Hong Kong Med J 2016 Feb;22(1):16–22 | Epub 18 Dec 2015
DOI: 10.12809/hkmj154451
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Assessment of postoperative short-term and long-term mortality risk in Chinese geriatric patients for hip fracture using the Charlson comorbidity score
TW Lau, FRCS (Edin), FHKAM (Orthopaedic Surgery);
Christian Fang, FRCS (Edin), FHKAM (Orthopaedic Surgery);
Frankie Leung, FRCS (Edin), FHKAM (Orthopaedic Surgery)
Department of Orthopaedics and Traumatology, The University of Hong
Kong, Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr TW Lau (catcherlau@hku.hk)
Abstract
Introduction: The clinical outcome of geriatric
patients with hip fracture depends on surgical
management as well as other medical factors. This
study aimed to evaluate the relationship between
Charlson comorbidity score and in-patient, 30-day,
and 1-year mortality in Chinese geriatric patients
who underwent surgery for hip fracture.
Methods: This was a historical cohort study
conducted in a tertiary trauma referral centre in Hong
Kong. From 1 January 2009 to 31 December 2010,
759 operated hip fracture patients who were over
65 years were recruited. The Charlson Comorbidity
Index of each patient was retrieved from their
medical records. The total Charlson comorbidity
score, the highest Charlson comorbidity score, and
the Charlson comorbidity score were calculated. The
associations between these scores and in-patient,
30-day, and 1-year mortality were examined using
Mann-Whitney U test and Cox regression model.
Results: The mean in-patient, 30-day, and 1-year
mortality rate was 0.8%, 2.5%, and 16.3%, respectively.
The total Charlson comorbidity score was
significantly associated with in-patient mortality
(P=0.031). The total Charlson comorbidity score
(P<0.001) and Charlson comorbidity score (P=0.010)
were significantly associated with 30-day mortality.
All three scores were also significantly related
to 1-year mortality (P<0.001). A Cox regression
model demonstrated the relationship between total
Charlson comorbidity score and 30-day and 1-year
mortality. This can help predict 30-day and 1-year
mortality risk in geriatric patients admitted for hip
fracture surgery.
Conclusion: The Charlson comorbidity score
provides a good preoperative indicator of 30-day
and 1-year mortality in geriatric patients with hip
fracture.
New knowledge added by this study
- Charlson comorbidity score correlates well with the short-term and long-term mortality of Chinese geriatric patients with operated hip fracture.
- Hip fracture surgery is generally safe in terms of short-term mortality rate even in high-risk patients.
- Preoperative assessment of geriatric patients admitted with hip fracture can provide a reasonably accurate indication of mortality risk. This helps improve patient and family rapport and subsequent satisfaction.
Introduction
The number of geriatric patients admitted to our
hospital with hip fracture has been increasing
steadily over the last decade. Such osteoporotic
fractures are difficult to treat because of poor bone
quality. The often extreme age of the patients and
other comorbidities make the management of such
patients even more challenging. The clinical outcome
of geriatric patients with hip fracture depends on
surgical management as well as many other medical
factors.
Hip fracture is a significant cause of mortality.1
Haentjens et al2 reported a 5- to 8-fold increased
risk for all-cause mortality in the first 3 months
following hip fracture. Some clinical scores and
assessments—for example, the American Society
of Anesthesiologists (ASA) classification, the
Barthel index, the Goldman index, the POSSUM
(Physiological and Operative Severity Score for the
enumeration of Mortality and Morbidity) scoring
system, the Charlson index and the visual analogue
scale for risk scale, or the cumulated ambulation
score—are reported to correlate with postoperative
complications and mortality of hip fracture.3 4 5
Some of these scores can predict complication rates
and others better predict short-term mortality.4 6 Individual clinical parameters also correlate with
mortality rates.6 7 8 9 10 11
Among all these scores, the Nottingham Hip
Fracture Score (NHFS) is one of the most well-known
for the prediction of short- and long-term mortality
in geriatric hip fracture patients, and has been
validated in both western and Asian populations.12 13 14 This excellent score includes patient age, sex,
admission haemoglobin level, Mini-Mental State
Examination (MMSE) score, previous institution,
number of comorbidities, and also presence of
malignancy.
In our hospital, a multidisciplinary hip fracture
clinical pathway programme was started in 2007.
The implementation of this pathway has not only
shortened hospital stay, but also improved clinical
outcomes, including pressure sore rate, infection
rate, and mortality rate.15 To enable early patient
assessment and quantification of the risks of hip
fracture surgery, a score that is easy to calculate
and readily obtainable should be identified. This can
greatly improve the rapport between the surgeon
and patient, as well as their family, with regard to
the operative risks and mortality risks. The NHFS
is an excellent score that has been widely validated.
