Hong Kong Med J 2015 Dec;21(6):573.e1–2
DOI: 10.12809/hkmj154585
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Phlebosclerotic colitis: radiological findings of an uncommon entity
HY Chan, FHKCEM, FHKAM (Emergency Medicine);
MN Chan, MB, BS;
F Ng, FHKCEM, FHKAM (Emergency Medicine);
WT Ho, FHKCEM, FHKAM (Emergency Medicine)
Accident and Emergency Department, Caritas Medical Centre, Shamshuipo, Hong Kong
Corresponding author: Dr HY Chan (chanhy1@ha.org.hk)
A 46-year-old Chinese woman attended our accident
and emergency department because of abdominal
pain, no bowel movements, and vomiting for 10 days
in February 2014. A plain abdominal radiograph
revealed a dilated small bowel, ascending and
transverse colon (Fig 1). Multiple short linear calcifications scattered along the medial aspect
of the ascending colon were observed (Fig 2).
Contrast-enhanced computed tomography (CT)
revealed a long segment of circumferential bowel
wall thickening and oedema involving the caecum,
the whole length of the ascending colon, hepatic
flexure, and the proximal part of the transverse colon.
Prominent vascular calcifications that involved the
mesenteric vessels over the ascending colon were
also visualised (Fig 3).
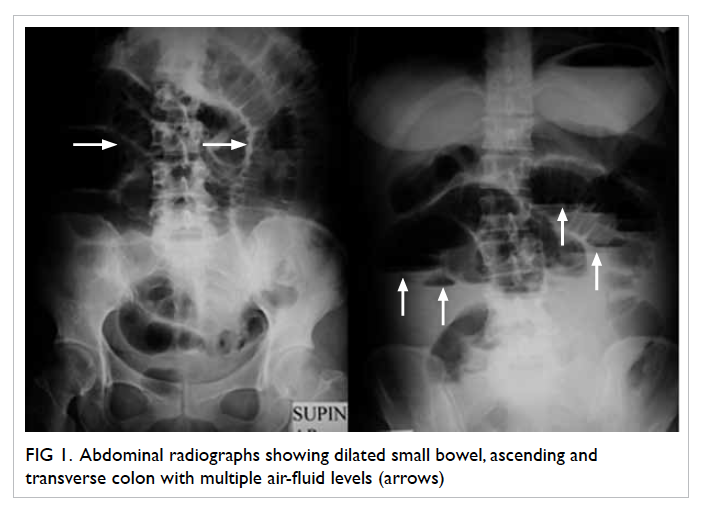
Figure 1. Abdominal radiographs showing dilated small bowel, ascending and transverse colon with multiple air-fluid levels (arrows)
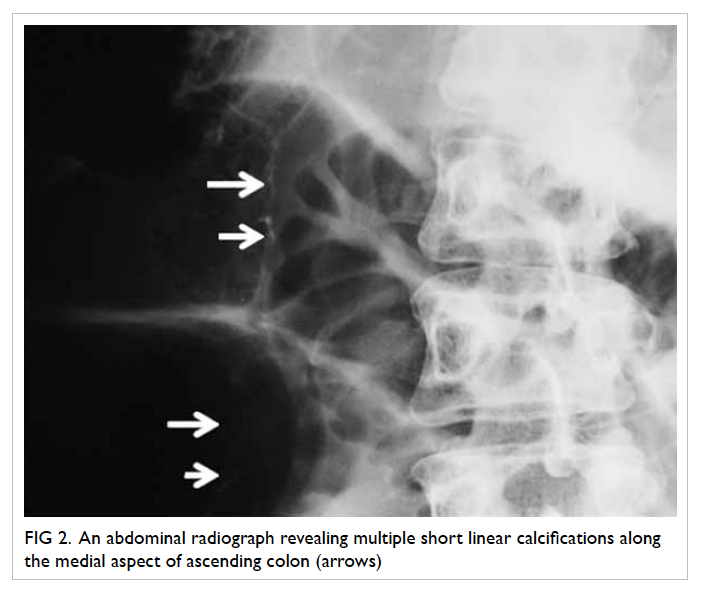
Figure 2. An abdominal radiograph revealing multiple short linear calcifications along the medial aspect of ascending colon (arrows)
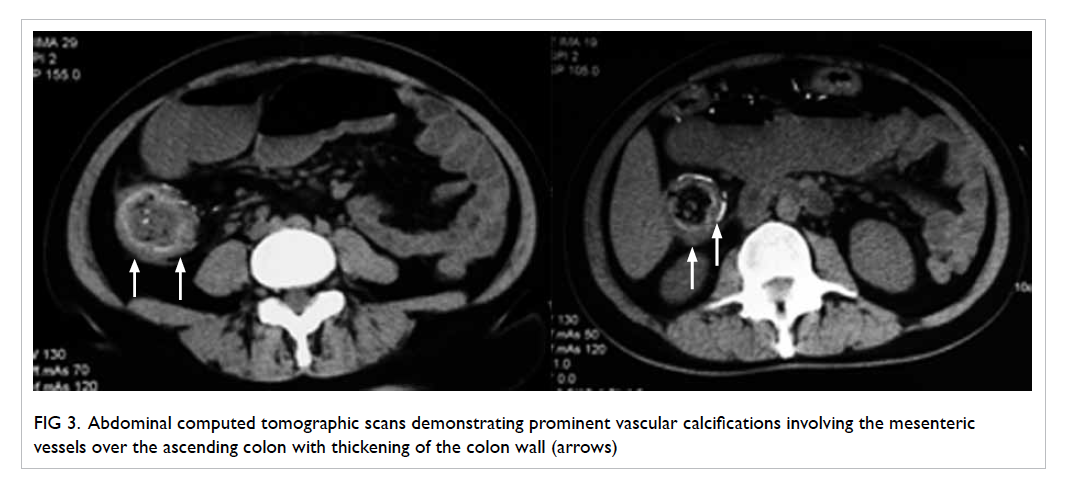
Figure 3. Abdominal computed tomographic scans demonstrating prominent vascular calcifications involving the mesenteric vessels over the ascending colon with thickening of the colon wall (arrows)
The patient was admitted to a surgical unit
and emergency laparotomy was arranged with a
provisional diagnosis of intestinal obstruction. Intra-operatively,
the colon was found to be ischaemic
from the caecum to the splenic flexure. The small
bowel was dilated and the superior mesenteric
artery was patent and pulsatile. Extended right
hemicolectomy and end ileostomy were performed.
Histopathology of a surgical specimen showed
most of the submucosal veins to have luminal
occlusion by intimal thickening and a hyalinised
wall with calcification. The pathological diagnosis
was phlebosclerotic colitis (PC). Postoperatively, the
patient’s recovery was complicated by pneumonia
that was successfully treated with antibiotics. She
was discharged home 18 days after admission.
Elective closure of the end ileostomy was performed
