complications, high efficacy, and many
non-contraceptive benefits, relatively few women use
it in Hong Kong. The report of the United Nations
world contraceptive patterns 2013 estimated that
the prevalence of pill use in Hong Kong women aged
15 to 49 years was 6.7%, which is much lower than
other countries with similar development, wealth,
and culture such as Australia (30.0%), Canada
(21.0%), Singapore (10.0%), the UK (28.0%), and the US (16.3%).3 Unlike these countries, the COC pill is not a prescription drug in
Hong Kong. Women can buy a low-dose COC pill
that contains either 30-µg or 20-µg ethinylestradiol
and one of the progestogens: levonorgestrel,
gestodene, desogestrel, or drospirenone at any of the
large-chain personal health and beauty retailers or
pharmacy stores. All pills have similar efficacy. Their
failure rate is 0.3% within the first year of perfect
use.2 Low-dose pills are safer, better tolerated, and
have equal or higher efficacy than high-dose pills
that contain 50-µg ethinylestradiol.
With 70% of couples in Hong Kong using the
male condom,1 the demand for abortion due to failed
contraception cannot be ignored. It was shown that
77.4% of women who underwent an abortion were
using contraception during the index pregnancy
and 51.2% of them were using a male condom.1 The
number of legal abortions in Hong Kong has reduced
from 25 363 in 1995 to 10 359 in 2014 (personal
communication, Department of Health), though
the number of abortions carried out across the border
is unknown. According to the results from the serial
5-yearly territory-wide family planning survey,1 the
proportion of married women who went to China for
their last abortion increased from 24.3% in 1992 to
47.2% in 2012. Given the limited resources assigned
to abortion in public hospitals, women have to resort
to the more expensive legal abortion service in
private hospitals or the Family Planning Association
of Hong Kong (FPAHK). The FPAHK performs 3000
medical and surgical first-trimester abortions each
year and has reached its full service capacity. There
is a need to further reduce unplanned pregnancies
and abortion in Hong Kong. One plausible solution
is to encourage more women to use more effective
contraception such as the combined hormonal
contraceptive pill, progestogen-only contraceptives,
intrauterine contraceptive device, or sterilisation.
The failure rate of these effective contraceptives
when used correctly is <1% in the first year of use.2
Studies have shown that identifying women’s
perspective can help doctors understand their motive
to choose one contraceptive over another.4 One study
identified personal choices, local factors, women’s
perceived safety, effectiveness, and convenience of
the method as determinants of contraceptive choice.5
Among the effective contraceptives available in
Hong Kong, the COC pill is the most accepted. We
performed this survey to determine the motivators
and barriers to COC pill use.
Methods
The Family Planning Association of Hong Kong
invited ESDlife to host the survey that was open to
its female members aged between 18 and 45 years.
The questionnaire was designed by the investigators.
ESDlife is an online lifestyle media in Hong Kong.
It is a joint venture between the Hong Kong SAR
Government and a commercial firm that began in
2000 with the aim of providing e-government and
e-commerce services. With the establishment of the
Government’s own website in 2008, all government
services have migrated to the official website and
ESDlife remains a solely commercial portal. As of
2 January 2015, it had 297 152 members of whom
64.4% were female. Among the female members,
89.0% were within our target age range: 32.3% were
30-34 years old, 23.3% were 35-39 years old, 19.3%
were 25-29 years old, 10.3% were 40-45 years old,
and 3.8% were 18-24 years old.
ESDlife sent out 100 000 invitations
randomly to its female members aged between 18
and 45 years on 21 April 2015 and invited them to
participate in this online survey between 21 April
2015 and 20 May 2015. There were 16 questions that
explored the basic demographic characteristics of
respondents (6), their contraceptive choice (3), and
their motivators and barriers to COC use (7). Invited
members entered the survey via a link and those who
had not used any contraception in the previous 12
months were screened out by the first question. Only
eligible subjects could proceed with the survey. They
could stop at any question and the questionnaire
would be voided. To encourage participation, a
$50 supermarket coupon was given to every 10th
respondent via ESDlife. This study was reviewed and
approved by the Health Services Subcommittee and
Ethics Panel of the FPAHK.