Nonetheless it involves assessment of the MMSE
score by a therapist and is not always possible
before surgery. In this retrospective study, we used
the Charlson Comorbidity Index (CCI) to evaluate
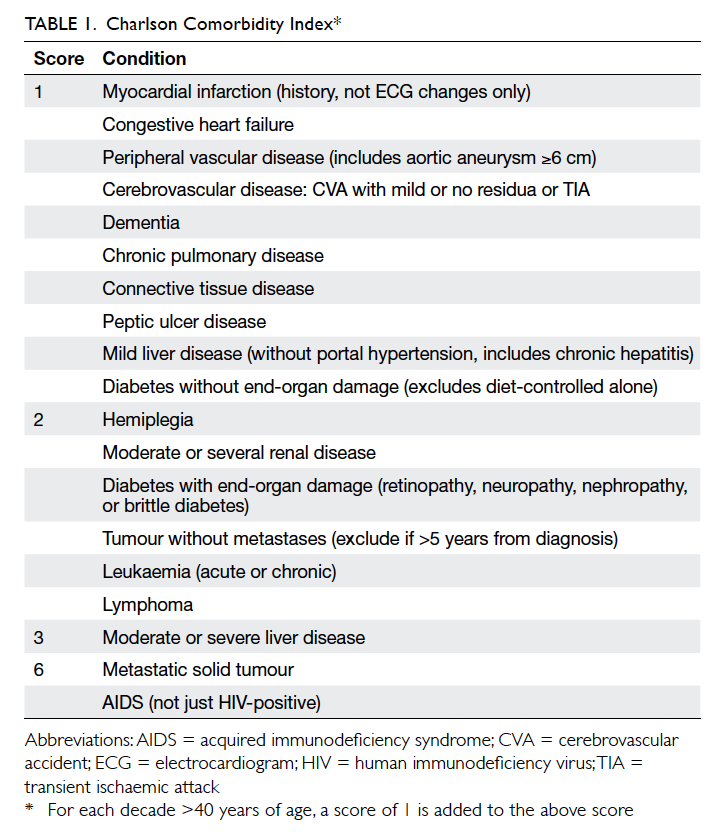
patient comorbidities (Table 1).
The objective of this study was to determine
the association of the CCI in operated hip fracture
in patients older than 65 years with the in-patient,
30-day, and 1-year mortality.
Methods
Our hospital is a tertiary trauma referral centre
in Hong Kong. When geriatric patients with hip
fracture present to the accident and emergency
department, they are transferred to the orthopaedic
ward for preoperative workup and assessment once
they are stabilised. Surgery is performed within 2
days. Postoperatively, they are observed in an acute
ward for a mean of 5 days before being transferred
to another convalescence hospital for rehabilitation.
Patients are discharged after a mean of 3 weeks.
From 1 January 2009 to 31 December 2010,
we recruited all patients aged over 65 years who
underwent surgery for geriatric hip fracture.
Patients with pathological fractures, multiple
fractures, or old fractures were excluded from
this study. Patient records were retrieved from the
electronic medical record system. Since all these
patients were managed according to our hip fracture
clinical pathway protocol, all demographic data, premorbid
walking status, comorbidities, past surgery,
complications, and also length of stay in both acute
and convalescence hospitals were available. Most
importantly, the in-patient, 30-day, and 1-year
mortality rates could be traced. In-patient mortality
was defined as death that occurred in the acute or
convalescence hospital, and the 30-day and 1-year
mortality was defined as death occurring within 30
days and 1 year of admission, respectively. Mortality
records are available when death occurs in any public
hospital in Hong Kong with an electronic medical
record system.
The CCI was calculated from the medical
records of patients admitted with hip fracture
obtained from the hospital electronic medical
system. The clinical history of patients was reviewed by
medical officers with comorbidities recorded.
The final patient outcome was not known to the
medical officers unless it was recorded in the same
medical records. Using the CCI, three scores can be
calculated—the total Charlson comorbidity score
(TCCS) is the sum of all comorbidities combined
with the score derived from the patient’s age; the
highest Charlson comorbidity score (HCCS) is the
highest single comorbidity score of a patient; and the
Charlson comorbidity score (CCS) is the sum of all
comorbidity scores without consideration of age. All
these scores were used to analyse and correlate with
different mortality rates.