a few months later.
Ischaemic bowel disease is commonly caused
by thrombosis and embolism in the mesenteric
artery. Obstructed mesenteric veins causing
ischaemia are rarely reported. Phlebosclerotic
colitis is characterised by sclerosis and calcification
of the mesenteric veins leading to large bowel
ischaemia. Interestingly, a genetic factor is thought
to play an important role in this disease since most
patients with PC are of Asian descent. It has been
suggested that portal hypertension may contribute
to the condition but there is insufficient evidence to
support this relationship.1
The most common symptoms of PC are
abdominal pain, vomiting, and recurrent diarrhoea.
The clinical course is fairly long because it is caused
by chronic venous insufficiency and congestion.
Serious complications including ileus and intestinal
perforation have been reported.2 3 Phlebosclerotic
colitis has distinct radiological findings. Plain
radiographs may demonstrate multiple tortuous
threadlike vascular calcifications commonly over the
ascending colon and may extend to the transverse
colon. Findings from CT include mucosal thickening
with calcifications along the colonic wall and around
the superior mesenteric vein trunk. Colonic wall
thickening caused by oedema and fibrosis can be
seen in more detail with magnetic resonance imaging
although calcifications cannot be demonstrated.
Endoscopic examination typically shows dark
purple-blue mucosal change of the involved colon
and oedema because of venous congestion. A rigid
colon and ulceration are also observed.
There is no standardised treatment for PC.
Many authors suggest that conservative management
is sufficient unless the disease is severe or results
in complications such as peritonitis and sepsis.4
Nonetheless most reported cases have been treated
surgically. A few patients have obtained symptomatic
relief following conservative treatment but serious
relapse later has eventually resulted in a need for
surgery.1
References
1. Wang CH, Chen TY, Chin J, Wu YJ, Wang MT.
Phlebosclerotic colitis: a case with a history of herbal
ingestion. J Soc Colon Rectal Surgeon (Taiwan)
2012;23:129-34.
2. Yao T, Iwashita A, Hoashi T, et al. Phlebosclerotic colitis:
value of radiography in diagnosis—report of three cases.
Radiology 2000;214:188-92. Crossref
3. Kato T, Miyazaki K, Nakamura T, Tan KY, Chiba T, Konishi
F. Perforated phlebosclerotic colitis—description of a case
and review of this condition. Colorectal Dis 2010;12:149-51. Crossref
4. Yu CJ, Wang HH, Chou JW, et al. Phlebosclerotic
colitis with nonsurgical treatment. Int J Colorectal Dis
2009;24:1241-2. Crossref

