DOI: 10.12809/hkmj144421
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Anti-neutrophil cytoplasmic antibody–associated pauci-immune glomerulonephritis in
a patient with chronic lymphocytic leukaemia
CS Yeung, MB, BS, MRCP1; CY Cheung, PhD, FHKAM (Medicine)1; PT Chan, MB, BS, FHKAM (Pathology)2; John W Li, MB, BS, MRCP1; WL Chak, FRCP, FHKAM (Medicine)1; KF Chau, FRCP, FHKAM (Medicine)1
1 Department of Medicine, Queen Elizabeth Hospital, Jordan, Hong Kong
2 Department of Pathology, Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Dr CY Cheung (simoncycheung@gmail.com)
Case report
A 71-year-old woman presented to us in August
2012 with a rash over both lower limbs. Blood
tests revealed leukocytosis with white cell count
of 22 x 109 /L (neutrophil 1.6 x 109 /L, lymphocytes
20 x 109 /L). Serum creatinine level was 53 µmol/L
and serum albumin 42 g/L. Urinalysis showed no
albuminuria or microscopic haematuria. Bone
marrow biopsy confirmed the diagnosis of chronic
lymphocytic leukaemia (CLL). Fluorescence in-situ
hybridisation showed deletion of chromosome
11q22~23. Computed tomography revealed multiple
enlarged lymph nodes in different regions such as
submental, bilateral jugular, left supraclavicular
fossa, mediastinal, hila, axillary, porta hepatis,
para-aortic and bilateral common iliac regions.
Chlorambucil 2 mg twice weekly was prescribed and
the patient was followed up regularly in our clinic.
During this period she had two episodes of sepsis
that were treated successfully with antibiotics.
In October 2013, she was noted to have
progressive bilateral lower limb swelling and facial
puffiness. She also reported frothy urine but no
gross haematuria. She denied taking any herbs or
over-the-counter medication. Physical examination
was unremarkable except for pitting oedema over
both lower limbs. Urinalysis revealed the presence
of 10-50 red blood cells/cm2. The spot urine
protein-to-creatinine ratio was 13.1 g/g. Her serum
creatinine concentration was 364 µmol/L (reference
range [RR], 65-100 µmol/L), albumin was 32 g/L
(RR, 35-52 g/L), globulin was 40 g/L (RR, 22-36 g/L),
haemogloblin was 87 g/L (RR, 134-171 g/L), and
white blood cell count was 26.4 x 109 /L (RR, 3.7-9.2
x 109 /L) [neutrophil 3.9 x 109 /L, lymphocytes 22.1 x
109 /L]. The liver function was normal. Anti-nuclear
antibody was positive (titre 1:80, homogeneous
pattern) but anti-DNA was negative. Her anti-neutrophil
cytoplasmic antibodies (ANCA) were
positive with perinuclear staining pattern (pANCA)
and the anti-myeloperoxidase (anti-MPO) antibody
titre was >100 U/mL (reference level, <5 U/mL).
The complement level was normal and hepatitis
serology was negative. Urine culture showed no
bacterial growth. Ultrasound-guided renal biopsy
was performed. Light microscopic examination
showed 21 glomeruli, three of which showed
global glomerulosclerosis (Fig 1). Twelve glomeruli
featured crescent formation (3 had cellular crescent,
6 had fibrocellular crescent, and 3 had fibrous
crescent). Fibrinoid necrosis was also identified.
Nonetheless, immunohistochemical staining
showed several atypical lymphoid cell aggregates
composed of small- to medium-sized lymphoid cells
expressing B-cell markers CD20, CD5, CD23 and
LEF-1 (Fig 2). They were negative for T-cell marker
CD3, follicular centre marker CD10 and cyclin D1.
