Hong Kong Med J 2015 Aug;21(4):310–7 | Epub 17 Jul 2015
DOI: 10.12809/hkmj144393
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Indications for and pregnancy outcomes of cervical cerclage: 11-year comparison of patients undergoing history-indicated, ultrasound-indicated, or rescue cerclage
Lucia LK Chan, MB, BS, MRCOG1;
TW Leung, PhD, FRCOG1;
TK Lo, MB, BS, FHKAM (Obstetrics and Gynaecology)2;
WL Lau, MB, BS, FRCOG1;
WC Leung, MD, FRCOG1
1 Department of Obstetrics and Gynaecology, Kwong Wah Hospital, Yaumatei, Hong Kong
2 Department of Obstetrics and Gynaecology, Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr Lucia LK Chan (lucia118@gmail.com)
Abstract
Objectives: To review and compare pregnancy
outcomes of patients undergoing history-indicated,
ultrasound-indicated, or rescue cerclage.
Design: Case series with internal comparison.
Setting: A regional obstetric unit in Hong Kong.
Patients: Women undergoing cervical cerclage at
Kwong Wah Hospital between 1 January 2001 and
31 December 2011.
Interventions: Cervical cerclage.
Main outcome measures: Pregnancy outcomes
including miscarriage, gestational age at delivery,
birth weight, and duration of pregnancy prolongation.
Results: Overall, 47 patients were included. Nine
(19.1%) pregnancies resulted in miscarriage. The
median gestational age at delivery was 35.7 weeks.
Among the 23 patients who had history-indicated
cerclage, only four (17.4%) had three or more previous second-trimester miscarriages or
preterm deliveries. Among the 15 patients who had
ultrasound-indicated cerclage, preoperative cervical
length of ≤1.5 cm was associated with shorter
prolongation of pregnancy, compared with that
of >1.5 cm (median, 12.1 vs 18.4 weeks; P=0.009).
Among the nine women who had rescue cerclage,
those who underwent the procedure before 20 weeks
of gestation delivered earlier than those underwent
cerclage later (median, 22.5 vs 34.1 weeks; P=0.048).
Conclusions: Patients eligible for the Royal College of
Obstetricians and Gynaecologists–recommended
history-indicated cerclage remain few. The majority
of patients may benefit from serial ultrasound
monitoring of cervical length with or without
ultrasound-indicated cerclage.
New knowledge added by this
study
- Women who had rescue cerclage before 20 weeks of gestation delivered significantly earlier than those who had the procedure performed later, supporting the expert opinion in the Royal College of Obstetricians and Gynaecologists (RCOG) guideline.
- The majority of patients may benefit from serial ultrasound monitoring of cervical length with or without ultrasound-indicated cerclage. A proposed algorithm on the management of patients, taking into consideration the RCOG guideline, is presented.
Introduction
Cervical cerclage was introduced by Shirodkar1
and McDonald2 in the 1950s, and has since become
a common obstetric practice for the secondary
prevention of preterm birth.3 4 Cervical cerclage is
performed in patients with a history of cervical
insufficiency; preterm labour or second-trimester
miscarriage; cervical dilatation in the second
trimester; or shortened cervix noted on transvaginal
ultrasound examination.
Although cervical cerclage is a common
obstetric procedure, there is still controversy
regarding its efficacy and patient selection. While
some studies showed that cervical cerclage
did not prolong gestation or improve neonatal
survival,5 6 7 8 9 others suggested that the procedure was
beneficial.10 11 12 13 14 15 For instance, a large trial demonstrated
that the incidence of preterm delivery before 33
weeks was halved by cervical cerclage among women
with a history of three or more preterm
deliveries before 37 weeks.10 It was shown in a meta-analysis11
and another study12 that among women
with shortened cervical length with or without
prior preterm birth, the risk of preterm birth with
or without perinatal mortality was significantly
reduced by cerclage. Rescue cerclage was also found
to prolong pregnancy, reduce the risk of preterm
labour,13 14 and improve neonatal survival and birth
weight, even in women considered at low risk of
preterm delivery in view of their obstetric
history.15
Decisions for cervical cerclage are difficult
and are often based on the clinical judgement of the
senior obstetrician. The guideline on cervical cerclage
published by the Royal College of Obstetricians and
Gynaecologists (RCOG) in 2011, which classifies
cervical cerclage into history-indicated, ultrasound-indicated and rescue cerclage, provides updated
evidence in this area.16
Nevertheless, on review of the literature
worldwide, no studies have been reported to
investigate systematically the use and outcomes
of cervical cerclage according to this new RCOG
classification. Hence, this study aimed to review
the indications and the pregnancy outcomes
(miscarriage, gestational age at delivery, birth weight,
prolongation of pregnancy, and rate of preterm birth
before 34 weeks) of cervical cerclage in a regional
obstetric unit in Hong Kong according to the RCOG
categorisation. Any change in practice of cervical
cerclage in the unit over 11 years was also reviewed.
