Hong Kong Med J 2016 Apr;22(2):152–7 | Epub 26 Feb 2016
DOI: 10.12809/hkmj144476
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Importance of clothing removal in scalds
Edgar YK Lau, MB, BS, FHKAM (Surgery);
Yvonne YW Tam, MB, ChB, MRCS (HKICSC);
TW Chiu, BMBCh (Oxford), FRCS (Glasgow)
Department of Surgery, Prince of Wales Hospital, Shatin, Hong Kong
Corresponding author: Dr Edgar YK Lau (lyk685@ha.org.hk)
Abstract
Objective: To test the hypothesis that prompt removal of clothing after scalds lessens the severity of injury.
Methods: This experimental study and case series
was carried out in the Burn Centre of a tertiary
hospital in Hong Kong. An experimental burn model
using Allevyn (Smith & Nephew Medical Limited,
Hull, England) as a skin substitute was designed to
test the effect of delayed clothing removal on skin
temperature using hot water and congee. Data of patients
admitted with scalding by congee over a 10-year
period (January 2005 to December 2014) were also
studied.
Results: A significant reduction in the temperature
of the skin model following a hot water scald was
detected only if clothing was removed within the
first 10 seconds of injury. With congee scalds,
the temperature of the skin model progressively
increased with further delay in clothing removal.
During the study period, 35 patients were admitted
with congee scalds to our unit via the emergency
department. The majority were children. Definite
conclusions supporting the importance of clothing
removal could not be drawn due to our small sample
size. Nonetheless, our data suggest that appropriate
prehospital burn management can reduce patient
morbidity.
Conclusions: Prompt removal of clothing after
scalding by congee may reduce post-burn morbidity.
New knowledge added by this study
- In hot water scalds, immediate clothing removal may lead to less severe injury.
- In congee scalds, severity of injury can potentially be reduced with earlier removal of clothing.
- Adequate post-injury first aid with water in congee scalds may lower the chance of requiring surgical intervention.
- Parents should be educated about scald prevention as it is prevalent in the paediatric population.
- It should be emphasised to the general public that immediate clothing removal, along with first aid by running cool water over the burn for 20 minutes within the first 3 hours of injury, could potentially reduce the severity of scald.
- Frontline medical staff should be aware of the importance of prehospital burn management so that relevant questions can be raised during the initial hospital admission.
Introduction
In Hong Kong, as in most developed countries, one of the
most common types of burn injury that requires
hospital admission is scald. If we view a scald as a
‘contact burns due to a liquid’, the severity of burn
injury will be a function of starting temperature,
contact time, and the thermal capacity of the
causative agent. In a previous study performed in
our centre, it was hypothesised that both viscosity
and thermal capacity of the agent were important
factors in prolonging heat exposure of the skin.1
Patients who were scalded by congee (a popular local
dish where rice with excess water is simmered until a
porridge-like mixture is formed) were more likely to
require surgery than those scalded by hot water (31%
vs 14%, respectively).1 This may be partly explained
by congee’s greater thermal capacity (causing more
effective heat transfer) and viscosity (prolonging
contact time).
In order to minimise the severity of burn
injury, it is essential that effective first-aid measures
be properly taught to the public. The two basic
principles are to stop the burning process and to
cool the burn wound. As patients are usually wearing
clothes and underwear at the time of scalding, the
most effective way to achieve the first objective is to
remove the involved clothing as quickly as possible.
For many reasons, however, this straightforward act
is sometimes not performed in a timely manner (eg
scald occurring in a restaurant where a patron is
too embarrassed to take off his/her clothing or simple
ignorance of first aid). It is in this context that a simple
model was designed in an attempt to demonstrate
the importance of prompt clothing removal after
scalding has occurred.
Methods
In the first part of our study, the effect of delayed
clothing removal on skin temperature was assessed
using our experimental burn model. As in our
centre’s previous study, a piece of Allevyn foam
dressing (Smith & Nephew Medical Limited, Hull,
England) served as our skin model. It was placed on
a metal plate above a heated water bath (JP Selecta,
Barcelona, Spain) until its surface temperature
reached 34°C when measured using the Raytek non-contact
thermometer (Raytek Corporation, Santa
Cruz [CA], US) 1 cm above the centre, in an attempt
to simulate ‘skin temperature’. Cotton underwear
was then placed on top of the Allevyn dressing. The
scalding agents (hot water and congee) were boiled
to 88°C and poured onto the model. The underwear
was then removed at various times following the
‘injury’ (10, 20, 30, 60, and 120 seconds). The
temperature of the Allevyn was immediately
measured at the aforementioned position by the
same observer starting from the moment of clothing
removal and every 10 seconds thereafter for 2
minutes. The same procedure was repeated 3
times for each time interval, and the mean value was
taken as the final data point. Standard cooling curves
were subsequently plotted using these average data
points along with calculated standard deviations.
