Hong Kong Med J 2016 Apr;22(2):184.e3–4
DOI: 10.12809/hkmj154821
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Median arcuate ligament syndrome
FH Ng, MB, ChB, FRCR;
Ophelia KH Wai, MB, ChB, FRCR;
Agnes WY Wong, MB, ChB, FRCR;
SM Yu, MB, ChB, FRCR
Department of Radiology and Organ Imaging, United Christian Hospital,
Kwun Tong, Kowloon, Hong Kong
Corresponding author: Dr FH Ng (nfh667@ha.org.hk)
Case
A middle-aged man admitted with abdominal
pain and anaemia in December 2015. A computed
tomographic (CT) angiogram demonstrated a
superior indentation with focal narrowing in the
proximal celiac axis (Fig 1). Conventional superior
mesenteric arteriogram demonstrated prominent
collaterals, and retrograde flow of contrast from the
superior mesenteric artery (SMA) to the hepatic
arteries (Fig 2). It was likely related to chronic
compression of the proximal celiac artery. Low
insertion of the median arcuate ligament (MAL) can
be found in normal asymptomatic people. In this
case, prominent collaterals and the retrograde flow
from the SMA supported the diagnosis and may
have explained his symptoms. In symptomatic cases,
surgical division of the median arcuate ligament is
the mainstay of treatment.
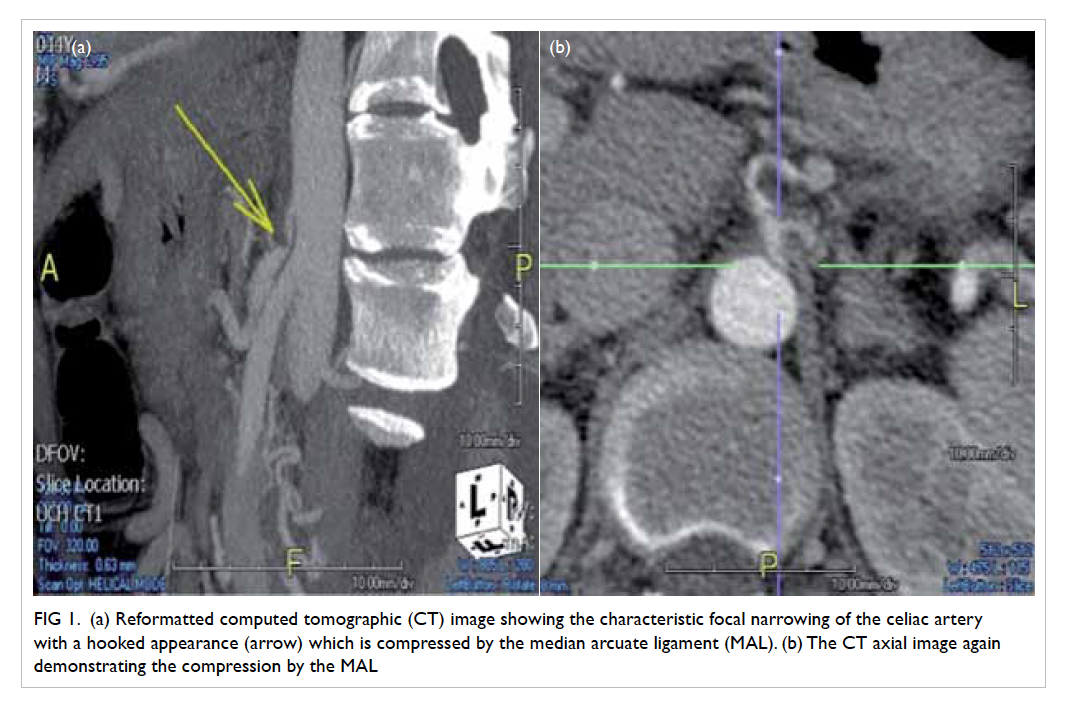
Figure 1. (a) Reformatted computed tomographic (CT) image showing the characteristic focal narrowing of the celiac artery with a hooked appearance (arrow) which is compressed by the median arcuate ligament (MAL). (b) The CT axial image again demonstrating the compression by the MAL
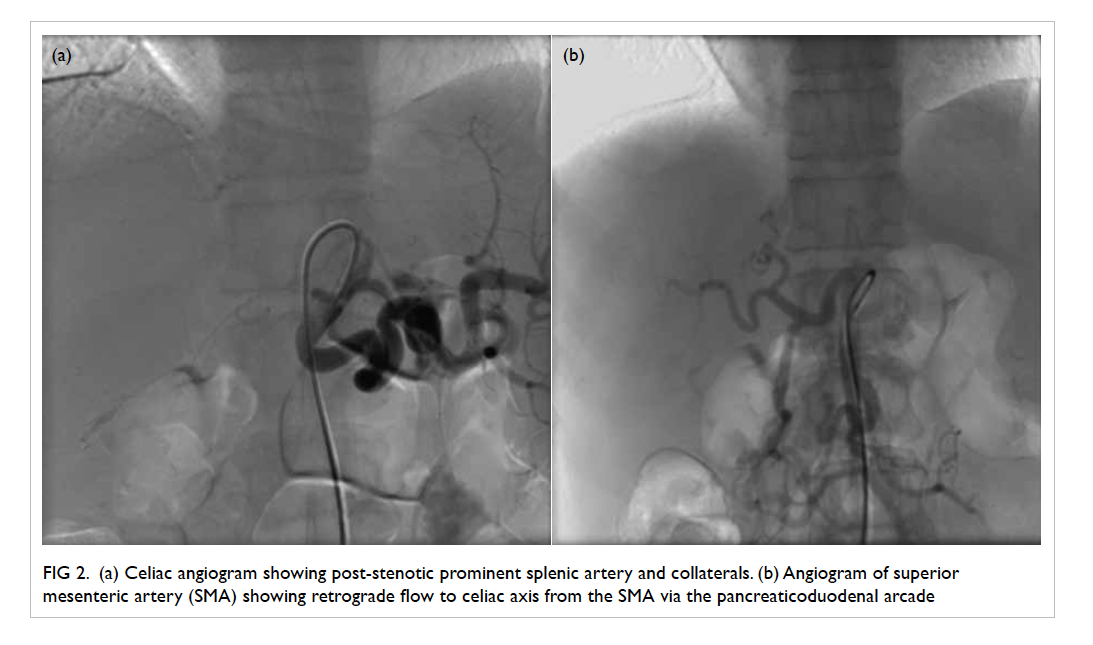
Figure 2. (a) Celiac angiogram showing post-stenotic prominent splenic artery and collaterals. (b) Angiogram of superior mesenteric artery (SMA) showing retrograde flow to celiac axis from the SMA via the pancreaticoduodenal arcade
Discussion
The MAL is a fibrous arch that unites the
diaphragmatic crura on either side of the aortic
hiatus. The crura pass superior and anterior to
surround the aortic opening and to join the central
tendon of the diaphragm. The ligament usually passes
superior to the origin of the celiac axis. The insertion
of the ligament may be low and therefore crossover
the proximal portion of the celiac axis, causing
a characteristic indentation. If it is significantly
compressed on the celiac axis, this will compromise
vascular flow and produce symptoms.
The MAL syndrome was first described in
1963 by Harjola1 and in 1965 by Dunbar et al.2 The definition of the syndrome relies on a combination
of both clinical and radiographic features. Clinically,
they described a classical triad of chronic postprandial
abdominal pain, epigastric bruit, and weight loss.3 4 Extrinsic compression of the celiac trunk by the
MAL occurs in 10% to 24% of patients.1 Usually,
patients are asymptomatic and the classical triad
is not always present, presumably due to collateral
supply from the superior mesenteric circulation.1 2 The disease typically occurs in young patients and
