DOI: 10.12809/hkmj144362
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Primary gestational choriocarcinoma of the
vagina: magnetic resonance imaging findings
T Wong, FRCR; Eliza PY Fung, FHKCR, FHKAM (Radiology); Alfred WT Yung, FHKCR, FHKAM (Radiology)
Department of Radiology, Princess Margaret Hospital, Laichikok, Hong Kong
Corresponding author: Dr T Wong (gloria_wong@live.com)
Case report
A 33-year-old nulligravid Filipino woman was
admitted to the gynaecology ward of Princess
Margaret Hospital in April 2014, with lower
abdominal pain and recurrent retention of urine. Her
pregnancy test was positive. Per-vaginal examination
revealed a 4-cm firm, fixed, and wide-based vaginal
mass with smooth wall over the upper anterior
vagina. Bedside transabdominal ultrasonography
confirmed a 4.5-cm solid mass in the anterior vagina
and a 3.5-cm intramural fibroid over the left side
of the uterus. No adnexal mass or free fluid was
seen. Beta human chorionic gonadotropin (β-hCG)
level was elevated to 270 743 IU/L (reference level,
<5.0 IU/L for non-pregnant women), and repeated
checking 3 days later was 253 957 IU/L. Alpha-fetoprotein,
carcinoembryonic antigen, and Ca-125
were negative. A urologist was consulted and the
patient underwent flexible cystoscopy that revealed
indentation of the urinary bladder by an external
mass. Mild erythematous changes were visualised
at the right urinary bladder base. Biopsy revealed
inflammation but no malignant cells.
Magnetic resonance imaging (MRI) of the
pelvis revealed a 4.8 cm x 5.2 cm x 4 cm (craniocaudal
x anteroposterior x transverse) mass located at the
anterior aspect of the vagina. It was hypointense
with a faint hyperintense rim on T1-weighted
images (Fig 1a) and heterogeneously hyperintense
with hypointense rim on T2-weighted images (Fig 1b). Peripheral enhancement was observed while the
central part remained non-enhanced (Figs 1c and 1d). Part of the mass closely abutted the cervix and
urinary bladder, where intervening fat planes could
not be well-delineated. The urinary bladder wall was
trabeculated. Dilated enhancing tortuous tubular
structures were seen at the left adnexal region and
numerous signal void foci were observed at the
uterine wall. These were due to the presence of high-flow
vasculatures related to tumour hypervascularity
(Figs 1e to 1h). There was also an incidental finding
of a predominantly T2 hypointense non-enhancing
intramural fibroid at the posterior uterine fundus
(Figs 1b and 1d). No ovarian mass was detected and
no intra-uterine gestational sac or ectopic pregnancy.