The overall features supported the diagnosis of
ANCA-associated crescentic glomerulonephritis
and renal involvement of CLL. She was given 3
days of intravenous pulse methylprednisolone 500
mg, followed by daily oral prednisolone 30 mg and
cyclophosphamide 50 mg. In addition, chlorambucil
was stopped and monthly rituximab (first dose
375 mg/m2, subsequent doses 500 mg/m2) was
administered. After 6 months, her lymphocyte count
was normal and serum creatinine level was around
142 µmol/L. Proteinuria also reduced to 1.12 g/day
and her last anti-MPO level was 11 U/mL.
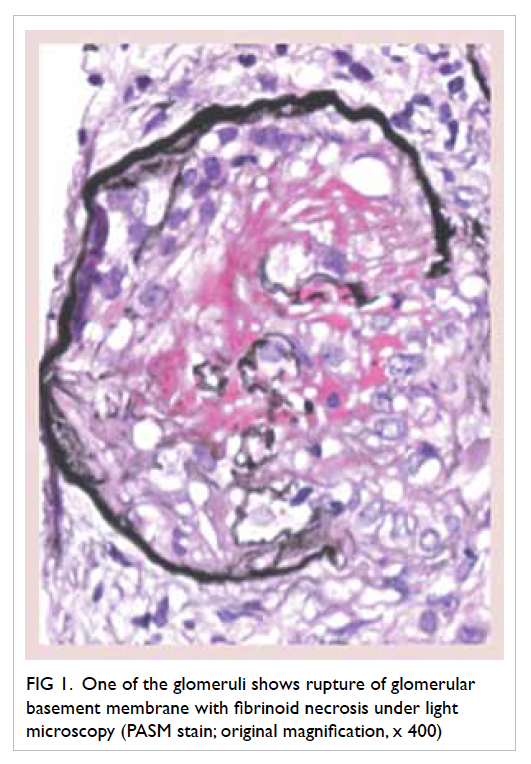
Figure 1. One of the glomeruli shows rupture of glomerular basement membrane with fibrinoid necrosis under light microscopy (PASM stain; original magnification, x 400)
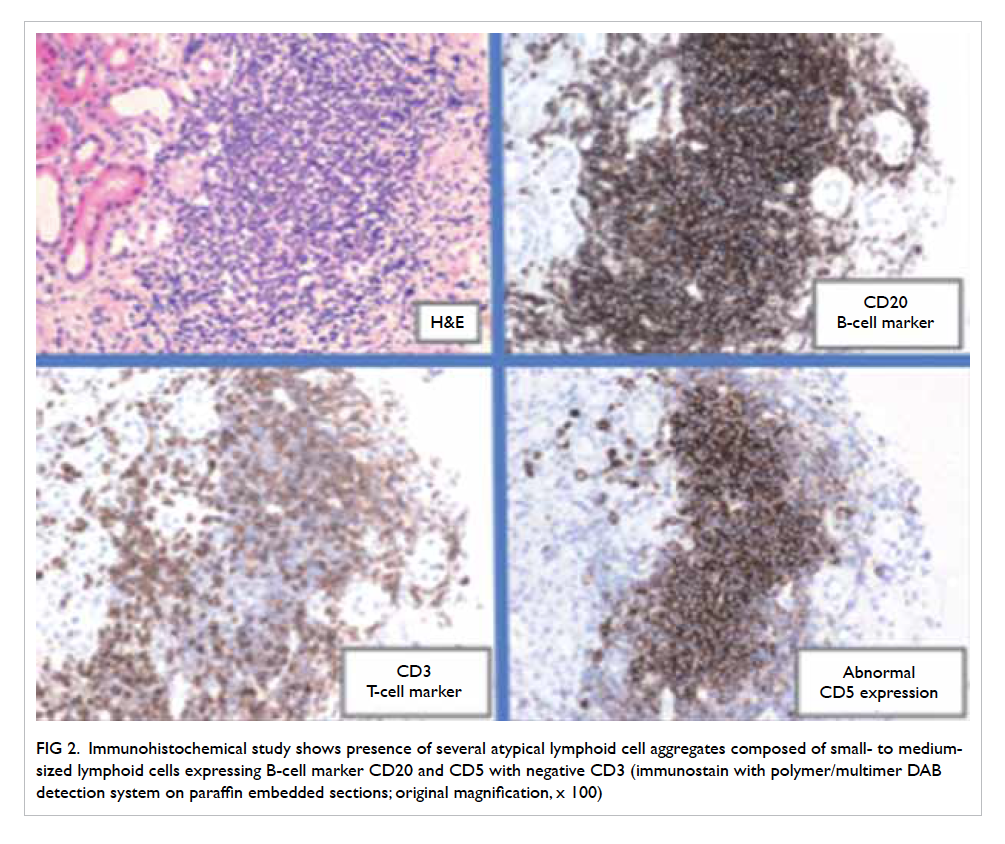
Figure 2. Immunohistochemical study shows presence of several atypical lymphoid cell aggregates composed of small- to mediumsized lymphoid cells expressing B-cell marker CD20 and CD5 with negative CD3 (immunostain with polymer/multimer DAB detection system on paraffin embedded sections; original magnification, x 100)
Discussion
We present a rare case of a 71-year-old woman with
ANCA-associated crescentic glomerulonephritis
that occurred simultaneously with renal infiltration
of CLL. Such leukaemia is one of the chronic
lymphoproliferative disorders characterised
by a progressive accumulation of functionally
incompetent lymphocytes that are monoclonal in
origin. In fact, CLL can be considered to be identical
to the mature (peripheral) B cell neoplasm small
lymphocytic lymphoma (SLL) but at different stages
along a continuum. Patients in an early stage of
CLL are usually asymptomatic. The most common
presentation is the incidental finding of leukocytosis,
especially lymphocytosis. Other presenting signs
and symptoms include malaise, weakness, anaemic
symptoms, night sweating, recurrent infection, and
lymphadenopathy. The diagnosis of CLL requires
demonstration of lymphocytes with monoclonal B
cells in either serum or bone marrow. Monoclonal B
cells can be demonstrated by the expression of CD5
antigen.
The disease CLL/SLL is commonly
