Hong Kong Med J 2015 Aug;21(4):318–26 | Epub 17 Jul 2015
DOI: 10.12809/hkmj144492
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Immigrants and tuberculosis in Hong Kong
CC Leung, MB, BS, FHKAM (Medicine);
CK Chan, MB, BS, FHKAM (Medicine);
KC Chang, MB, BS, FHKAM (Medicine);
WS Law, MB, ChB, FHKAM (Medicine);
SN Lee, MB, ChB, FHKAM (Medicine);
LB Tai, MB, ChB, FHKAM (Medicine);
Eric CC Leung, MB, BS, FHKAM (Medicine);
CM Tam, MB, BS, FHKAM (Medicine)
Tuberculosis and Chest Service, Department of Health, Wanchai Chest Clinic, 1/F, 99 Kennedy Road, Wanchai, Hong Kong
Corresponding author: Dr CC Leung (cc_leung@dh.gov.hk)
Abstract
Objective: To examine the impact of immigrant
populations on the epidemiology of tuberculosis in
Hong Kong.
Design: Longitudinal cohort study.
Setting: Hong Kong.
Participants: Socio-demographic and disease
characteristics of all tuberculosis notifications in
2006 were captured from the statutory tuberculosis
registry and central tuberculosis reference
laboratory. Using 2006 By-census population data,
indirect sex- and age-standardised incidence
ratios by place of birth were calculated. Treatment
outcome at 12 months was ascertained from
government tuberculosis programme record forms,
and tuberculosis relapse was tracked through the
notification registry and death registry up to 30 June
2013.
Results: Moderately higher sex- and age-standardised
incidence ratios were observed among
various immigrant groups: 1.06 (Mainland China),
2.02 (India, Pakistan, Bangladesh), 1.59 (Philippines,
Thailand, Indonesia, Nepal), and 3.11 (Vietnam).
Recent Mainland migrants had a lower sex- and
age-standardised incidence ratio (0.51 vs 1.09) than
those who immigrated 7 years ago or earlier. Age
younger than 65 years, birth in the Mainland or
the above Asian countries, and previous treatment
were independently associated with resistance to
isoniazid and/or rifampicin. Older age, birth in the
above Asian countries, non-permanent residents,
previous history of treatment, and resistance to
isoniazid and/or rifampicin were independently
associated with poor treatment outcome (other than
cure/treatment completion) at 1 year. Birth outside
Hong Kong was an independent predictor of relapse following successful
completion of treatment (adjusted
hazard ratio=1.76; 95% confidence interval, 1.07-2.89; P=0.025).
Conclusion: Immigrants carry with them a higher
tuberculosis incidence and/or drug resistance rate
from their place of origin. The higher drug resistance
rate, poorer treatment outcome, and excess relapse
risk raise concern over secondary transmission of
drug-resistant tuberculosis within the local community.
New knowledge added by this
study
- Immigrants carry with them a higher tuberculosis incidence and/or drug resistance rate from their place of origin to Hong Kong.
- Their higher drug resistance rate, poorer treatment outcome, and excess relapse risk may increase the risk of secondary transmission of drug-resistant tuberculosis within the local community.
Introduction
Great disparity in tuberculosis (TB) rates has been
reported in different parts of the world.1 Patients
with TB from 22 high-burden areas accounted
for over 80% of all notified TB cases in the world.1
Immigrants from these high-burden areas have often
been blamed for their impact on the TB situation
in many developed areas.2 3 4 5 6 7 8 9 10 11 12 A rapid increase in
population was observed in Hong Kong in the last
century, largely due to a heavy influx of immigrants
from Mainland China.13 14 15 Despite remarkable
socio-economic improvement over the past four
decades, TB remains a common disease in Hong
Kong. In 2006, the TB notification rate remained as
high as 84.1/100 000.16 With continuing population
movement between the Mainland and Hong Kong,
there has been major concern about cross-border
transmission of infections including TB.
A large-scale population census has been
conducted in Hong Kong every 10 years since
1961, with a smaller by-census in-between.
Tuberculosis is a statutorily notifiable disease, and
basic demographic, clinical, and bacteriological
data of notified cases are regularly captured by the
TB notification registry. All residents are issued an
identity card, and the identity card is used by both
the TB notification registry and death registry as a
unique personal identifier. Eighteen government
chest clinics offer free programmatic case-finding
and treatment services for TB patients under a
centralised Tuberculosis and Chest Service of the
Department of Health, with estimated programme
coverage of over 80% of the population. Sputum
culture and drug susceptibility testing are regularly
performed by a centralised laboratory that is a
Supranational Reference Laboratory within the
World Health Organization/International Union
Against Tuberculosis and Lung Diseases (WHO/IUATLD) network. Standard short-course regimens
are used in line with the WHO recommendations.