is more common in thin women who may present
with epigastric pain and weight loss.1 The abdominal
pain may be associated with eating, but not always.1
On physical examination, an abdominal bruit that
varies with respiration may be audible in the mid-epigastric
region. Symptoms are thought to arise
from compression of the celiac axis with consequent
compromised blood flow.
The diagnosis of celiac artery compression
is traditionally made following conventional
angiography. The use of thin-section multidetector
CT and three-dimensional imaging techniques
has greatly improved the ability to non-invasively
obtain detailed images of the mesenteric vessels.
Compression of the celiac axis by the MAL
produces characteristic findings visible on CT
angiography. Computed tomographic angiography
can play a role in the diagnosis of this condition by
demonstrating the characteristic focal narrowing of
the celiac artery (Fig 1) with a hooked appearance
that distinguishes this condition from other causes
of celiac artery narrowing, such as atherosclerotic
disease. Indentation of the origin of coeliac artery is
exacerbated during the expiratory phase. Repeating
CT on inspiration can often distinguish clinically
significant narrowing from transient compression
seen only during expiration in some patients, and is
how most abdominal CT studies are performed.1
The majority of affected patients have no
symptoms, thus radiographic finding of celiac
axis compression alone may not be significant,
unless it is correlated with clinical symptoms.
Severe compression occurs in approximately 1% of
patients.1 Severe stenosis will result in post-stenotic
dilatation, and in some cases, the celiac axis will be
fed by the SMA via the pancreaticoduodenal arcade.
This was evident on the angiogram of our patient
with prominent collaterals and retrograde flow
from the SMA (Fig 2). His CT angiogram showed a
characteristic hooked focal narrowing at the superior
proximal celiac artery (Fig 1).
The surgical management of MAL syndrome
is controversial.1 2 Surgical treatment in severe cases is advocated, particularly in cases with post-stenotic
dilatation and collateral vessels (Fig 2), by division
of the ligament. A laparoscopic approach is being
increasingly adopted. Celiac angioplasty and stenting
by endovascular means may be a future hot topic.2
References
1. Harjola PT. A rare obstruction of the coeliac artery: report
of a case. Ann Chir Gynaecol Fenn 1963;52:547-50.
2. Dunbar JD, Molnar W, Beman FF, Marable SA.
Compression of the celiac artery and abdominal angina.
Am J Roentgenol Radium Ther Nucl Med 1965;95:731-44. Crossref
3. Horton KM, Talamini MA, Fishman EK. Median arcuate
ligament syndrome: evaluation with CT angiography.
Radiographics 2005;25:1177-82. Crossref
4. Duffy AJ, Panait L, Eisenberg D, Bell RL, Roberts KE,
Sumpio B. Management of median arcuate ligament
syndrome: a new paradigm. Ann Vasc Surg 2009;23:778-84. Crossref