associated with various glomerular disease
entities such as minimal-change glomerulopathy,
membranoproliferative glomerulonephritis,
membranous glomerulopathy, focal segmental
glomerulosclerosis, light-chain deposition disease,
amyloidosis, and immunotactoid glomerulopathy.1
In addition, CLL can infiltrate various internal
organs such as the kidneys. Previous studies have
shown on autopsy that the kidneys were involved in
60% to 90% of CLL cases.2 3 Renal infiltration of CLL
can be easily missed however, because it is usually
asymptomatic and is not a common cause of acute
kidney injury or end-stage renal disease.4 5 As a
result, the interstitial inflammatory cell infiltrate in
the renal biopsy specimen should be examined with
immunofluorescence and electron microscopy.
Moreover, CLL can also be associated with
autoimmune diseases, notably haematological
diseases such as haemolytic anaemia,
thrombocytopenia, and pure red cell aplasia.6
Approximately 2% of patients with CLL have
associated pANCA positivity.7 Titre of ANCA has
been shown to be involved in the pathogenesis of
pauci-immune crescentic glomerulonephritis.8
Hence, it is not surprising that CLL can be associated
with rapidly progressive glomerulonephritis
(RPGN). The association between CLL/SLL and
RPGN, however, has been shown in only a few case
reports, and while renal histology was lacking in
some of these patients, most of them were found
to have positivity for pANCA and anti-MPO when
serologic tests were available.1 9 10 11 12 13 14
There have been no large-scale randomised
controlled trials for the treatment of CLL-related
pauci-immune glomerulonephritis because of
the limited number of patients. Most reported
cases have been treated in the same way as other
pauci-immune glomerulonephritis.9 Medication
used in the treatment of RPGN such as steroid,
cyclophosphamide, chlorambucil, and rituximab
can also be used to treat CLL. In comparison, the
combination chemotherapy for high-risk CLL—which includes fludarabine, cyclophosphamide, and
rituximab—shows a higher complete response rate.15
It has been postulated that successful treatment of
CLL will eventually result in resolution of RPGN.