Patients are regularly followed up for 2 years after
initiation of TB treatment to facilitate cohort analysis
of treatment outcome. Using regularly captured
data within the statutory registries and government
TB programme, a longitudinal cohort study was
performed to examine the impact of immigrant
populations on the epidemiology of TB in Hong
Kong.
Methods
Data on sex, age, place of birth, residency status,
case category (new or retreatment), disease form
(pulmonary with or without extrapulmonary
involvement, or extrapulmonary only), sputum
smear and culture results of consecutive patients
notified within 2006 were obtained from the
territory-wide TB notification registry of Hong
Kong. An active case of TB was defined as positive
isolation of Mycobacterium tuberculosis complex or,
in the case of absent bacteriological confirmation,
disease diagnosed on clinical, radiological, and/or
histological grounds together with an appropriate
response to anti-TB treatment. As part of the public
health surveillance, bacteriological results of notified
cases were verified with the reports from the central
TB reference laboratory, with drug susceptibility test
results for streptomycin, isoniazid, rifampicin, and
ethambutol retrieved for culture-positive cases.
The sex- and age-stratified population data
were obtained from the 2006 By-census for the
following places of birth: Hong Kong (Group I);
Mainland China (Group II); India, Pakistan, and
Bangladesh (Indian subcontinent: Group III);
Philippines, Thailand, Indonesia, and Nepal (other
key Asian minority groups, Group IV); Vietnam
(Group V); and other miscellaneous places of birth
(Group VI).17 The crude incidence of TB among
each of the above population groups was calculated
with adjustment made by a multiplication factor
(total notified cases / [total notified cases – cases
with missing place of birth]) for cases with missing
data on place of birth. The sex- and age-specific
(by 5-year age-group) TB rates were derived from
the overall population data and applied
to the corresponding sex-age groups of each of the
above six population groups to obtain the expected
number of cases. The observed number of TB cases
for each population group was compared with the
respective number of expected cases to obtain the
indirectly standardised TB incidence ratio. The
95% confidence intervals (CIs) were calculated by
assuming a Poisson distribution in the occurrence of
events. For those born in Mainland China, further
stratification was made by the duration of residence
in Hong Kong.
The treatment outcome 12 months after
initiation of treatment was ascertained for those
patients being managed by the government chest
clinics under the Tuberculosis and Chest Service
from the programme record form of the Tuberculosis
and Chest Service. Treatment success was defined
as cure or treatment completion (successfully
completed treatment of ≥6 months for new cases and
≥8 months for retreatment cases), irrespective of
subsequent relapse or death or loss to follow-up. All
other treatment outcomes (including death before
treatment completion, default, transferring out, still
on treatment at 12 months after treatment initiation)
were regarded as unsuccessful. Permanent residents
who successfully completed treatment under the
government TB programme were subsequently
tracked up to 30 June 2013 through the territory-wide
TB notification registry and death registry for
relapse of TB or death.
Chi squared and Fisher’s exact tests were used
as appropriate for categorical variables and analysis
of variance was used for continuous variables.
Logistic regression modelling was used for multivariate
analysis of 12-month outcome. For censored data of
TB relapse during follow-up, Kaplan-Meier analysis
was used in univariate analysis and Cox proportional
hazards modelling was used in multivariate analysis
to adjust for potential confounders. A two-tailed P
value of 0.05 was considered statistically significant.
The study was part of a public health
surveillance exercise in tracking the profile and
outcome of statutory TB notifications. It did not
involve intervention on human subjects.
Results
A total of 6246 TB notifications were received
in 2006, 480 of which were excluded because of
duplicate notification or revised diagnosis, leaving
5766 cases in the 2006 TB notification registry.