Methods
This was a retrospective review of patients who had
cervical cerclage performed in a regional obstetric
unit in Hong Kong between 1 January 2001 and
31 December 2011. Ethics approval from the local
institutional review board (Kowloon West Cluster
Clinical Research Ethics Committee Reference: KW/EX-13-041[61-62]) was obtained. Patients who had
undergone cervical cerclage were identified by the
Clinical Data Analysis and Reporting System, which
is a computerised database of the Hospital Authority,
Hong Kong, using the key word “cervical cerclage”.
The clinical data for these patients were retrieved
and reviewed.
The patients were divided into three
subgroups for data analysis. Group 1 included
patients with history-indicated cerclage, that is,
cerclage was performed in women with obstetric or
gynaecological risk factors for spontaneous second-trimester
loss or preterm delivery. Group 2 were
patients with ultrasound-indicated cerclage, that
is, cerclage was performed for women with cervical
shortening (<2.5 cm) detected by transvaginal
ultrasound examination, without exposure of fetal
membranes in the vagina. This group comprised
women who planned for history-indicated cerclage
with preoperative sonographic finding of shortened
cervix; had a history of preterm delivery before
37 weeks or second-trimester miscarriage(s) and
underwent ultrasound monitoring of cervical length;
or were incidentally found to have sonographic
cervical shortening. Regular ultrasound examination
was not performed for all patients and, if done, the
frequency of monitoring was determined individually.
Group 3 consisted of patients undergoing rescue
cerclage, that is, cerclage was performed for women
with premature cervical dilatation and exposure of
fetal membranes in the vagina, which was either
detected by ultrasound examination of the cervix
or by speculum/physical examination for symptoms
such as vaginal discharge, bleeding, or ‘sensation of
pressure’, with or without a history of preterm
birth before 37 weeks or second-trimester losses.
The definitions of history-indicated cerclage
and ultrasound-indicated cerclage in this study were
not exactly the same as the RCOG definitions,16
which suggest that history-indicated cerclage should
be offered to women with three or more previous preterm births and/or second-trimester
losses, while ultrasound-indicated cerclage should
be offered to women with one or more previous preterm birth or second-trimester loss and
sonographic cervical shortening (≤2.5 cm) before
24 weeks of gestation. To explore the significance
of the differences in the category definitions, a sub-analysis
was performed by dividing the present
cohort into two groups. Group A included women
who underwent history-indicated or ultrasound-indicated
cerclage as defined by the RCOG guideline. Group B included women who had the procedure
performed without strictly following the RCOG
guideline.
All cervical cerclage procedures were
performed by a senior obstetrician using the
McDonald’s technique with Mersilene tape
(Ethicon, West Somerville [NJ], US). Perioperative
management—such as the use of prophylactic
antibiotics and/or tocolytics, bed rest, and the
choice of anaesthesia—was at the discretion of the
operating team. The interval between the diagnosis
of cervical incompetence and the performance of
rescue cervical cerclage ranged from 0 to 3 days.