Data analyses were accomplished using the
Statistical Package for the Social Sciences (Windows
version 22.0; SPSS Inc, Chicago [IL], US). Descriptive
statistics were presented. Bivariate Chi squared
test was performed to analyse the demographic
characteristics that predicted COC pill use.
Results
During the survey period, only completed
questionnaires were captured by the system so the
number of incomplete questionnaires was unknown.
A total of 1566 women completed the survey
within the 1-month period, 271 were screened out
by Question 1 because they had not used regular
contraception in the past 12 months and 1295
questionnaires were analysed. The response rate was
1.57%. The median age of the respondents was 32
years (interquartile range, 29-36 years). Half of them
(50.7%) had a university education, 20.5% had a post-secondary
education (diploma or associate degree),
and 28.3% had a secondary education. The majority
(65.5%) were married, 29.0% were unmarried,
3.3% were cohabiting, 2.1% had separated or
divorced, and 0.2% were widowed. Over half of the
respondents were nulliparous (56.7%) and had no
plan for pregnancy (52.3%). They usually purchased
contraceptives from a chain of personal health and
beauty retailers (52.8%), convenience store and
supermarket (43.9%), or pharmacy (23.6%). They
usually sought contraceptive information from
an online health website (46.5%), online forum
(40.1%), gynaecologists (27.8%), or family planning
clinic (21.6%). A summary of the socio-demographic
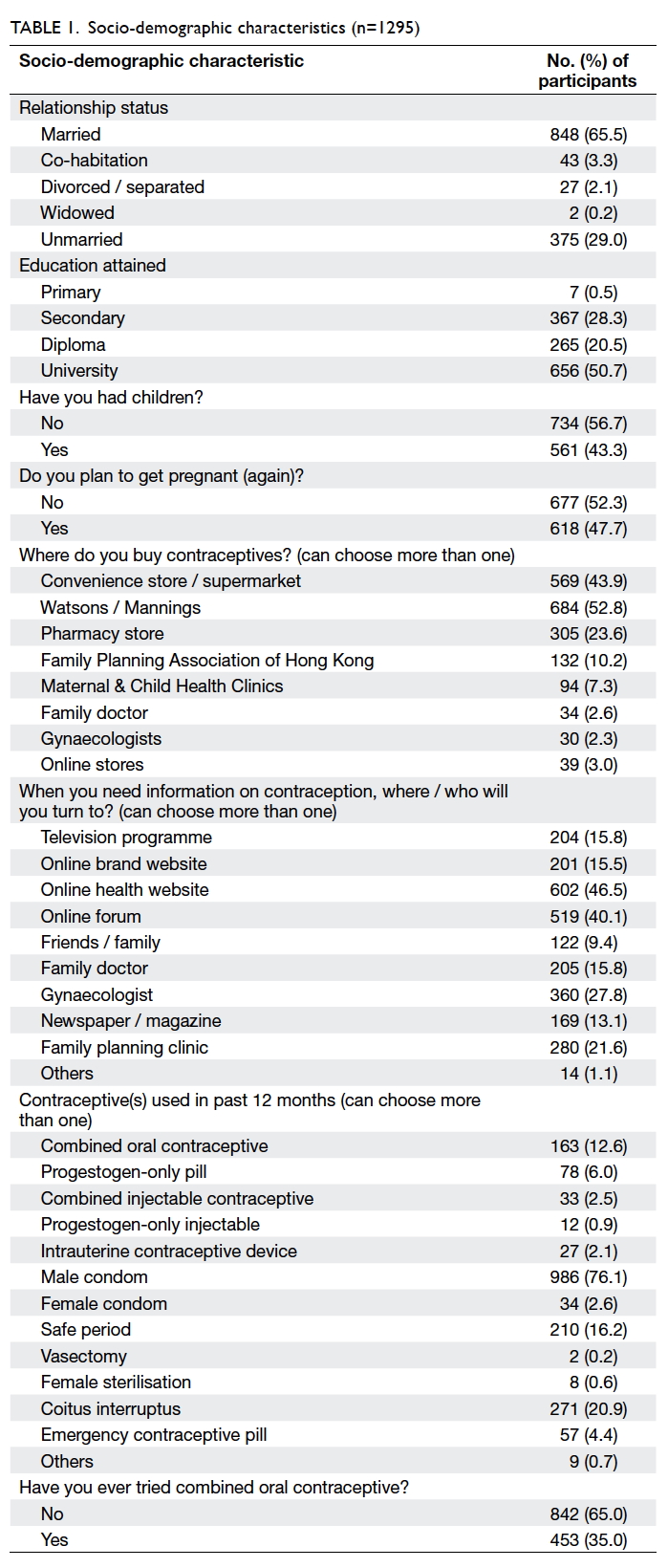
characteristics is shown in Table 1.