Of these, 18 cases involving tourists, 17 cases
involving illegal immigrants, and 329 cases without
information on place of birth were also excluded,
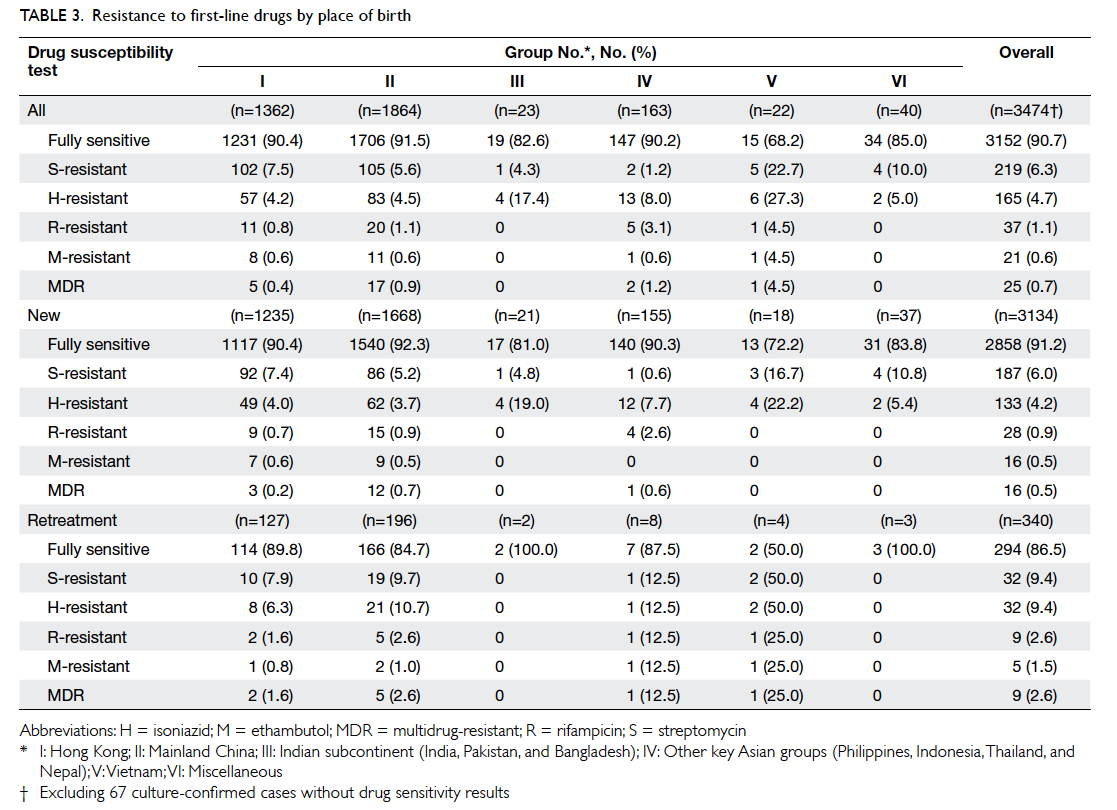
leaving 5402 cases for analysis. Table 1 shows their
basic characteristics as stratified by place of birth.
The vast majority (92.3%) of TB cases involved
residents born in either Hong Kong or Mainland
China. Significant differences were observed
between the six population groups in terms of sex
and age distribution as well as proportions of new
and pulmonary cases, but not proportions of either
smear-positive or culture-confirmed cases.
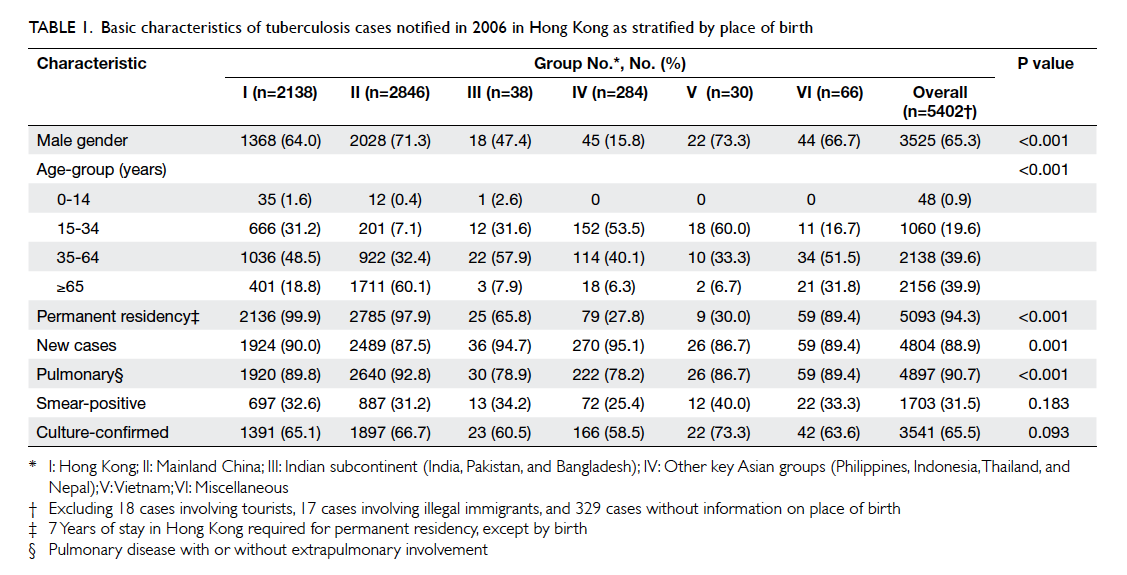
Table 1. Basic characteristics of tuberculosis cases notified in 2006 in Hong Kong as stratified by place of birth
Table 2 summarises the incidence of TB and
indirectly sex- and age-standardised incidence
ratio (SIR) of TB for the six population groups. The TB SIR was significantly above 1 for
those born in Mainland China (males and combined),
Group III (females and combined), Group IV
(females and combined), and Group V (males and
combined), but significantly below 1 for those born
in Hong Kong (males, females, and combined) and
other miscellaneous places of birth (males, females,
and combined). Mainland-born permanent residents
(staying in Hong Kong for ≥7 years) maintained a
higher TB risk than the population average for both
sexes and combined. Nonetheless, recent Mainland
immigrants with duration of stay of less than 7
years actually had a lower TB risk than the general
population, despite sex and age standardisation.