The Statistical Package for the Social Sciences
(Windows version 20.0; SPSS Inc, Chicago [IL],
US) was used for statistical analysis. The pregnancy
outcomes studied included miscarriage, gestational
age at delivery, birth weight, and duration of
prolongation of pregnancy. Kruskal-Wallis test and
Pearson Chi squared test were employed to analyse
the relationship between indication for cerclage
and various pregnancy outcomes. Patients who had
history-indicated or ultrasound-indicated cerclage
as defined by the RCOG guideline (group A) were
compared with patients who had the procedure
performed without strictly following the RCOG
definition (group B) by the Mann-Whitney U
test and Fisher’s exact test. Fisher’s exact test and
Mann-Whitney U test were used, respectively, to
compare the indications for cerclage and the various
pregnancy outcomes between two different time
periods (2001-2005 vs 2006-2011). A P value of less
than 0.05 was taken as statistically significant.
Results
Overall, 47 patients with a singleton pregnancy were
included in this study. The majority (87.2%) were
Chinese. No immediate operative complications
associated with cervical cerclage (namely membrane
rupture or miscarriage within 1 week) occurred
except for one miscarriage.
Among the 47 patients, nine (19.1%)
pregnancies resulted in miscarriage, and 28 (59.6%)
patients delivered after 34 weeks of gestation. The
median gestational age at delivery was 35.7 (range,
14.9-40.1) weeks, with a median birth weight of
2270 (range, 75-3960) g. The median prolongation
of pregnancy after cervical cerclage was 17.3
(range, 0.3-27.1) weeks. Among the 38 patients who
delivered after 24 weeks of gestation, 29 (76.3%)
delivered by normal spontaneous delivery, eight
(21.1%) by lower segment caesarean section, and one
(2.6%) by vacuum extraction.
Patients undergoing history-indicated cerclage (group 1; n=23)
Cerclage was performed at a median gestation
of 14.6 (range, 12.4-19.6) weeks (Table 1). The median cervical length of the 20 patients who had it
measured preoperatively by ultrasound examination
was 3.5 (range, 2.5-4.8) cm. Four (17.4%) patients
had three or more previous second-trimester
miscarriages or preterm deliveries (ie the
true history-indicated cerclage group as defined
by the RCOG guidelines) and 13 (56.5%) had two
or more second-trimester miscarriages
or preterm deliveries. One patient did not have
previous second-trimester miscarriage or preterm
delivery, but had a history of large loop excision
of transformation zone for cervical intraepithelial
neoplasia, two terminations of pregnancy, and
recurrent first-trimester miscarriages.

Table 1. Demographic characteristics and pregnancy outcomes of patients with different indications for cervical cerclage
No significant association was found between
pregnancy outcomes and the gestation at which
cerclage was performed. The pregnancy outcomes
of the four women with three or more previous second-trimester miscarriages or preterm
deliveries were compared with the other 19
women who had less than three second-trimester
miscarriages or preterm deliveries. The former
group tended to have a better pregnancy outcome,
with higher gestational age at delivery (median,
38.1 weeks vs 37.4 weeks) and heavier birth weight
(median, 3135 vs 2570 g) than the latter group,
although these differences did not reach statistical
significance.
Patients undergoing ultrasound-indicated cerclage (group 2; n=15)
Cerclage was performed at a median gestation of
18.6 (range, 14.3-23.4) weeks (Table 1). Shortened
cervical length with or without funnelling of the
cervix was detected on ultrasound examination. The
median cervical length was 1.5 (range, 0-2.4) cm. All
patients had cervical length of <2.5 cm.
Patients with a preoperative cervical length
of ≤1.5 cm had significantly shorter prolongation
of pregnancy compared with patients with a
preoperative cervical length of >1.5 cm (median,
12.1 vs 18.4 weeks, P=0.009). Seven (46.7%) patients
had cervical funnelling. No significant difference
in pregnancy outcomes was detected between
patients with and without cervical funnelling seen
in the preoperative ultrasound examination. Among
the 15 patients undergoing ultrasound-indicated
cerclage, 13 (86.7%) had a history of
second-trimester miscarriages or preterm deliveries.
No significant difference in pregnancy outcomes
was found between patients with or without a history of second-trimester miscarriages or preterm
deliveries.
Patients undergoing rescue cerclage (group 3; n=9)
Rescue cerclage was performed at a median
gestation of 19.3 (range, 16.1-23.0) weeks (Table 1).