In the second part, all patients admitted to our
unit via the emergency department with scalding
by congee over a 10-year period (January 2005 to
December 2014) were first retrospectively identified
from our hospital’s computer records. Clinical notes
were physically traced in order to examine the
admission details as well as subsequent management
of the patients.
Results
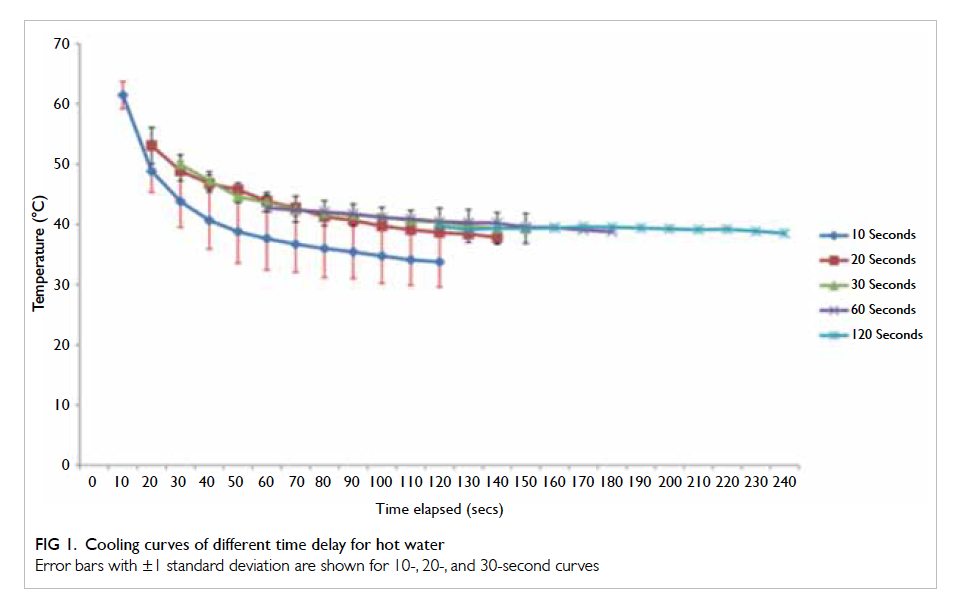
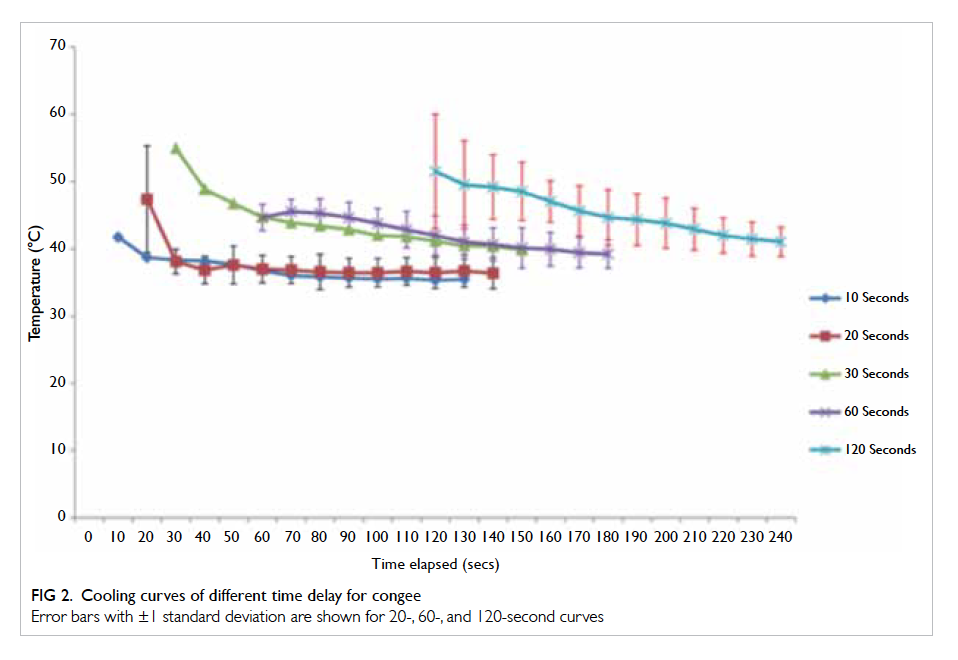
The results of our experimental burn model are shown
in Figures 1 and 2. The temperature of the Allevyn
partly reflected the amount of heat transferred from
the causative agent. A higher cooling curve translated
to a higher skin temperature (hence higher potential
injury). Examination of the cooling curves revealed a
difference in the behaviour of hot water and congee.