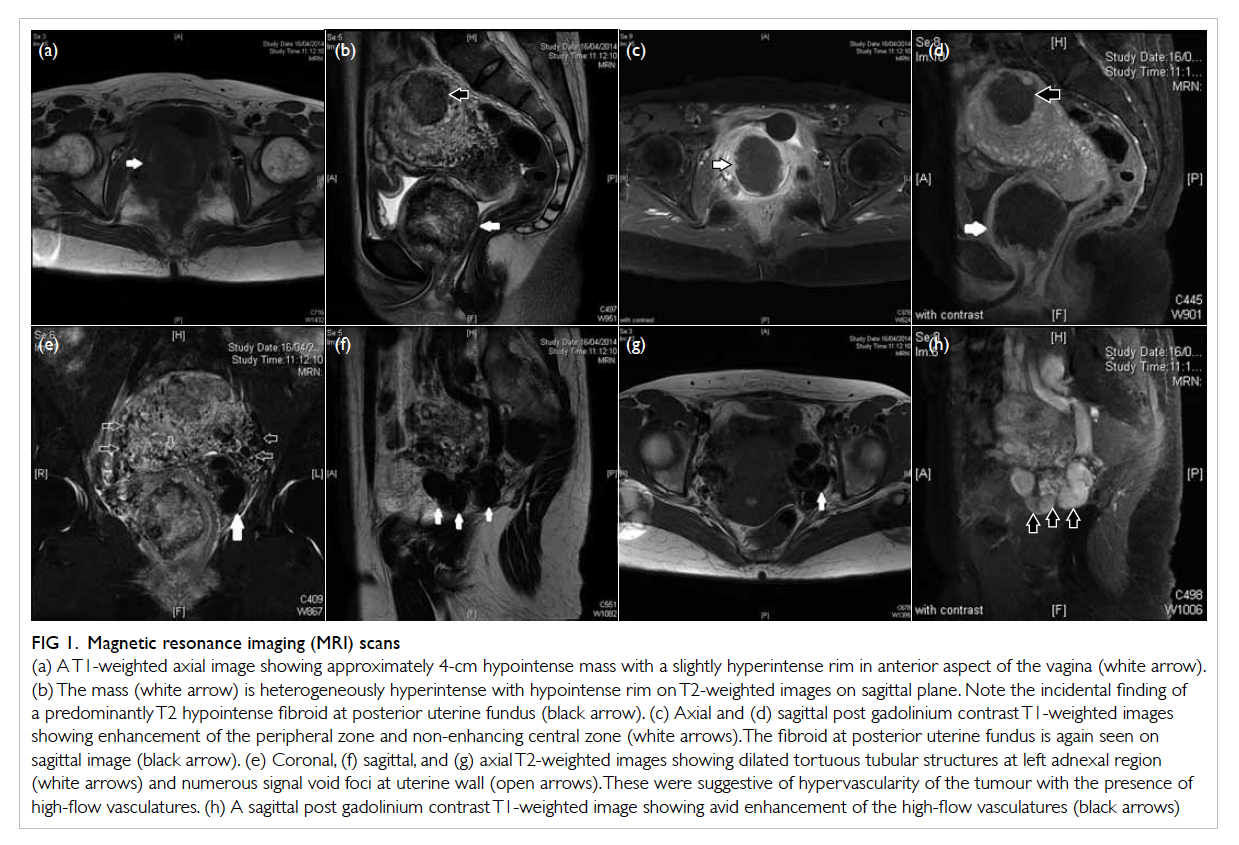
Figure 1. Magnetic resonance imaging (MRI) scans
(a) A T1-weighted axial image showing approximately 4-cm hypointense mass with a slightly hyperintense rim in anterior aspect of the vagina (white arrow). (b) The mass (white arrow) is heterogeneously hyperintense with hypointense rim on T2-weighted images on sagittal plane. Note the incidental finding of a predominantly T2 hypointense fibroid at posterior uterine fundus (black arrow). (c) Axial and (d) sagittal post gadolinium contrast T1-weighted images showing enhancement of the peripheral zone and non-enhancing central zone (white arrows). The fibroid at posterior uterine fundus is again seen on sagittal image (black arrow). (e) Coronal, (f) sagittal, and (g) axial T2-weighted images showing dilated tortuous tubular structures at left adnexal region (white arrows) and numerous signal void foci at uterine wall (open arrows). These were suggestive of hypervascularity of the tumour with the presence of high-flow vasculatures. (h) A sagittal post gadolinium contrast T1-weighted image showing avid enhancement of the high-flow vasculatures (black arrows)
Later examination under anaesthesia
revealed that the lower part of the vaginal lesion
had ruptured. Excision of part of the vaginal lesion
was performed. Tissue frozen section confirmed
it to be choriocarcinoma with no other germ cell
component. DNA polymorphism analysis was
performed in a microsatellite analysis using six
markers by extracting DNA from the microdissected
tumour cells, then comparing it with normal DNA
extracted from a peripheral blood sample. The result
favoured gestational choriocarcinoma. In addition,
chest X-ray revealed multiple ill-defined opacities in
both lungs, measuring about 0.8 to 1.2 cm in size (Fig 2a).
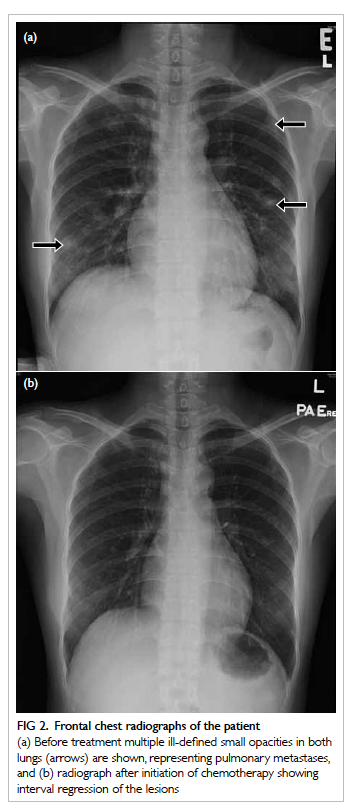
Figure 2. Frontal chest radiographs of the patient
(a) Before treatment multiple ill-defined small opacities in both lungs (arrows) are shown, representing pulmonary metastases, and (b) radiograph after initiation of chemotherapy showing interval regression of the lesions
The patient was diagnosed with primary
gestational choriocarcinoma of the vagina with
lung metastases, and suspicious infiltration of
the urinary bladder and cervix. She was further
managed at the gynae-oncology specialist centre
and given chemotherapy (etoposide, methotrexate,
actinomycin, and cisplatinum). The β-hCG level
dropped to 5604 IU/L with interval regression of the
pulmonary nodules after initiation of chemotherapy
(Fig 2b).