The independent sample Mann-Whitney U
test was used to test the statistical association of
different comorbidity scores and mortality rates.
Receiver operating characteristic (ROC) curve was
used to measure the best cut-off for the score with
respect to different mortality rates. Multiple variant
analysis using Cox regression model was employed
to measure the survival rate of hip fracture patients
with respect to the cut-off scores derived from
the ROC curves. Age, sex, fracture sites, and the
Charlson scores were the independent variables. This
regression model can be used as a means to predict
patient mortality rate before surgery is performed.
Results
During the 2-year period, we performed surgery
on 759 geriatric patients with acute hip fracture.
Among them, 28% were male and 72% were female.
The mean age was 84 years: 25% aged from 70 to 79
years, 50% aged from 80 to 89 years, and 21% aged
from 90 to 99 years. The oldest patient operated on
was 102 years old. Overall, 72% of patients lived at
home before the admission, and the remainder in
a home for the elderly. With regard to premorbid
mobility, 36% of them could walk unaided and 56%
could walk with some form of aid such as a stick or
walking frame.
With regard to the comorbidities, the
three most common diseases were hypertension,
diabetes mellitus, and dementia. Mini-Mental State
Examination was used to evaluate the patients’ mental
function and revealed that 65% were considered
severely or moderately demented. Premorbid
functional status was assessed by the modified
Barthel index: 40% of patients were independent,
42% were mildly and moderately dependent, and
18% were severely or totally dependent in their daily
function. The ASA score was also documented: 2.5%
were ASA 1 (with normal health), 38% were ASA
2 (with mild systemic disease), and 58% were ASA
3 (with severe systemic disease). When the type of
fracture was analysed, 49% were at the femoral neck
and 49% the trochanter. The remaining 2% were
subtrochanteric fractures. Internal fixation was
performed in 75%. Among this group of internally
fixed hip fractures, 24% of them were impacted
fractured neck of femur that was fixed by screws
only. The remaining 76% were fixed by either an
extramedullary or intramedullary device for the
pertrochanteric fractures. The remaining 25% of
fractures were displaced fractured neck of femur,
managed by hemiarthroplasty. Postoperatively, 72%
of patients did not require a blood transfusion. The
mean preoperative waiting time was 1.44 days. The
longest waiting time was 14 days due to unstable
medical conditions. The mean total length of stay in
both acute and convalescence hospitals was 26.6 days.
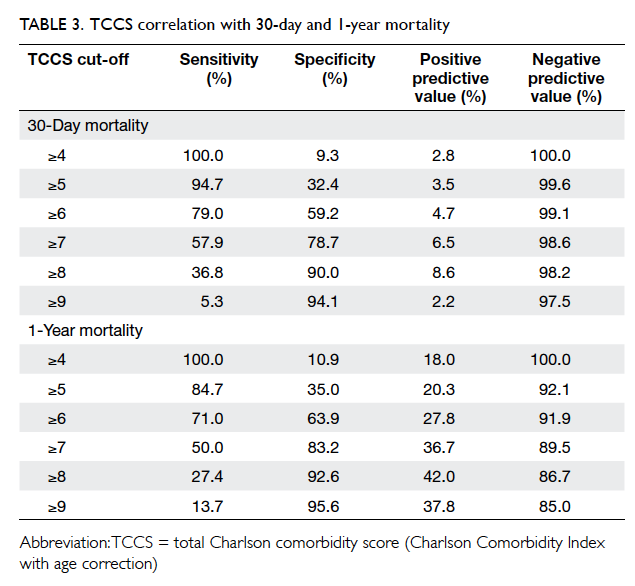
The statistical analysis of the difference in
mortality rates compared with the difference scores
is summarised in Table 2. Among these 759 operated
patients, six died in the hospital. The in-patient
mortality rate was 0.8%. Within 30 days of admission,
19 patients died. The 30-day mortality rate was
2.5%. In 1-year time, 124 patients died. The 1-year
mortality rate was 16.3%. Mann-Whitney analysis
showed that the in-patient mortality was significantly
related to the TCCS (P=0.031). Regarding the 30-day
mortality rate, statistical analysis showed that it was
significantly related to TCCS (P<0.001) and CCS (P=0.010).
Using Spearman’s rank correlation coefficient, the
TCCS was statistically correlated with HCCS and
CCS. All three different scores derived from the CCI
were significantly related to this 1-year mortality
rate (P<0.001; Table 2).