With hot water, the 10-second cooling curve was
lower than its counterparts (the 20-, 30-, 60-, and
120-second cooling curves) that essentially lie along
the same curve above. With congee, the cooling
curves appeared to lie progressively higher with
further delay in clothing removal—the 30- and 60-second cooling curves were in a significantly higher
position compared with the 10- and 20-second
cooling curves, while the 120-second cooling curve
was higher than that of 30 and 60 seconds.
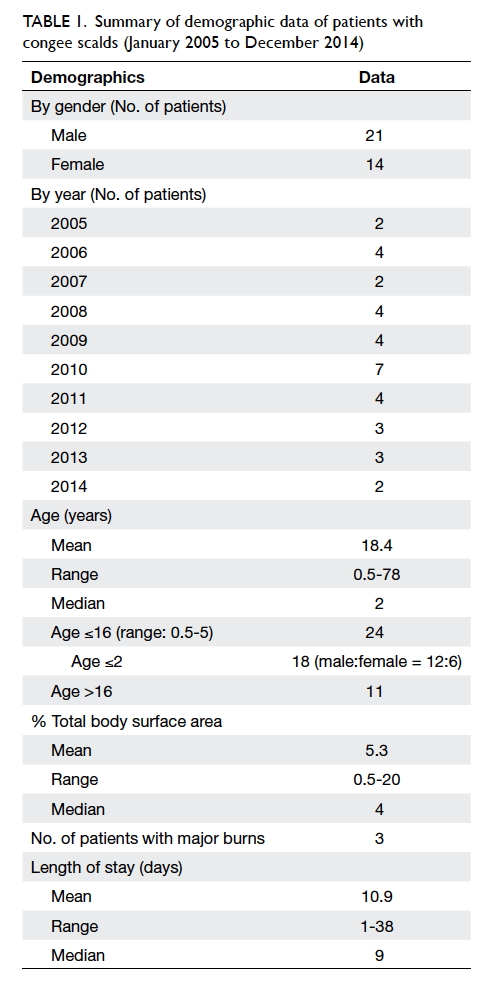
During the study period, 35 patients were
admitted (21 males, 14 females) for scalding by
congee. Of note, two paediatric patients were
admitted to the Intensive Care Unit (ICU) for initial
resuscitation due to the extent of their burns (16%
and 20% of total body surface area [TBSA]) and
one patient was discharged against medical advice
after being admitted for 1 day. The demographic
distribution, percentage of TBSA burnt, and length
of hospital stay are shown in Table 1. On average, our
unit admitted two to four cases per year except in 2010
when there were seven cases. Although most of these
congee scalds were relatively minor as evidenced
by the small mean percentage of TBSA involved and
a mean hospital stay of approximately 11 days,
more than two thirds of patients were children.