Cervical dilatation ranged from 2 to 3 cm at the time
of diagnosis. Among the nine patients undergoing
rescue cerclage, six (66.7%) had a history of
second-trimester miscarriages or preterm deliveries.
The diagnosis of cervical dilatation among these six
women was made by either ultrasound assessment
or physical examination based on symptoms. One
patient had history-indicated cervical cerclage
performed at a private hospital at 12 weeks of
gestation. She presented with increased vaginal
discharge at 22 weeks and was found to have cervical
dilatation with a loosened cerclage stitch. Rescue
cerclage was performed.
All the patients who miscarried after rescue
cerclage had the procedure performed before 20
weeks of gestation. Women who underwent cerclage
before 20 weeks delivered at an earlier gestation
(median, 22.5 vs 34.1 weeks; P=0.048) and had smaller
babies (median birth weight, 565 vs 2190 g; P=0.048)
than women who had cerclage at a later gestation.
Comparison among the three groups of patients
There were no significant differences in age, body
mass index, or parity between the three groups.
Cerclage was performed at a significantly earlier
gestation for patients with history-indicated cerclage
compared with the other two groups (P<0.001; Table 1).
Regarding the pregnancy outcomes, it seems
that patients undergoing rescue cerclage had a higher
incidence of miscarriage than the other two groups
(44.4% vs 20.0% in the ultrasound-indicated group
and 8.7% in the history-indicated group), although
the differences did not reach statistical significance
(P=0.07), probably because of the small number of
patients included in each group (Table 1).
Patients in the history-indicated and
ultrasound-indicated cerclage groups had
significantly longer prolongation of pregnancy,
delivered at later gestation, and had heavier birth
weight babies than women in the rescue cerclage
group (Table 1). Nevertheless, there were no
statistically significant differences in the gestational
age at delivery or birth weight between patients in
history-indicated cerclage group and the ultrasound-indicated
group, although the former group had significantly longer
prolongation of pregnancy than the latter group (P=0.002).
Comparison between patients in group A and group B according to the Royal College of Obstetricians and Gynaecologists definition
Comparison between patients who had history-indicated
or ultrasound-indicated cerclage as
defined by the RCOG guideline (group A) with
patients who had the procedure performed without
strictly following the RCOG definition (group B) was
made. Group A consisted of four patients who had
history-indicated cerclage and 13 patients who had
ultrasound-indicated cerclage. Group B comprised
19 patients who had history-indicated cerclage
and two patients who had ultrasound-indicated
cerclage. No significant differences were detected
in the demographic characteristics between the
two groups. There were also no significant differences in
the pregnancy outcomes between the two groups,
including miscarriage rate, gestational age at delivery,
preterm delivery rate before 34 weeks of gestation,
birth weight, and prolongation of pregnancy (Table 2).
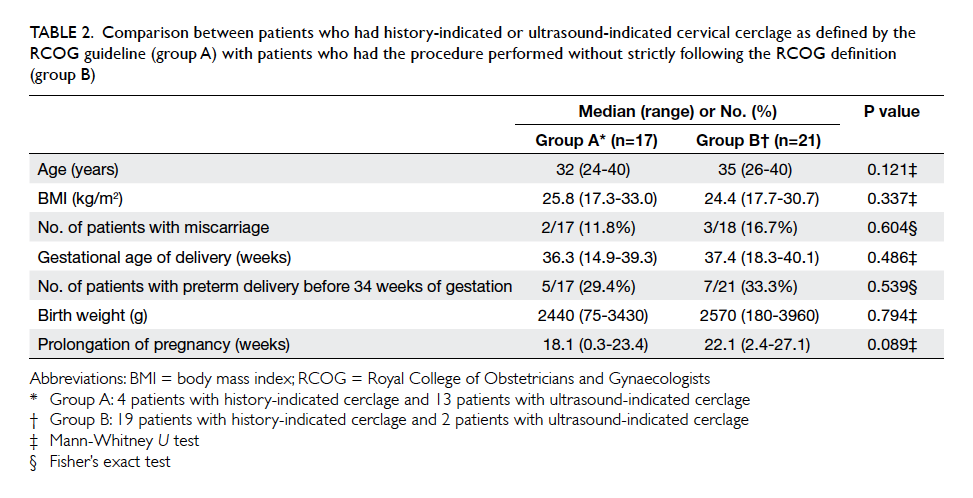
Table 2. Comparison between patients who had history-indicated or ultrasound-indicated cervical cerclage as defined by the RCOG guideline (group A) with patients who had the procedure performed without strictly following the RCOG definition (group B)
Comparison of the cerclage practice between 2001-2005 and 2006-2011
There was a trend for more ultrasound-indicated
cerclage and rescue cerclage in 2006-2011 than in
2001-2005. More history-indicated or ultrasound-indicated
cerclages were performed according to
the RCOG’s recommendation in 2006-2011 than in
2001-2005 (50% vs 38.9%), although the difference
did not reach statistical significance (P=0.532),
probably because of the small sample size (Table 3).