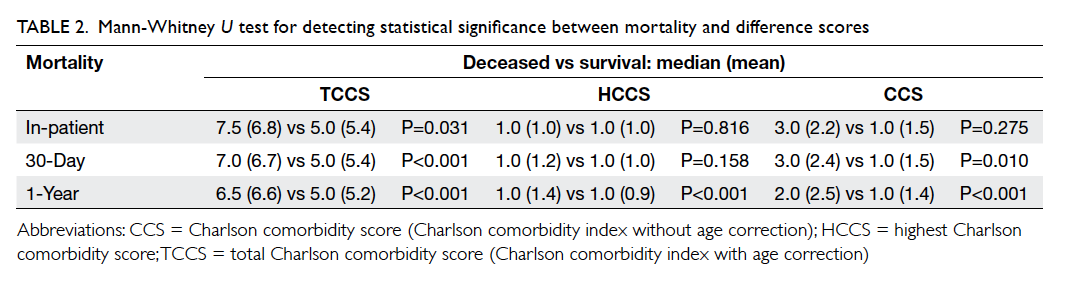
Table 2. Mann-Whitney U test for detecting statistical significance between mortality and difference scores
An ROC curve analysis was used to identify
the relationship between TCCS and mortality rates.
Both 30-day mortality and 1-year mortality rates
were analysed using MedCalc software (MedCalc
Software, Ostend, Belgium). Both ROC findings
were significant for 30-day and 1-year mortality
(area under the curve=0.72 and 0.75 respectively,
P<0.001). In both situations, the best cut-off value
was a TCCS of ≥6 according to the Youden
index method, with 30-day mortality (sensitivity 79%,
specificity 59%, positive predictive value [PPV] 4.7%,
and negative predictive value [NPV] 99%) and 1-year
mortality (sensitivity 71%, specificity 64%, PPV 28%,
and NPV 92%). Nonetheless when referring to the
actual curve (Fig 1), this optimal cut-off point was
not well-defined versus using the adjacent higher
cut-off value of TCCS of ≥7.
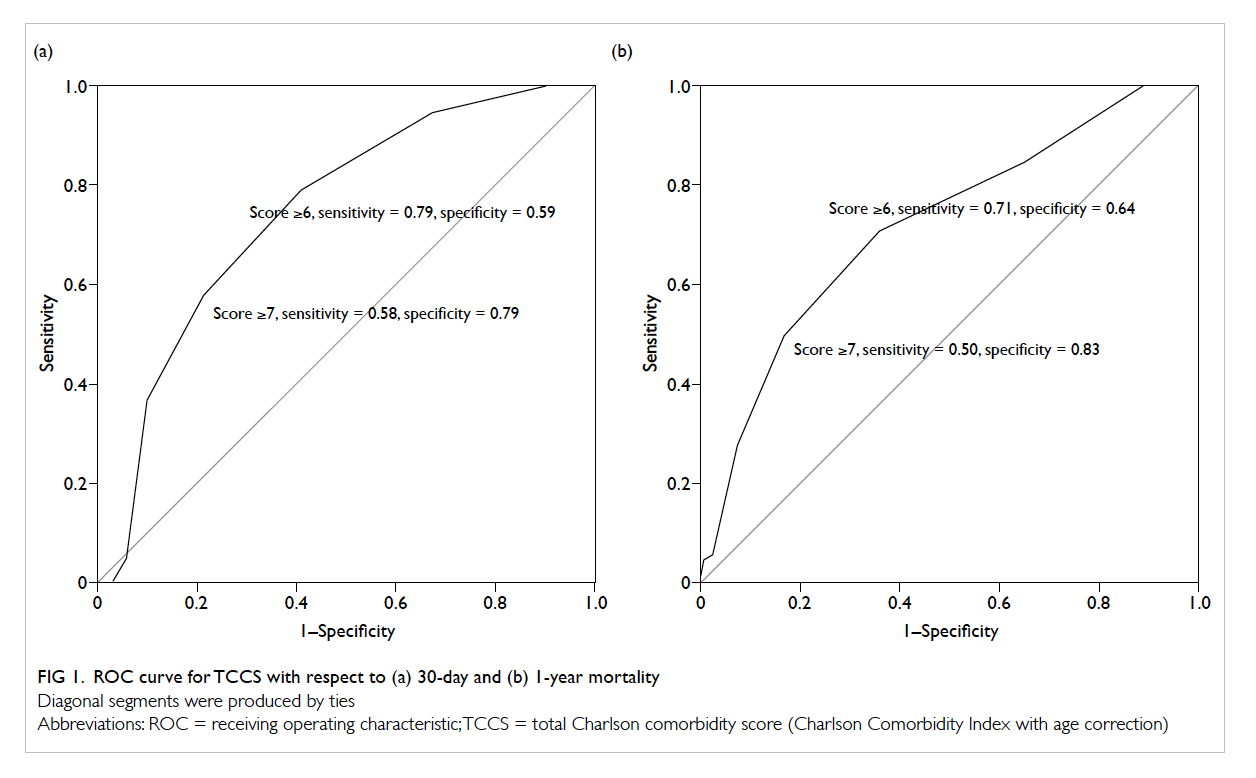
Figure 1. ROC curve for TCCS with respect to (a) 30-day and (b) 1-year mortality
Diagonal segments were produced by ties
If a TCCS cut-off value of ≥7 was used, the
respective value of sensitivity, specificity, PPV,
and NPV was 58%, 79%, 6.5%, and 99% for 30-day
mortality, and 50%, 83%, 37%, and 90% for 1-year
mortality. In a clinical situation, better specificity is
preferred for predicting mortality. Thus we elected
to use a 3-tier stratification of patients based on their
TCCS in the regression analysis—low-risk group:
TCCS 0-5, borderline group: TCCS 6-7, high-risk
group: TCCS ≥8. These values are shown in Table 3.