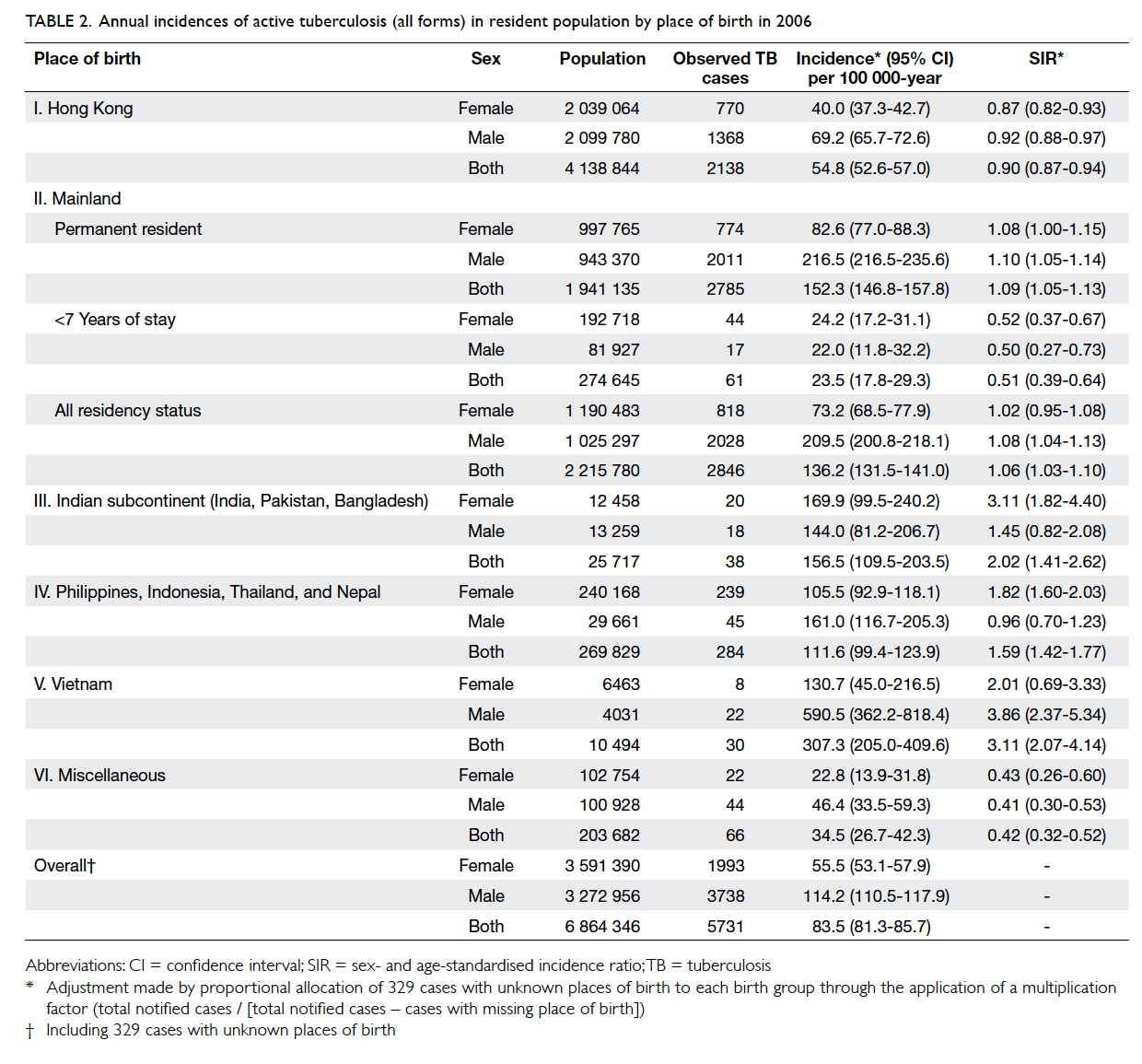
Table 2. Annual incidences of active tuberculosis (all forms) in resident population by place of birth in 2006
Table 3 shows the resistance profile of 3474 (98.1%) culture-confirmed
cases (with available drug susceptibility testing results) by place of birth. Table 4 summarises
the results of univariate and multiple logistic
analyses with respect to isoniazid, rifampicin, and
multidrug resistance (resistance to both isoniazid
and rifampicin) of 3434 culture-confirmed cases
after combining all patients born in Asian countries
listed under Groups III, IV and V, and excluding 40
patients with miscellaneous places of birth in Group
VI that included very few drug-resistant cases. In the
multiple logistic regression models using a backward
stepwise elimination approach, only age <65 years,
place of birth, and history of previous treatment
(ie retreatment cases) remained important
independent predictors of isoniazid, rifampicin, and
multidrug resistance.
Of the 5402 subjects included in this study, 4319
(80.0%) were managed, at least at some stage of the
disease, within the government TB programme. A
total of 3304 (76.5%) patients successfully completed
treatment within 12 months after initiation of
treatment. Table 5 summarises the factors associated
with 12-month treatment outcome in both univariate