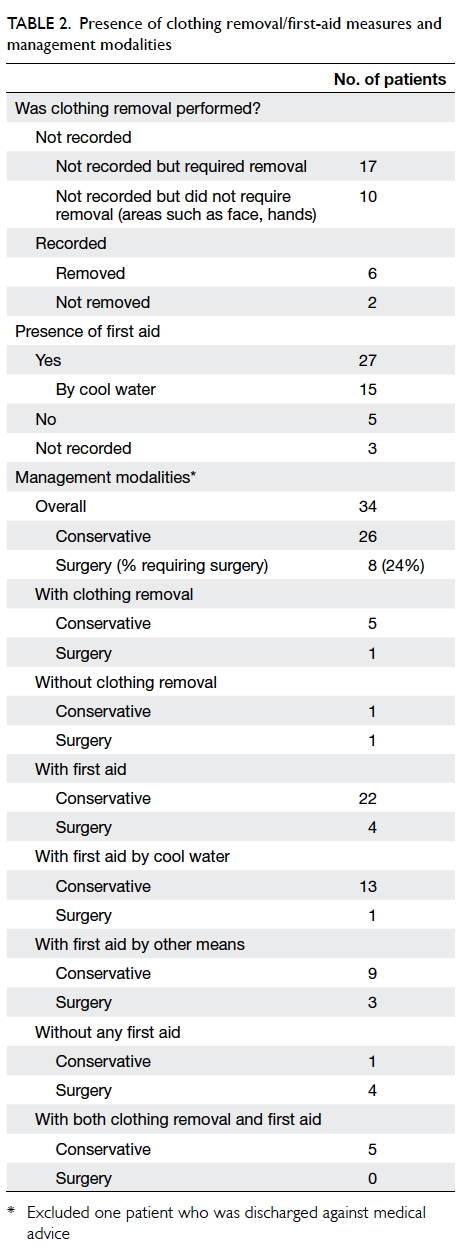
Table 2 shows the statistics for clothing removal/first-aid measures and the subsequent management.
While most of our patients received some form of first aid, it was found that the act of clothing removal was not documented in the majority (27/35) of cases. Despite an extended review period, it is recognised that
the sample size remains small. Consequently, only
descriptive statistics could be shown and a formal
statistical analysis could not be conducted for this
retrospective review. Nonetheless, those patients
who received first aid or in whom clothing was
removed (or both) did seem to fare better than those
without.
Discussion
This was a preliminary study of the potential
relationship between the time of clothing removal
and depth of scald burns. While ‘cooling the burn
wound’ is an important step in the first-aid process,
it must be recognised that ‘stop the burning process’
should take precedence in order to maximise the
benefit of first aid. To this end, the contact time of the
offending agent with the skin should be minimised.
A cooling study was performed by our centre in
2006 to examine the cooling curves of different
food/drinks. Of seven common agents examined
for their rate of cooling, congee cooled significantly
slower compared with the other agents (eg tea,
coffee, noodles, etc).1 It was also shown that a higher
percentage of patients required surgery if scalded
by congee compared with hot water. As congee is a
common dish for children in Hong Kong from which
scalds could lead to greater morbidity, congee was
specifically selected for further investigation.
We showed that delay in clothing removal
could increase the severity of scald burns by congee
as demonstrated by the increased temperature in
our skin model when clothing removal was delayed.
The experiment did not persist beyond a delay of 120
seconds since clothing would generally be removed
within that time or not at all.
Hot water was first examined as a ‘control’
compared with congee. In our results, the cooling
curves of 20, 30, 60, and 120 seconds essentially
lay along the same curvature while the 10-second
cooling curve was significantly lower. This implies
that if clothing removal occurs within the first 10
seconds, the surface temperature of our skin model
would be significantly lower at all subsequent time
points; thus in hot water scalds, immediate clothing
removal may prove to be the most beneficial.
On subsequent examination of the effect of
congee, the cooling curves behaved differently—there appeared to be a stepwise progression from the
10- and 20-second curves to the 30- and 60-second
curves, and then finally to the 120-second curve.
Observation of the error bars showed that the 10- and 20-second curves did not differ significantly and
this also applied to the 30- and 60-second curves.
The 120-second curve generally lay significantly
above the rest; therefore, it appears that delay in
clothing removal significantly affected the surface
temperature of our skin model—removing it within
the first 20 seconds may lead to a less-severe injury
compared with a 30- to 60-second delay, which in
turn is better than a 2-minute delay.