Cox regression model was used to demonstrate
the relationship between mortality rates by using the
TCCS as the predictor (Fig 2). Using a score of ≤5
(low-risk group) as baseline, when score was equal
to 6 or 7 (borderline group), the 30-day and 1-year
mortality hazard ratio (HR) was 3.41 (95% confidence
interval [CI], 0.88-13.19; P=0.075) and 2.66 (95% CI,
1.71-4.10; P<0.001), respectively. If the score was ≥8
(high-risk group), the 30-day mortality and 1-year
mortality HR was 7.93 (95% CI, 1.93-32.54; P=0.004)
and 5.08 (95% CI, 3.06-8.42; P<0.001), respectively.
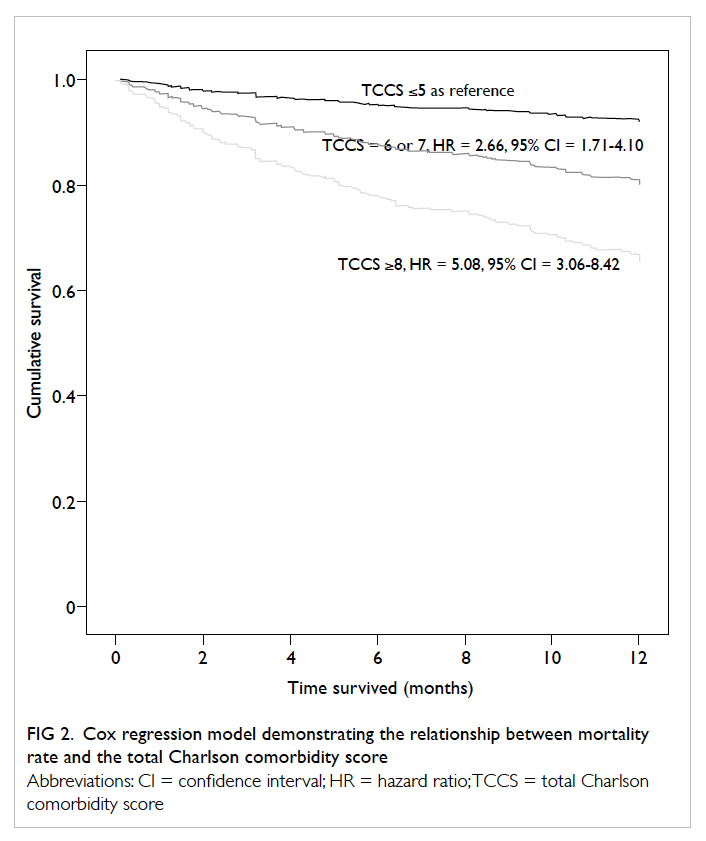
Figure 2. Cox regression model demonstrating the relationship between mortality rate and the total Charlson comorbidity score
The logistic regression model revealed that the
30-day mortality rate correlated with the TCCS in a
good exponential relationship (Fig 3a). If the graph
was analysed in more detail, it would show that
operating on the hip fractures was generally safe.
Even when the TCCS reached 9 points, the 30-day
mortality rate remained <5%.