analysis and multivariate logistic regression analysis.
Of those patients who successfully completed
treatment, 3176 (96.1%) permanent residents in
Hong Kong were followed up by cross-linking with
the TB notification registry and death registry until
relapse of TB, death or 30 June 2013, whichever was
the earliest. After a mean (± standard deviation)
duration of 5.28 ± 1.64 years of follow-up, 80 (2.5%)
relapses were detected at a median (range) time
interval of 1004 (225-2640) days after initiation of
treatment, 37 (46.3%) of which were bacteriologically
confirmed. In Kaplan-Meier analysis, the relapse risk
was higher among permanent residents born outside
Hong Kong than among those born in Hong Kong
(3.0% vs 1.9%; log rank test, P=0.019). A consistently
higher relapse risk was present among those born
outside Hong Kong (adjusted hazard ratio=1.76; 95%
CI, 1.07-2.89; P=0.025) after adjustment for gender,
age, case category (new or retreatment), type of
TB (pulmonary or extrapulmonary only), sputum
smear, culture, and drug resistance to isoniazid and/or rifampicin at the baseline. The Figure shows the
cumulative hazard curves by place of birth in and
outside Hong Kong in Cox proportional hazards
modelling.
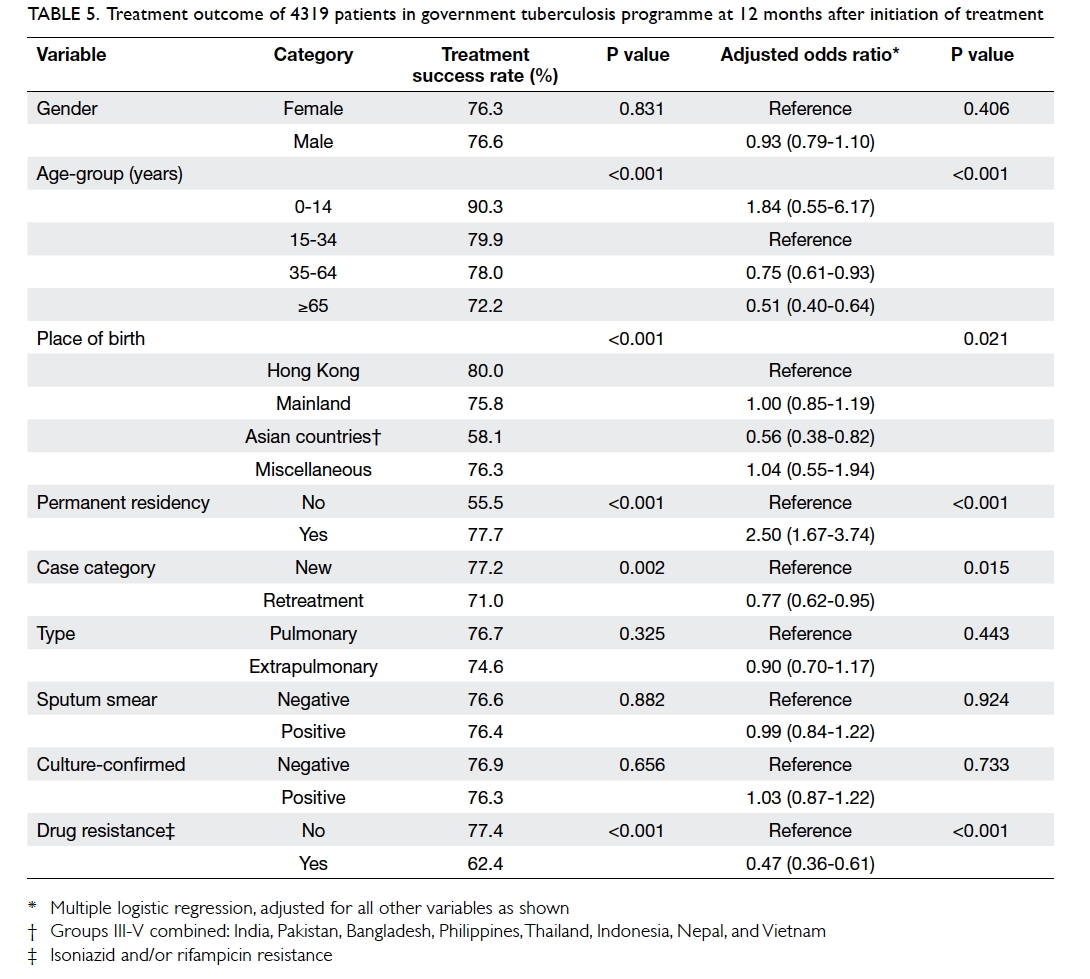
Table 5. Treatment outcome of 4319 patients in government tuberculosis programme at 12 months after initiation of treatment