Among the 1295 respondents, 453 (35.0%)
had used more than one type of contraceptive in the
previous 12 months. The contraceptive choices of
the whole group were: male condom (76.1%), coitus
interruptus (20.9%), safe period (16.2%), and COC
pill (12.6%) [Table 1]. The contraceptive choices of the 986 male condom users were further analysed
to estimate their risk of unplanned pregnancy.
Among them, 598 (60.6%) used a male condom
alone, 295 (29.9%) also used other less effective
contraceptives such as a female condom, safe period,
and coitus interruptus but whether they used them
all together during coitus or switched between
these contraceptives was unknown. Therefore,
these condom users were indisputably at risk for
unplanned pregnancy because they did not use other
effective contraceptives with the male condom.
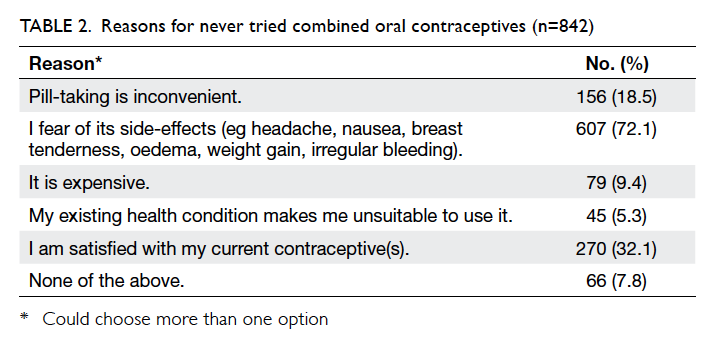
In this study sample, 842 (65.0%) women had
never tried a COC pill. The main reasons were
fear of side-effects (72.1%), satisfied with their
current contraceptive (32.1%), and pill-taking was
inconvenient for them (18.5%) [Table 2]. Among
453 women who had tried a COC pill, the median
age they started use was 24 years (interquartile
range, 20-28 years). Use of COC pill was associated
with older age (mean ± standard deviation: users and non-users was 33.4 ± 5.8 and 32.4 ±
5.5 years, respectively; t test, P=0.003), not planning to
get pregnant (P=0.002), and university education
(P=0.004). There was no association with relationship
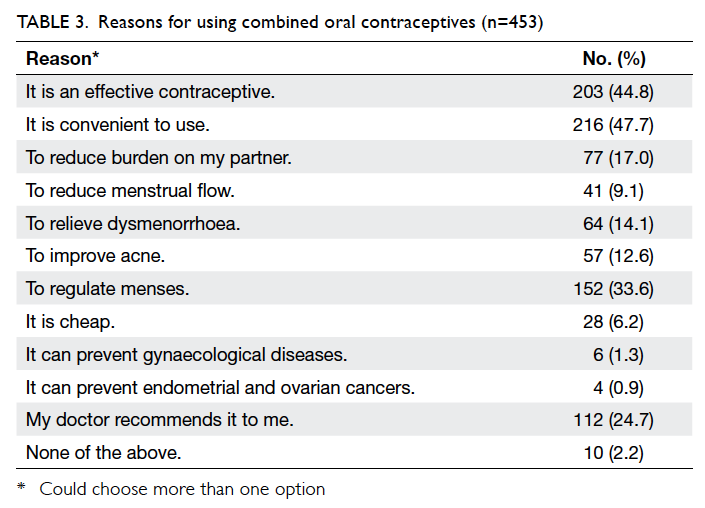
status (P=0.968) or parity (p=0.427). These women
preferred the COC pill because of convenience
(47.7%), effectiveness (44.8%), menstrual regulation
(33.6%), recommendation by their doctor (24.7%),
reduced burden to partner (17.0%), for relief of
dysmenorrhoea (14.1%), and improvement of acne
(12.6%) [Table 3]. They chose a COC pill based on
the dosage of hormones, type of hormones, and
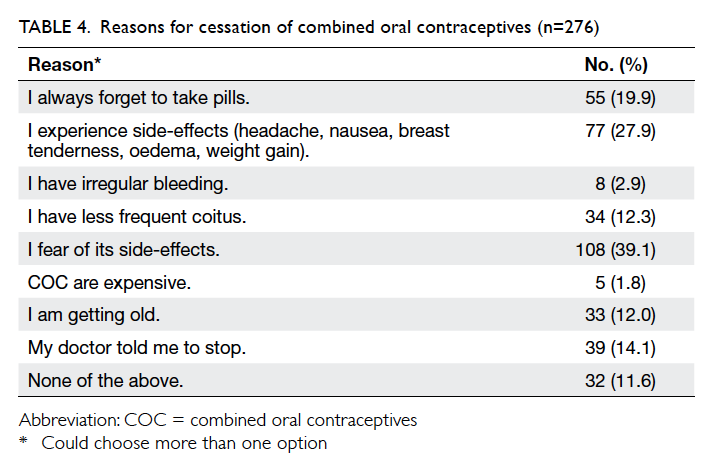
price. Among the 453 ever-users, 177 (39.1%) had
been taking a COC pill in the previous 12 months.
Use had stopped in 276 because they feared side-effects
(39.1%); they experienced side-effects such
as nausea, vomiting, breast tenderness, oedema, or
weight gain (27.9%); they consistently forgot to take
pills (19.9%); their doctor told them to stop (14.1%);
or they were having less frequent coitus (12.3%)
(Table 4).
Discussion
The pattern of contraceptive use in this study
sample was similar to that in the 2012 territory-wide
survey.1 Male condom was the most popular
contraceptive, used by 76.1% of couples in our study.