Discussion
Gestational trophoblastic disease comprises
a wide spectrum of benign/premalignant to
malignant conditions and includes hydatidiform
mole (complete or partial), invasive mole,
choriocarcinoma, and placental-site trophoblastic
tumour. The incidence varies in different countries
with the highest rate noted in South-East Asia. The
cause of such variation is not well understood.1
Choriocarcinoma is a malignant form of gestational
trophoblastic neoplasia, and generally arises in
the uterine corpus of women of reproductive age
with coincident or antecedent pregnancy. Primary
extrauterine choriocarcinoma is rare and most
reported cases have occurred in the uterine cervix.2
It is thought to arise along the path of migration
of germ cells to gonads, or de-differentiated from
another histological type.3 Our case was very unusual
as it occurred in the vagina. The most common site
of metastasis for choriocarcinoma is lung,1 and this
also occurred in our patient.
The clinical diagnosis of extrauterine
choriocarcinoma is extremely difficult as symptoms
are often non-specific. Vaginal bleeding is the
most common presenting symptom,2 but as such
often mimics other more common disease entities.
Primary extrauterine choriocarcinoma has been
misdiagnosed as ectopic pregnancy,2 4 dysfunctional
uterine haemorrhage,5 and cervical polyp.6 This can
often lead to a delay in proper management. Since
trophoblastic neoplasm such as choriocarcinoma
produces an excessive amount of β-hCG, serial
monitoring of its trend is very helpful for diagnosis
and follow-up of treatment response. The mainstay
of treatment is chemotherapy, as choriocarcinoma
is highly chemosensitive.2 For a nulligravid woman
as in this case, differentiation between gestational
or non-gestational origin merely from a clinical
history can be confusing. Differentiation by DNA
polymorphism analysis is useful to guide the
management as non-gestational choriocarcinoma is
known to have a worse prognosis and to be resistant
to single-agent chemotherapy.7
To the best of our knowledge, the imaging
findings of primary extrauterine choriocarcinoma
are rarely described in the literature, particularly
that of vaginal origin. In the present case, MRI
showed a hypointense vaginal tumour with
hyperintense rim on T1-weighted images and
heterogeneously hyperintense with hypointense
rim on T2-weighted images. Rim enhancement was
observed on T1-weight images after gadolinium
contrast injection. The non-enhancing centre of the
tumour could be due to tumour necrosis, commonly
seen in choriocarcinoma. Poor delineation of fat
planes with cervix and urinary bladder raised the
suspicion of tumour involvement. Features of
chronic bladder outlet obstruction were present
as suggested by the trabeculated bladder outline.
The signal void foci over the uterine wall and the
high-flow vasculatures at the left adnexal region
signified angiogenesis and neovascularisation, thus
the hypervascular nature of the tumour.1 This is in
accordance with the characteristic hypervascularity
of choriocarcinoma.5 6 The multiple nodular
opacities on chest X-ray most likely represented lung
metastases, although histological confirmation was
not performed. Interval shrinkage of these nodules
was observed on chest X-ray following initiation of
treatment.
In summary, imaging findings of a
hypervascular tumour and exceedingly high levels
of β-hCG are useful in making the diagnosis of
extrauterine choriocarcinoma, and MRI is valuable
in assessing extrauterine extension, tumour
vascularity, and overall staging of the tumour.
References
1. Allen SD, Lim AK, Seckl MJ, Blunt DM, Mitchell AW.
Radiology of gestational trophoblastic neoplasia. Clin
Radiol 2006;61:301-13. Crossref
2. Kairi-Vassilatou E, Papakonstantinou K, Grapsa D,
Kondi-Paphiti A, Hasiakos D. Primary gestational
choriocarcinoma of the uterine cervix. Report of a case and
review of the literature. Int J Gynecol Cancer 2007;17:921-5. Crossref
3. Dilek S, Pata O, Tok E, Polat A. Extraovarian nongestational
choriocarcinoma in a postmenopausal woman. Int J
Gynecol Cancer 2004;14:1033-5. Crossref
4. Gerson RF, Lee EY, Gorman E. Primary extrauterine
ovarian choriocarcinoma mistaken for ectopic pregnancy:
sonographic imaging findings. AJR Am J Roentgenol
2007;189:W280-3. Crossref
5. Maestá I, Michelin OC, Traiman P, Hokama P, Rudge MV.
Primary non-gestational choriocarcinoma of the uterine
cervix: a case report. Gynecol Oncol 2005;98:146-50. Crossref
6. Yahata T, Kodama S, Kase H, et al. Primary choriocarcinoma
of the uterine cervix: clinical, MRI, and color Doppler
ultrasonographic study. Gynecol Oncol 1997;64:274-8. Crossref
7. Koo HL, Choi J, Kim KR, Kim JH. Pure non-gestational
choriocarcinoma of the ovary diagnosed by DNA
polymorphism analysis. Pathol Int 2006;56:613-6. Crossref