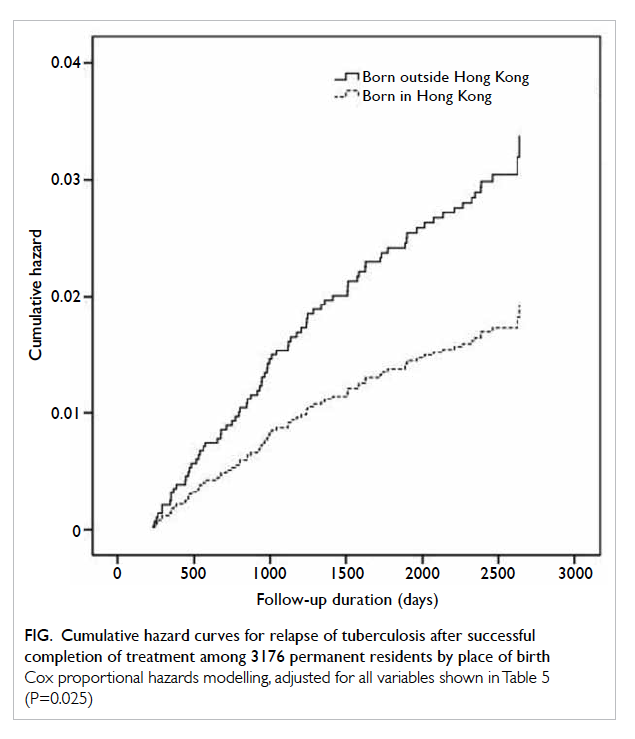
Figure. Cumulative hazard curves for relapse of tuberculosis after successful completion of treatment among 3176 permanent residents by place of birth
Cox proportional hazards modelling, adjusted for all variables shown in Table 5 (P=0.025)
Discussion
In this study, persons born in Hong Kong had a SIR of
0.90 (95% CI, 0.87-0.94), while those born in Mainland
China (Group II), Indian subcontinent (Group III),
Philippines, Indonesia, Thailand, Nepal (Group IV),
and Vietnam (Group V) had significantly higher
SIRs of 1.06, 2.02, 1.59, and 3.11 respectively (Table
2). Recent Mainland migrants (with length of stay <7
years), however, had a significantly lower SIR (0.51
vs 1.09) than other Mainland-born residents. Age
<65 years, birth in Mainland or Groups III-V Asian
countries, and history of previous treatment were
independently associated with resistance to isoniazid
and/or rifampicin (Table 4). Older age, birth in Groups
III-V Asian countries, non-permanent residents,
retreatment case, and resistance to isoniazid and/or
rifampicin were independently associated with lower
treatment success (cure/treatment completion) rate at
1 year (Table 5). Birth outside Hong Kong (Groups II-V combined) was an independent predictor of TB
relapse among permanent residents after successful
treatment completion under the government TB
programme (Fig).