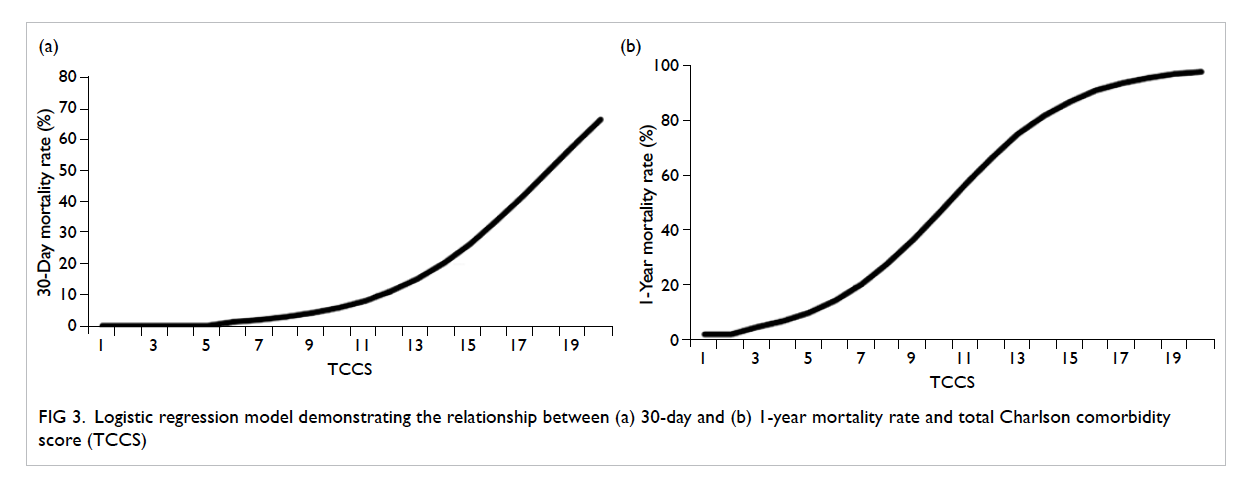
Figure 3. Logistic regression model demonstrating the relationship between (a) 30-day and (b) 1-year mortality rate and total Charlson comorbidity score (TCCS)
The 1-year mortality rate showed a different
correlation with TCCS. The curve became more
linear in shape (Fig 3b). When TCCS was <3, 1-year morality rate remained <5%. When the TCCS was >5,
mortality rate rose almost linearly with the TCCS.
When the TCCS was ≤10, 1-year mortality rate was
approximately 50%. The increase in mortality rate
appeared to plateau at TCCS of >15, where it reached
88%. An overview of our hip fracture patients reveals
that there was a reasonable 1-year survival with only
10% 1-year mortality rate after hip fracture surgery if the
TCCS was <5.
Discussion
In the last two decades, there has been an increasing
attention on geriatric fragility fractures with a
special focus on hip fractures.6 Many parameters
are significant predictors of associated clinical
outcome and mortality. These include type of
injury and surgery,7 postoperative delirium,8 timing of rehabilitation,9 and surgical technique.10 11 In
addition, many other preoperative indicators
have been found to affect postoperative mortality.
The most commonly identified factors include
advanced age,16 17 18 male gender,16 18 19 poor premorbid functional capability,18 20 and presence of multiple
comorbidities.21 22
The CCI is a system that allows classification
of severity and uses recorded secondary diagnoses to
assign a weight to morbidity, thereby generating the
patient’s risk of death.23 This score can be combined
with age to form a single index. This is particularly
useful in our geriatric hip fracture patient group
because our patients’ age ranged from 65 to 102
years, which is a major factor in their mortality rates.
We have shown that the TCCS correlates well
with both short-term and long-term mortality. The
TCCS includes all the comorbidities and the age
of the patient and reflects the general health of the
patient on admission to hospital. Thus the poorer
the general health is, the higher the short-term
mortality rate will be. As most of these patients
require surgery to either fix or replace the fractured
hip, there is additional stress on their physiologically
compromised body. Although many of the common
comorbidities of geriatric hip fracture patients are
minor problems, such as diabetes, hypertension, or
previous cerebrovascular accident, these problems
are nonetheless chronic diseases that lead to gradual
multi-organ dysfunction and deterioration. The
most commonly affected organs are the lungs,
heart, general vascular system, kidneys, and brain.
Surgery poses a major stress challenge to these
diseased organs and can result in a rapid decline
in general health. Therefore the severity of a
patient’s comorbidities has a significant prognostic
implication for short-term mortality post-surgery.
This explains why the TCCS correlates significantly
with the in-patient and 30-day mortality rates.