In conclusion, we report a rare case of anti-MPO
antibody–related crescentic glomerulonephritis in a
patient with a known history of CLL. Awareness of
this rare complication in patients with CLL with
early screening, close follow-up of renal function,
and timely appropriate treatment are important.
Further trials may be required to determine definitive
treatment when these diseases co-exist.
References
1. Moulin B, Ronco PM, Mougenot B, Francois A, Fillastre
JP, Mignon F. Glomerulonephritis in chronic lymphocytic
leukemia and related B-cell lymphomas. Kidney Int
1992;42:127-35. Crossref
2. Barcos M, Lane W, Gomez G, et al. An autopsy study of
1206 acute and chronic leukemias (1958 to 1982). Cancer
1987;60:827-37. Crossref
3. Schwartz J, Shamsuddin A. The effects of leukemic
infiltrates in various organs in chronic lymphocytic
leukemia. Hum Pathol 1981;12:432-40. Crossref
4. Boudville N, Latham B, Cordingly F, Warr K. Renal failure
in a patient with leukaemic infiltration of the kidney
and polyomavirus infection. Nephrol Dial Transplant
2001;16:1059-61. Crossref
5. Hewamana S, Pepper C, Jenkins C, Rowntree C. Acute
renal failure as the presenting feature of leukaemic
infiltration in chronic lymphocytic leukaemia. Clin Exp
Nephrol 2009;13:179-81. Crossref
6. Diehl LF, Ketchum LH. Autoimmune disease and chronic
lymphocytic leukemia: autoimmune hemolytic anemia,
pure red cell aplasia, and autoimmune thrombocytopenia.
Semin Oncol 1998;25:80-97.
7. Cil T, Altintas A, Isikdogan A, Batun S. Prevalence of
antineutrophil cytoplasmic antibody positivity in patients
with Hodgkin’s and non-Hodgkin lymphoma: a single
center experience. Int J Hematol 2009;9:52-7. Crossref
8. Xiao H, Heeringa P, Hu P, et al. Antineutrophil cytoplasmic
autoantibodies specific for myeloperoxidase cause
glomerulonephritis and vasculitis in mice. J Clin Invest
2002;110:955-63. Crossref
9. Henriksen KJ, Hong RB, Sobrero MI, Chang A. Rare
association of chronic lymphocytic leukemia/small
lymphocytic lymphoma, ANCAs, and pauci-immune
crescentic glomerulonephritis. Am J Kidney Dis
2011;57:170-4. Crossref
10. Biava CG, Gonwa TA, Naughton JL, Hopper J Jr. Crescentic
glomerulonephritis associated with nonrenal malignancies.
Am J Nephrol 1984;4:208-14. Crossref
11. Rivera M, González C, Gonzalo A, Quereda C, Fogué
L, Ortuño J. Vasculitis associated with non-Hodgkin’s
lymphoma. Nephron 1993;65:167-8. Crossref
12. Dussol B, Brunet P, Vacher-Coponat H, Bouabdallah R,
Chetaille P, Berland Y. Crescentic glomerulonephritis with
antineutrophil cytoplasmic antibodies associated with
chronic lymphocytic leukaemia. Nephrol Dial Transplant
1997;12:785-6. Crossref
13. Tisler A, Pierratos A, Lipton JH. Crescentic
glomerulonephritis associated with p-ANCA positivity
in fludarabine-treated chronic lymphocytic leukaemia.
Nephrol Dial Transplant 1996;11:2306-8. Crossref
14. Hamidou MA, El Kouri D, Audrain M, Grolleau JY.
Systemic antineutrophil cytoplasmic antibody vasculitis
associated with lymphoid neoplasia. Ann Rheum Dis
2001;60:293-5. Crossref
15. Robak T, Dmoszynska A, Solal-Céligny P, et al. Rituximab
plus fludarabine and cyclophosphamide prolongs
progression-free survival compared with fludarabine and
cyclophosphamide alone in previously treated chronic
lymphocytic leukemia. J Clin Oncol 2010;28:1756-65. Crossref