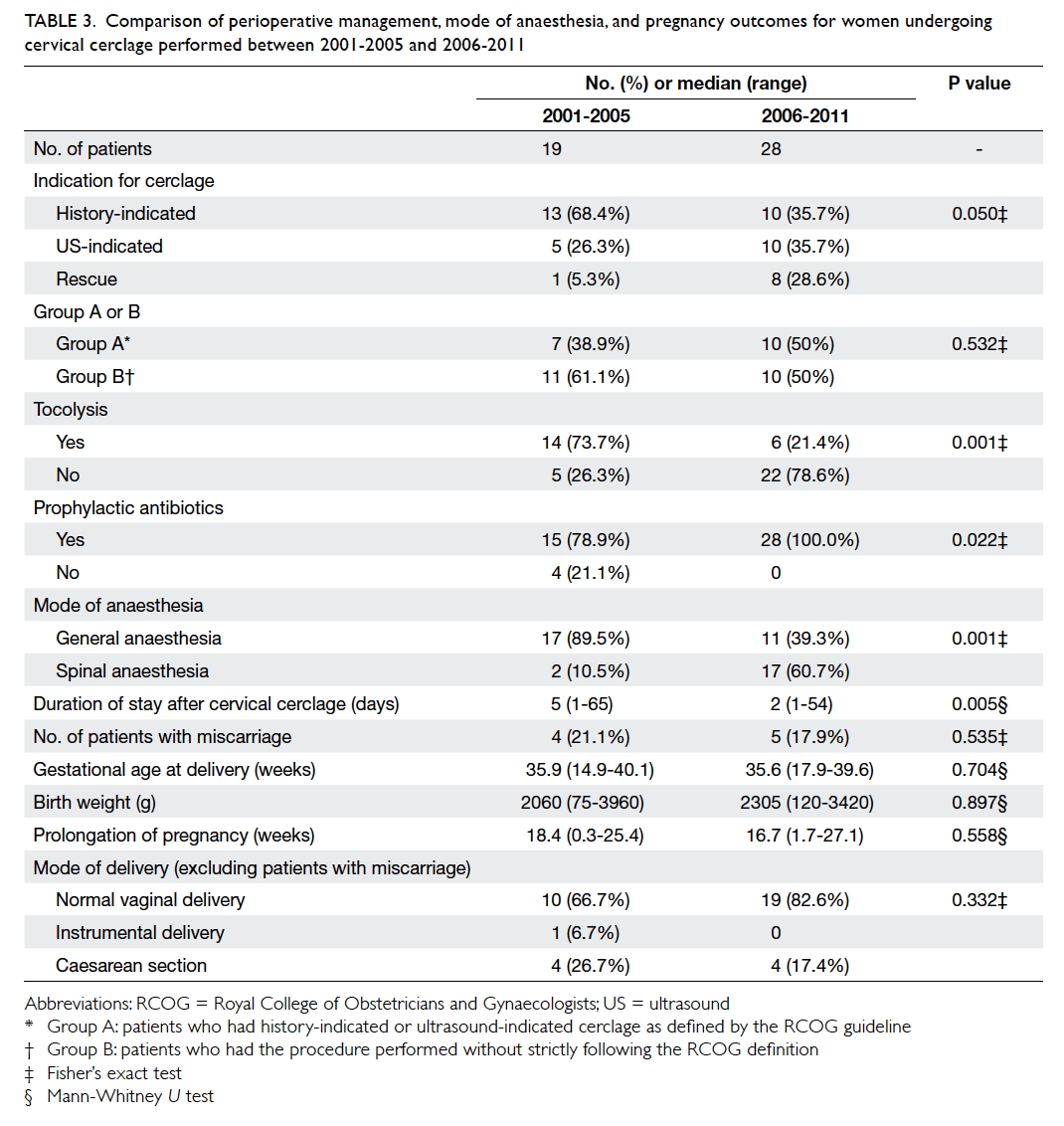
Table 3. Comparison of perioperative management, mode of anaesthesia, and pregnancy outcomes for women undergoing cervical cerclage performed between 2001-2005 and 2006-2011
Pregnancy outcomes were similar between
the two periods. However, there was less use of
prophylactic tocolysis, but more frequent use of
spinal anaesthesia and prophylactic antibiotics in
2006-2011 than in 2001-2005. The median duration of
hospital stay was also significantly shorter in 2006-2011 than in 2001-2005 (Table 3).