Using the logistic regression graph correlating
the TCCS and 30-day mortality rate, different TCCSs
correspond to an estimated 30-day mortality rate.
This is valuable information when frontline staff are
required to explain the risks to the newly admitted
patient and their family. Many patients and their
family are concerned about the impending need for
surgery, believing that surgery will lead to death of
their loved one who already has multiple existing
comorbidities. With the information available, we
can reassure the patient about their low mortality
risk, despite these multiple comorbidities. Informed
discussion between the patient, their family, and the
surgeon can allay fears about surgery and allow extra
effort and care during the postoperative period.
A more experienced surgeon and staff should be
involved in care to minimise surgical trauma and the
possibility of surgical complications. Geriatricians
and anaesthetists should be informed about the
higher incidence of major life-threatening conditions
during the pre-, peri-, and post-operative period. This
allows better utilisation and coordination of limited
medical and human resources such as intensive
care unit beds, sophisticated preoperative and
postoperative monitoring machines, and specialist
nursing care.
Analysis of the 1-year mortality rate revealed
a statistically significant correlation with all scores,
similar to another study.24 This is to be expected as
the 1-year mortality relates more to general physical
health and age, and not the hip fracture. The CCI
independently predicts both short- and long-term
mortality in acutely ill hospitalised elderly adults.25 In
our series, the 1-year mortality rate was 16.3%, slightly
lower than some studies17 but not uncommon.24 This may be partly due to the general health status of our
population and may be partly due to differences in
the medical system.
Information about short- and long-term
mortality can help reassure the patient and their
family and allay their fears about surgery in the
presence of other comorbidities. It can alleviate
some of the stress associated with uncertainty.
This study is not without limitations. There is
a possible discrepancy between the actual number
of deaths because a small number may have
occurred outside of the public hospital system. As
a retrospective study, we were not able to control
the confounding factors that could influence the
results. Although age, sex, and fracture sites were
accounted in the regression model, other factors
such as smoking, medications, fracture sites,
surgeon experience, and surgical procedure were not
included in the analysis. Possible errors in coding
and rating of CCI also exist. There might also have bias in data collection for the comorbidity
index if patient mortality was known during the
data collection process. Nonetheless based on our
results in this retrospective cohort, a prospective
study should be conducted to further analyse the
relationship between comorbidity and mortality of
the geriatric patients with hip fracture.
Furthermore, non-operated hip fracture patients were not included in this study. During the
study period, 15 hip fracture patients were treated
conservatively. The most common reasons for non-operative
treatment were being unfit for surgery or
refusal of surgery by family. The 30-day mortality
rate was 13.3%. The 1-year mortality rate was
20%. Both the short-term and long-term mortality
rates of these non-operated patients were generally
higher than that of operated patients. However,
since the number of deaths was small, a statistical
comparison was not performed. Interpretation of the
data should also be cautious because non-operated
patients are usually very fragile with pre-existing
life-threatening medical conditions. These patients
may have had a very high short-term mortality rate if
surgery were performed that would have influenced
the final statistical analysis. Nevertheless the small
proportion of non-operated hip fracture patients
would not have been expected to have a large effect
on overall results.
Conclusion
In this retrospective study of the short- and long-term
mortality rates of geriatric patients undergoing
surgery for hip fracture, scores derived from the
CCI correlated well with mortality rates. Use of CCI
before surgery to assess the patients’ general health
and operative risks can aid communication between
the patient and doctors, and assist in deciding the
best treatment option.