The proportion of women using a COC pill in our
study was also similar to that in the 2012 survey.
Our survey has provided some information about
the characteristics of women who chose to take the
COC pill, such as older age, university education,
and no plan for future pregnancy. A similar age
profile and education attainment were identified in
a national survey conducted in the US,6
in which parity and relationship
status were also characteristics associated with COC
pill use.
Fear of side-effects was the major reason cited
by both subgroups of women who stopped or had
never tried a COC pill. Studies carried out in both
developed and developing countries have also shown
that the experience of side-effects as well as the fear of
side-effects are major reasons for discontinuation.7 8 9 10
It appeared that fear of side-effects was a unique
barrier across different countries and cultures.
Minor side-effects such as breast tenderness, fluid
retention, nausea, and vomiting were transient and
usually subsided after one to two cycles. Major
health hazards such as myocardial infarction, stroke,
thromboembolism, breast cancer, and cervical cancer
are rare. Two meta-analyses showed a 2-fold increase
in myocardial infarction and stroke in low-dose COC
pill users compared with non-users.11 12 The risk of
venous thromboembolism was increased by 3- to
5-fold depending on the type of progestogen used.13
Since the baseline incidence of these vascular events
in women of reproductive age is very low (myocardial
infarction: 0.2 per 100 000 at age 30-34 years to 2.0 at
age 40-44 years14; stroke: 1 per 100 000 at age 30-34
years to 1.6 at age 40-44 years14; thromboembolism:
2 per 10 000 women at reproductive age15), the
absolute risk of such vascular complications is very
small. Breast cancer risk with a low-dose COC pill
is also small. A large meta-analysis of case-control
studies from 25 countries showed a modest increase
in breast cancer risk with the COC pill (relative
risk=1.24; 95% confidence interval [CI], 1.15-1.33).16
The risk of cervical cancer depends on the duration
of use. Women who used a COC pill for less than 5
years have no increased risk of cervical cancer. The
odds ratio for cervical cancer after using COC for 5 to 9
years was 2.82 (95% CI, 1.46-5.42) and 4.03 (95% CI,
2.09-8.02) for 10 years or longer.17 Cervical cancer is
largely preventable by regular cervical smears, safe
sex, as well as avoidance of smoking. The overall
morbidity and mortality associated with the low-dose
COC pill are low and most healthy women can
use it without major concerns.