At the time points between 120 and 140 seconds
where all the curves have overlapping temperature
measurements, one is able to observe that there are
three distinct ‘tiers’ (10/20, 30/60, 120 seconds). In
our model, heat was transferred to the Allevyn with
the garment initially acting as a ‘barrier’ since the
underwear was removed before the congee could
soak through, resulting in a lower temperature
detected. By increasing the time interval, the garment
increasingly acted as a ‘reservoir’ for heat as the
congee gradually soaked through. Due to the greater
thermal capacity and viscosity of congee compared
with water, the temperature of the entire ‘congee-underwear-Allevyn complex’ was maintained with
more heat being transferred to the Allevyn for the
same given period, resulting in a higher temperature
detected. Overall, our findings corroborate our
hypothesis that with a viscous agent such as congee,
the severity of scald burns could potentially be
reduced with earlier removal of clothing as evidenced
by lower temperatures detected in our skin model.
Although our experimental study did succeed
in demonstrating effects in our skin model, the ideal
model for this study would be human skin (eg cadaveric
or surgically excised) but it is rather difficult to
source in practice. For the sake of scientific reproducibility,
Allevyn was used instead (a bilayer dressing
material with an outer waterproof layer analogous to
the epidermis along with an inner absorbent sponge
layer). Although Allevyn does not exactly mimic the
‘in-vivo’ behaviour of human skin per se, this model allows the opportunity for comparative
study. Another potential improvement of our model
is to set up a thermometer to measure the skin
model’s temperature underneath the surface so that
temperature can be tracked while clothing is still in
place. In this experimental model, we were only able
to measure the temperature after the garment was
removed. Having continual temperature monitoring
would enable us to plot ‘complete’ curves starting
from 0 second onwards for all five time intervals,
and the temperature change both before and after
clothing removal could be more accurately depicted.
In an early study by Moritz and Henriques,2 porcine
skin was found to bear a remarkable resemblance
to human skin. If the experiment can be repeated
with porcine skin along with improved accuracy
of temperature measurement (ie setting up a
thermometer intradermally within the porcine skin),
the validity of our conclusions may be strengthened.
Nonetheless, this experimental study lends support
to the notion that timely clothing removal before
first-aid application may reduce the severity of burn
injury.
The paediatric population (especially those
under the age of 2 years) is particularly susceptible to
scalds with a male preponderance.3 4 5 This age-group is
particularly vulnerable as it is an age of great curiosity
about the environment (hence the tendency to grab/tip over things) but limited motor development does
not allow a child to move away from danger, such as
a falling bowl of congee. It is also compounded by the
fact that children have relatively thinner skin and this
results in more significant injuries. Our statistics from
this congee scald review do not deviate much from
our centre’s previous experience: slightly over 50% of
our patients were aged 2 years or younger with a male
predominance, and 24 out of 35 patients were within
the paediatric age-group.
It seems almost intuitive that clothing should
be removed as soon as possible whenever a scald
burn is sustained. This may not necessarily be so. In
a recent UK study where parents were interviewed
and asked about first-aid measures they would
provide for a child with a large scald, 61% of parents
failed to state that clothes should be stripped
and several thought that it would cause further
skin damage.6 The question of whether removing clothing would cause further skin damage is commonly asked by parents of paediatric
burn patients admitted to our unit.
In our retrospective review, analysis of the
efficacy of clothing removal was hindered because
such action was not recorded in the majority of cases
(27 out of 35). The location of burns was further
studied: in 10 of these 27 cases, injury occurred over
an exposed area (eg face and hands), while the
remaining 17 cases could have benefited from clothing
removal. In six of eight patients where clothing was
removed, the exact timing was not documented.
Such lack of documentation demonstrates the benefit
of education about prehospital treatment for both
the public and frontline medical staff. An increased
awareness of correct prehospital treatment of burns
would mean relevant questions are asked during
history taking, and this would facilitate proper documentation
and subsequent patient management. As mentioned
in the Results section, our sample size did not
permit any meaningful statistical analysis to be
carried out pertaining to the potential usefulness of
early clothing removal in reducing morbidity from
scalds. Nonetheless, it appeared that those patients
who had clothing removed fared quite well. One
exception was a 50-year-old man with a relatively
larger scald (TBSA, 13%) involving the face/neck/chest/bilateral upper limbs who eventually required
skin grafting.
After the burning process is stopped, the next
logical step is to cool the burn by applying first
aid. Ideally, first aid for burns should provide pain
relief and reduce potential morbidity associated
with the injury. Although many first-aid treatments
to cool burns have been studied, the application of
cold water has the strongest supporting evidence.