References
1. Frost SA, Nguyen ND, Center JR, Eisman JA, Nguyen TV.
Excess mortality attributable to hip-fracture: a relative
survival analysis. Bone 2013;56:23-9. Crossref
2. Haentjens P, Magaziner J, Colón-Emeric CS, et al. Meta-analysis:
excess mortality after hip fracture among older
women and men. Ann Intern Med 2010;152:380-90. Crossref
3. Burgos E, Gómez-Arnau JI, Díez R, Muñoz L, Fernández-Guisasola J, Garcia del Valle S. Predictive value of six risk
scores for outcome after surgical repair of hip fracture in
elderly patients. Acta Anaesthesiol Scand 2008;52:125-31. Crossref
4. Foss NB, Kristensen MT, Kehlet H. Prediction of
postoperative morbidity, mortality and rehabilitation in
hip fracture patients: the cumulated ambulation score. Clin
Rehabil 2006;20:701-8. Crossref
5. Kirkland LL, Kashiwagi DT, Burton MC, Cha S, Varkey P.
The Charlson Comorbidity Index Score as a predictor of
30-day mortality after hip fracture surgery. Am J Med Qual
2011;26:461-7. Crossref
6. Smith T, Pelpola K, Ball M, Ong A, Myint PK. Preoperative
indicators for mortality following hip fracture
surgery: a systematic review and meta-analysis. Age
Ageing 2014;43:464-71. Crossref
7. Smith EB, Parvizi J, Purtill JJ. Delayed surgery for patients
with femur and hip fractures—risk of deep venous
thrombosis. J Trauma 2011;70:E113-6. Crossref
8. Lee HB, Mears SC, Rosenberg PB, Leoutsakos JM,
Gottschalk A, Sieber FE. Predisposing factors for
postoperative delirium after hip fracture repair in
individuals with and without dementia. J Am Geriatr Soc
2011;59:2306-13. Crossref
9. Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E,
Morrison RS. Early ambulation after hip fracture: effects
on function and mortality. Arch Intern Med 2006;166:766-71. Crossref
10. Cheng T, Zhang GY, Liu T, Zhang XL. A meta-analysis of
percutaneous compression plate versus sliding hip screw
for the management of intertrochanteric fractures of the
hip. J Trauma Acute Care Surg 2012;72:1435-43. Crossref
11. Cho SH, Lee SH, Cho HL, Ku JH, Choi JH, Lee AJ.
Additional fixations for sliding hip screws in treating
unstable pertrochanteric femoral fractures (AO Type
31-A2): short-term clinical results. Clin Orthop Surg
2011;3:107-13. Crossref
12. Maxwell MJ, Moran CG, Moppett IK. Development and
validation of a preoperative scoring system to predict 30
day mortality in patients undergoing hip fracture surgery.
Br J Anaesth 2008;101:511-7. Crossref
13. Wiles MD, Moran CG, Sahota O, Moppett IK. Nottingham
Hip Fracture Score as a predictor of one year mortality in
patients undergoing surgical repair of fractured neck of
femur. Br J Anaesth 2011;106:501-4. Crossref
14. Kau CY, Kwek EB. Can preoperative scoring systems be
applied to Asian hip fracture populations? Validation
of the Nottingham Hip Fracture Score (NHFS) and
identification of preoperative risk factors in hip fractures.
Ann Acad Med Singapore 2014;43:448-53.
15. Lau TW, Fang C, Leung F. The effectiveness of a geriatric
hip fracture clinical pathway in reducing hospital and
rehabilitation length of stay and improving short-term
mortality rates. Geriatr Orthop Surg Rehabil 2013;4:3-9. Crossref
16. Holt G, Smith R, Duncan K, Hutchison JD, Gregori A.
Gender differences in epidemiology and outcome after hip
fracture: evidence from the Scottish Hip Fracture Audit. J
Bone Joint Surg Br 2008;90:480-3. Crossref
17. Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B.
Excess mortality in men compared with women following
a hip fracture. National analysis of comedications,
comorbidity and survival. Age Ageing 2010;39:203-9. Crossref
18. Jamal Sepah Y, Umer M, Khan A, Ullah Khan Niazi
A. Functional outcome, mortality and in-hospital
complications of operative treatment in elderly patients
with hip fractures in the developing world. Int Orthop
2010;34:431-5. Crossref
19. Endo Y, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ.
Gender differences in patients with hip fracture: a greater
risk of morbidity and mortality in men. J Orthop Trauma
2005;19:29-35. Crossref
20. Williams A, Jester R. Delayed surgical fixation of fractured
hips in older people: impact on mortality. J Adv Nurs
2005;52:63-9. Crossref
21. Franzo A, Francescutti C, Simon G. Risk factors correlated
with post-operative mortality for hip fracture surgery in
the elderly: a population-based approach. Eur J Epidemiol
2005;20:985-91. Crossref
22. Hannan EL, Magaziner J, Wang JJ, et al. Mortality and
locomotion 6 months after hospitalization for hip fracture:
risk factors and risk-adjusted hospital outcomes. JAMA
2001;285:2736-42. Crossref
23. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A
new method of classifying prognostic comorbidity in
longitudinal studies: development and validation. J Chronic
Dis 1987;40:373-83. Crossref
24. Svensson O, Strömberg L, Ohlén G, Lindgren U. Prediction
of the outcome after hip fracture in elderly patients. J Bone
Joint Surg Br 1996;78:115-8.
25. Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, van
Munster BC, de Rooij SE. Validation of the Charlson
Comorbidity Index in acutely hospitalized elderly adults: a
prospective cohort study. J Am Geriatr Soc 2014;62:342-6. Crossref