With the successful control of recent
transmission of TB in Hong Kong, the majority of
TB cases arose from endogenous reactivation of
past infection.18 The higher SIR and drug resistance
prevalence among Mainland immigrants and
immigrants from Groups III-V Asia countries
corroborate reports of higher TB incidence2 3 4 5 6 8 and drug resistance7 12 among immigrants in low-TB-burden countries. These higher risks among
immigrants may have resulted at least in part from
reactivation of latent TB infection9 10 11 acquired
during their previous residence in, and/or travel to,
their places of birth with higher burdens of TB and/or drug resistance.1 19 20 21 22 Apart from possible selection
factors in migration, the progressive fall in TB
prevalence in the Mainland over the recent decades22
could also have contributed to a lower burden of
latent TB infection, and hence SIR, among recent
Mainland immigrants compared with those who
immigrated longer ago. Taking into consideration
the independent effects of birth outside Hong Kong
on both treatment outcome and relapse (Table 5
and Fig), population mobility may have adversely
affected treatment adherence, and thus impacted
on treatment outcome and/or relapse with possible
acquisition of drug resistance. In line with these
observations, a previous case-control study also
identified younger age, non-permanent residents,
and frequent travel as independent predictors of
multidrug-resistant TB among previously treated
patients in Hong Kong.23
Although this study showed an increased risk
of TB among immigrants in Hong Kong, which is a
metropolitan city with intermediate TB burden, the
vast majority of TB cases still occurred among the
majority population groups of local-born persons or
permanent residents born in Mainland China (both
of which were largely of Chinese ethnicity). This is
contrary to the situation in most low-burden areas,
where the majority of TB cases often came from
foreign-born minority groups.2 3 12 The relatively high
crude TB incidence rate of 55/100 000, even among
the local-born (both genders combined) in this intermediate burden area
(Table 2), could have reduced the risk differential
between the immigrant groups and the local-born,
thus reducing the influence of immigrants on the
overall TB incidence. Nonetheless, the higher drug
resistance rate, poorer treatment outcome, and
higher relapse rate among immigrants in this study
remain critical areas of concern. In a recent study
on the transmission of drug-resistant TB in Hong
Kong,24 46% of all multidrug-resistant TB cases were
new cases with no previous history of treatment.
This suggests ongoing transmission of these difficult-to-treat TB cases within our community. The degree
of molecular clustering was as high as 65% among
extensively drug-resistant TB cases, the majority of
which did not have obvious epidemiological linkage,
suggesting active transmission outside households
or other conventional close contact settings.24
This study was based on territory-wide data
from by-census, statutory registries, a centralised
government TB programme, and centralised
TB laboratory. The well-developed health care
infrastructure in Hong Kong with easy access to
free TB care services allowed capture of relevant
information from TB patients notified in a by-census
year and successful tracking of the majority
of them for treatment outcome and relapse. Some
degree of incomplete case ascertainment was still
likely as in all other public health surveillance
systems. Even though around 20% of the notified
patients were managed outside the government
TB programme, this might not have substantially
confounded the internal comparisons among
different population groups if access to care could be
assumed to be roughly parallel. If the usual inverse
care law25 did apply, the direction of bias would
likely be underestimation of the risks among the
immigrants as an underprivileged group. With the
limited amount of socio-demographic and clinical
information contained in the various statutory
registries and programme forms, this study may
not be in a strong position to analyse the complex
mechanisms that underlie the observed associations
between immigrants and treatment outcome or
relapse. Further studies are therefore warranted to
identify potential areas of intervention for specific
minority groups.
Declaration
No external grant or support has been received for
this study.
References
1. Global tuberculosis control report 2013. WHO/HTM/TB/2013.11. Available from: http://apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf.
Accessed May 2015.
2. Gilbert RL, Antoine D, French CE, Abubakar I, Watson JM,
Jones JA. The impact of immigration on tuberculosis rates
in the United Kingdom compared with other European
countries. Int J Tuberc Lung Dis 2009;13:645-51.