Currently, an ‘adequate’ first aid is defined as 20
minutes of running tap water over the burn within
the first 3 hours of injury.7 Apart from removing
heat energy from the damaged tissue, the benefits
of cooling continue and include decreased oedema
formation, preservation of dermal perfusion,
decreased inflammatory response, and improved
wound healing.8 9 Regrettably, our centre’s previously published paper showed that first aid was applied
only to half of our paediatric patients.5 In our current
review, although 27 patients received some form of
first aid, only 15 (43%) patients received cool-water
treatment of variable duration. The duration of first
aid with cool water was either not recorded or fell
short of the recommended 20 minutes. This state of
affairs is certainly unsatisfactory and more public
education is warranted.
Our data once again do not enable formal
statistical analysis, and a number of factors such
as percentage of TBSA burnt and depth of burn would affect
the eventual outcome of our patients. Nonetheless,
it does appear that those who received first aid
required fewer surgeries. Detailed analysis of those
who received no first aid revealed that none of the
burns was classified as major even though four out
of eight patients underwent skin grafting. In patients
who received cool water as first aid, only one needed
surgery—a 14-month-old boy with a TBSA of 13.5%
burnt involving the left flank and bilateral lower
limbs. In patients who received other types of first
aid, three required surgeries (one of whom had a
major burn and required ICU admission). Of note, for
patients in whom clothing was removed and first-aid
measures applied, all were managed conservatively.
Although definite conclusions from our data cannot
be drawn, clothing removal and first aid do seem to
have beneficial effects, especially in smaller burns
that constitute most of our case load. It is our
hope that with better medical documentation and
education of our frontline staff, the quality of our
future data can be enhanced with a view to facilitate
formal data analysis.
Before a simple and effective message can be
delivered to the public about post-burn prehospital
management, it is equally important to consider
the local food characteristics. For instance, the
population of Hong Kong may find it easier to relate
burns to congee or cup noodle than burns to coffee.
Since half of our paediatric burn patients received
no first aid upon admission, simply emphasising
the importance of ‘stop the burning process’ may
reduce potential morbidity. Our experimental skin
model showed that earlier clothing removal post-burn
reduces skin temperature and thus beneficial.
Although our retrospective review was unable
to reflect any concrete statistical results, it was
certainly suggestive of the potential usefulness of
proper prehospital management. Last but not least,
the financial cost of managing acute uncomplicated
minor paediatric scalds is significant (including
hospital beds, theatre visits, dressings, medications
etc). This is an important social and economic issue
since burns sustained by children often require
many years of follow-up for scar management and
psychosocial support.10 If preventive measures fail
and accidents occur, it is in the best interests of the
public to understand how to minimise morbidity.
References
1. Chiu TW, Ng DC, Burd A. Properties of matter matter in
assessment of scald injuries. Burns 2007;33:185-8. Crossref
2. Moritz AR, Henriques FC. Studies of thermal injury: II. The
relative importance of time and surface temperature in the
causation of cutaneous burns. Am J Pathol 1947;23:695-720.
3. Ray JG. Burns in young children: a study of the mechanism
of burns in children aged 5 years and under in the Hamilton,
Ontario Burn Unit. Burns 1995;21:463-6. Crossref
4. Dewar DJ, Magson CL, Fraser JF, Crighton L, Kimble RM.
Hot beverage scalds in Australian children. J Burn Care
Rehabil 2004;25:224-7. Crossref
5. Tse T, Poon CH, Tse KH, Tsui TK, Ayyappan T, Burd A.
Paediatric burn prevention: an epidemiological approach.
Burns 2006;32:229-34. Crossref
6. Graham HE, Bache SE, Muthayya P, Baker J, Ralston DR.
Are parents in the UK equipped to provide adequate burns
first aid? Burns 2012;38:438-43. Crossref
7. First aid. Australian and New Zealand Burn Association.
Available from: http://anzba.org.au/care/first-aid/.
Accessed Feb 2016.
8. Cuttle L, Pearn J, McMillan JR, Kimble RM. A review of
first aid treatments for burn injuries. Burns 2009;35:768-75. Crossref
9. Wright EH, Harris AL, Furniss D. Cooling of burns:
mechanisms and models. Burns 2015;41:882-9. Crossref
10. Griffiths HR, Thornton KL, Clements CM, Burge TS,
Kay AR, Young AE. The cost of a hot drink scald. Burns
2006;32:372-4. Crossref