Discussion
This retrospective study reviewed systematically the
use and outcomes of cervical cerclage according to
the new 2011 RCOG categorisation,16 although not
all cases followed strictly the exact definition of
history-indicated or ultrasound-indicated cerclage
in the RCOG guideline. The data from the study may
help provide more evidence on the application of the
new guideline for making the decision for cervical
cerclage among women at risk of or diagnosed with
cervical incompetence.
In this study, only four (17.4%) patients
fulfilled the RCOG recommendation16 for history-indicated
cerclage (ie ≥3 previous second-trimester
miscarriages or preterm deliveries), although more
than half of the women in the group (n=13, 56.5%)
had a history of two or more second-trimester
miscarriages or preterm deliveries. This
suggests that in clinical practice, women eligible
for cerclage based on their obstetric history alone
are few and, hence, serial ultrasound monitoring of
cervical length is needed for most of the women at
risk for cervical incompetence.
The optimal cervical length for recommending
cerclage is controversial.12 17 One multicentre trial
suggested that cerclage should be performed at
cervical length of <1.5 cm,12 whereas a meta-analysis
suggested that cerclage should be done for women
with a singleton gestation with a previous preterm
birth and cervical length of <2.5 cm.17 Our study
showed that patients with preoperative cervical
length of ≤1.5 cm had shorter prolongation of
pregnancy compared with those with preoperative
cervical length of 1.5 to 2.4 cm, supporting the
recommendation that cervical cerclage should be
offered if sonographic cervical shortening to ≤2.5
cm is detected (Fig). No significant difference in
pregnancy outcomes was detected between patients
with and without preoperative sonographic cervical
funnelling. Review of the literature also suggests that
cervical funnelling is not an independent risk factor
for preterm birth.18 Hence, cervical funnelling is not
recommended as a criterion to offer cerclage.