The lack of access to consultation services has
exacerbated concern about side-effects, both for
women who experience them and for those who
fear them.9 At our clinics, women are counselled
about the common side-effects and complications
of the COC pill. This prevents them from panicking
when minor side-effects occur. They are also told to
stop taking the COC pill immediately and consult
a doctor if they develop signs and symptoms of a
major complication. Such counselling helps women
establish realistic expectations and they are able
to use COC safely. An information sheet detailing
side-effects and complications, warning signs and
symptoms for major complications, commonly
used drugs that interact with COC pill, and missed
pill management is given to all users. When first
prescribed, we usually provide two packs and then
review acceptability after 2 months. Women are
advised that different COC pills vary slightly in
their side-effect profile and they can change to
another formulation if they have problems. We also
offer walk-in clinics for any woman who wishes to
get contraceptive advice from nurses. The above
COC pill delivery mode conforms to the World Health
Organization recommendations.18
Apart from side-effects and complications,
women should be informed of the non-contraceptive
benefits of the COC pill, such as menstrual
regulation and relief of dysmenorrhoea; reduced
risk for endometrial, ovarian, and colorectal cancers;
lower incidence of gynaecological diseases such as
endometriosis, pelvic inflammatory disease, ectopic
pregnancy; and improved acne and bone health. All
such information should be shared with women to
help them establish an impartial perspective on the
risks and benefits of the COC pill.
The main limitation of this survey is the very
low response rate, albeit not unexpected with online
survey. There was also selection bias as members
of an exclusive group were invited to participate.
Those who participated in the survey prompted
self-selection bias as they might be systematically
different from those who chose not to respond.
When we planned the study, we had explored other
alternatives such as face-to-face interview, phone
interview, or online survey for the general public.
Nonetheless, the first would be too expensive and
in the last two alternatives, we would be unable to
verify respondent’s age or gender. We settled with this
arrangement as it was the most convenient means to
reach our target group since ESDlife only allowed
female members aged 18 to 45 years to participate.
The demographic statistics provided by ESDlife
revealed that the education attainment and income
reported by its female members were better than
the population average. The contraceptive choice
in this group matched that of the population study
and the sample size was not small. Although the
results obtained cannot be generalised to the local
population, we believe they provide useful insight
into the reasons why women do or do not use the
COC pill. The other limitation is the number of
questions we could ask was limited by the budget. If
we had a larger budget to include more questions, we
would have explored the type of COC pill used, total
duration of use, and the switch pattern in women
who used more than one contraceptive in the
previous 12 months. Lastly, there was a discrepancy
in the number of women who were using a COC pill
in the past 12 months. For “Question 15. Are you
still on COC in the past 12 months?”, 177 responded
positively. In response to Question 7, however, only
163 chose COC pill as one of the contraceptives
they had used in the past 12 months. Some women
might have omitted COC when they selected their
contraceptives from the list provided in Question 7.
Conclusions
The COC pill remains underutilised in Hong Kong
compared with many western countries. The male
condom is the most popular contraceptive and the
proportion of women using a COC pill is one sixth of
that of women who use a male condom. A considerable
proportion of respondents expressed concerns
about actual or anticipated side-effects. Doctors
should focus on this area during contraceptive
counselling and help dispel the underlying myths and
misconceptions surrounding COC pill use. Studies
have shown that minor side-effects are transient,
major complications are rare in healthy women, and
there are many non-contraceptive benefits of the
COC pill. These facts should be emphasised during
COC counselling to help women balance the risks
and benefits of the COC pill and make an informed
choice about contraception.
Declaration
Sponsorship was provided by Pfizer Corporation
Hong Kong Limited to cover all costs incurred with
ESDlife and incentives for participants. The company
was not involved in the study design, execution, data
interpretation, or manuscript preparation.