3. Das D, Baker M, Venugopal K, McAllister S. Why the
tuberculosis incidence rate is not falling in New Zealand.
N Z Med J 2006;119:U2248.
4. Cain KP, Haley CA, Armstrong LR, et al. Tuberculosis
among foreign-born persons in the United States:
achieving tuberculosis elimination. Am J Respir Crit Care
Med 2007;175:75-9. Crossref
5. Dye C, Lönnroth K, Jaramillo E, Williams BG, Raviglione
M. Trends in tuberculosis incidence and their determinants
in 134 countries. Bull World Health Organ 2009;87:683-91. Crossref
6. Svensson E, Millet J, Lindqvist A, et al. Impact of
immigration on tuberculosis epidemiology in a low-incidence
country. Clin Microbiol Infect 2011;17:881-7. Crossref
7. Baussano I, Mercadante S, Pareek M, Lalvani A, Bugiani
M. High rates of Mycobacterium tuberculosis among
socially marginalized immigrants in low-incidence area,
1991-2010, Italy. Emerg Infect Dis 2013;19:1437-45. Crossref
8. Manangan L, Elmore K, Lewis B, et al. Disparities in
tuberculosis between Asian/Pacific Islanders and non-Hispanic Whites, United States, 1993-2006. Int J Tuberc
Lung Dis 2009;13:1077-85.
9. Farah MG, Meyer HE, Selmer R, Heldal E, Bjune G. Long-term
risk of tuberculosis among immigrants in Norway. Int
J Epidemiol 2005;34:1005-11. Crossref
10. Patel S, Parsyan AE, Gunn J, et al. Risk of progression to
active tuberculosis among foreign-born persons with
latent tuberculosis. Chest 2007;131:1811-6. Crossref
11. McPherson ME, Kelly H, Patel MS, Leslie D. Persistent
risk of tuberculosis in migrants a decade after arrival in
Australia. Med J Aust 2008;188:528-31.
12. Long R, Langlois-Klassen D. Increase in multidrug-resistant
tuberculosis (MDR-TB) in Alberta among foreign-born
persons: implications for tuberculosis management.
Can J Public Health 2013;104:e22-7.
13. Tuberculosis and Chest Service. Annual Report of
Tuberculosis and Chest Service 1949. Hong Kong:
Department of Health; 1950: 3.
14. Tuberculosis and Chest Service. Annual Report of
Tuberculosis and Chest Service 1961. Hong Kong:
Department of Health; 1962: 3.
15. Hong Kong Monthly Digest of Statistics April 2012, p.9.
Available from: http://www.census2011.gov.hk/pdf/Feature_articles/Trends_Pop_DH.pdf. Accessed 3 Jul 2013.
16. Tuberculosis and Chest Service. Annual Report of
Tuberculosis and Chest Service 2006. Hong Kong: Department of Health; 2008.
17. Census and Social Statistics Department of Hong Kong,
2006 Population By-census. Available from: http://www.bycensus2006.gov.hk/en/data/data2/index.htm. Accessed
3 Jul 2014.
18. Chan-Yeung M, Kam KM, Leung CC, et al. Population-based
prospective molecular and conventional
epidemiological study of tuberculosis in Hong Kong.
Respirology 2006;11:442-8. Crossref
19. Zignol M, van Gemert W, Falzon D, et al. Surveillance of
anti-tuberculosis drug resistance in the world: an updated
analysis, 2007-2010. Bull World Health Organ 2012;90:111-119D. Crossref
20. Zhao Y, Xu S, Wang L, et al. National survey of drug-resistant
tuberculosis in China. N Engl J Med 2012;366:2161-70. Crossref
21. Udwadia ZF, Amale RA, Ajbani KK, Rodrigues C. Totally
drug-resistant tuberculosis in India. Clin Infect Dis
2012;54:579-81. Crossref
22. Wang L, Zhang H, Ruan Y, et al. Tuberculosis prevalence
in China, 1990-2010; a longitudinal analysis of national
survey data. Lancet 2014;383:2057-64. Crossref
23. Law WS, Yew WW, Leung CC, et al. Risk factors for
multidrug-resistant tuberculosis in Hong Kong. Int J
Tuberc Lung Dis 2008;12:1065-70.
24. Leung EC, Leung CC, Kam KM, et al. Transmission
of multidrug-resistant and extensively drug-resistant
tuberculosis in a metropolitan city. Eur Respir J
2013;41:901-8. Crossref
25. Hart JT. The inverse care law. Lancet 1971;1:405-12. Crossref