References
1. Family Planning Knowledge, Attitude and Practice in
Hong Kong Survey 2012. Available from: http://www.famplan.org.hk/fpahk/en/template1.asp?style=template1.asp&content=info/research.asp. Accessed 6 Aug 2015.
2. Trussell J. Contraceptive failure in the United States.
Contraception 2011;83:397-404. Crossref
3. United Nations. Department of Economic and Social
Affairs. Population Division. World contraceptive
patterns 2013. Available from: http://www.un.org/en/development/desa/population/publications/pdf/family/worldContraceptivePatternsWallChart2013.pdf. Accessed
6 Aug 2015.
4. Heise L. Beyond acceptability: reorienting research
on contraceptive choice. In: Ravindran TS, Berer M,
Cottingham J, editors. Beyond acceptability: users’
perspectives on contraception. London: Reproductive
Health Matters; 1997: 6-14.
5. User preferences for contraceptive methods in India, Korea,
the Philippines, and Turkey. World Health Organization
Task Force on Psychosocial Research in Family Planning
and Task Force on Service Research in Family Planning.
Stud Fam Plann 1980;11:267-73.
6. Hall KS, Trussell J. Types of combined oral contraceptives
used by US women. Contraception 2012;86:659-65. Crossref
7. Ali M, Cleland J. Contraceptive discontinuation in six
developing countries: a cause-specific analysis. Int Fam
Plan Perspect 1995;21:92-7. Crossref
8. Sanders SA, Graham CA, Bass JL, Bancroft J. A prospective
study of the effects of oral contraceptives on sexuality
and well-being and their relationship to discontinuation.
Contraception 2001;64:51-8. Crossref
9. D’Antona Ade O, Chelekis JA, D’Antona MF, Siqueira AD.
Contraceptive discontinuation and non-use in Santarém,
Brazilian Amazon. Cad Saude Publica 2009;25:2021-32. Crossref
10. Larsson G, Blohm F, Sundell G, Andersch B, Milsom I. A
longitudinal study of birth control and pregnancy outcome
among women in a Swedish population. Contraception
1997;56:9-16. Crossref
11. Baillargeon JP, McClish DK, Essah PA, Nestler JE.
Association between the current use of low-dose oral
contraceptives and cardiovascular arterial disease: a meta-analysis.
J Clin Endocrinol Metab 2005;90:3863-70. Crossref
12. Khader YS, Rice J, John L, Abueita O. Oral contraceptives
use and the risk of myocardial infarction: a meta-analysis.
Contraception 2003;68:11-7. Crossref
13. Faculty of Sexual and Reproductive Healthcare Statement.
Venous thromboembolism and hormonal contraception.
November 2014. Available from: http://www.fsrh.org/pdfs/FSRHStatementVTEandHormonalContraception.pdf. Accessed 6 Aug 2015.
14. Farley TM, Meirik O, Collins J. Cardiovascular disease and
combined oral contraceptives: reviewing the evidence and
balancing risks. Human Reprod Update 1999;5:721-35. Crossref
15. European Medicines Agency. Benefits of combined
hormonal contraceptives (CHCs) continue to outweigh
risks. Product information updated to help women make
informed decisions about their choice of contraception.
London, UK: EMA, 2014. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/referrals/Combined_hormonal_contraceptives/human_referral_prac_000016.jsp&mid=WC0b01ac05805c516f.
Accessed 6 Aug 2015.
16. Collaborative Group on Hormonal Factors in Breast Cancer.
Breast cancer and hormonal contraceptives: collaborative
reanalysis of individual data on 53 297 women with breast
cancer and 100 239 women without breast cancer from 54
epidemiological studies. Lancet 1996;347:1713-27. Crossref
17. Moreno V, Bosch FX, Muñoz N, et al. Effect of oral
contraceptives on risk of cervical cancer in women with
human papillomavirus infection: the IARC multicentric
case-control study. Lancet 2002;359:1085-92. Crossref
18. World Health Organization. Family Planning: A Global
Handbook for Providers. 2011 edition. Available from:
https://www.fphandbook.org/sites/default/files/chap_1_eng.pdf. Accessed 6 Aug 2015.