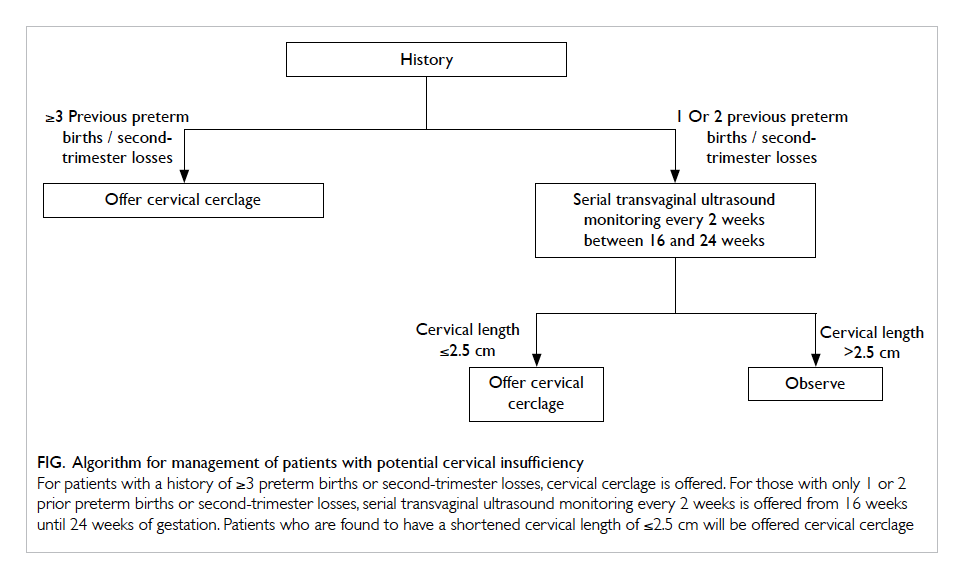
Figure. Algorithm for management of patients with potential cervical insufficiency
For patients with a history of ≥3 preterm births or second-trimester losses, cervical cerclage is offered. For those with only 1 or 2 prior preterm births or second-trimester losses, serial transvaginal ultrasound monitoring every 2 weeks is offered from 16 weeks until 24 weeks of gestation. Patients who are found to have a shortened cervical length of ≤2.5 cm will be offered cervical cerclage
Group A comprised patients who had three
or more previous preterm deliveries
or second-trimester miscarriages in the history-indicated
cerclage group and patients with one or
more previous preterm delivery or second-trimester
miscarriage in the ultrasound-indicated
cerclage group, and therefore was expected to carry
a higher risk for preterm delivery or miscarriage
and, hence, a worse pregnancy outcome compared
with group B patients, who did not strictly fulfil the
RCOG recommendation. Interestingly, no significant
difference in pregnancy outcomes was detected
between group A and group B patients. This may
be due to the small sample size in each group. This,
however, may mean that a less stringent criterion
to offer cerclage other than the present RCOG
recommendation may still be helpful for women at
risk for cervical incompetence. A prospective study
with a larger sample size to compare the pregnancy
outcomes between these two groups of patients is
warranted.
Women who had rescue cerclage before 20
weeks delivered significantly earlier than those
who underwent the procedure later than 20 weeks.
Although it is stated in the 2011 RCOG guideline that
“in cases presenting before 20 weeks of gestation,
insertion of a rescue cerclage is highly likely to result
in a preterm delivery before 28 weeks of gestation”,16
this is based on expert opinion only, rather than
data from previous studies. The result from this
study provides new evidence to support such expert
opinion.
Among patients with history-indicated or
ultrasound-indicated cerclage, more patients fulfilled
the RCOG’s recommendation in 2006-2011 than
in 2001-2005 (50.0% vs 38.9%). This suggests that
even before the publication of the RCOG guideline
in 2011, the practice of cervical cerclage has already
been changing, with a shift towards more stringent
criteria for offering cerclage.
Strengths and limitations of this study
This study reviewed systematically the use and
outcomes of cervical cerclage according to the
categories in the new 2011 RCOG guideline.16 The
data obtained may help in patient selection and
counselling for cerclage. The major limitations
include small sample size and lack of control groups.
Moreover, not all patients included in the history-indicated
and ultrasound-indicated groups fulfilled
exactly the strict RCOG definitions for the respective
groups.
The way forward
Although the RCOG guideline recommends history-indicated
cerclage be performed in patients with a
history of three or more previous second-trimester
miscarriages or preterm deliveries, in
clinical practice, this group of patients remains
small. In the present study, only 17.4% of patients
in the history-indicated cerclage group fulfilled
such criteria. The majority of patients with potential
cervical insufficiency encountered are those with a
history of one or two previous second-trimester
miscarriages or preterm deliveries, who may benefit
from serial ultrasound monitoring of cervical length
with or without ultrasound-indicated cerclage. Based
on the findings from this study, an algorithm for
the management of patients with potential cervical
insufficiency is proposed (Fig).
A major limitation of ultrasound monitoring
is the difficulty of timely identification of
sudden cervical shortening and dilatation. The
recommended frequency of ultrasound surveillance
is not well established. Since this study demonstrated
that rescue cerclage performed before 20 weeks
of gestation was associated with a much poorer
pregnancy outcome than procedures done at a later
gestation, it is recommended that among patients
with a history of one or two previous preterm births
or second-trimester miscarriages, serial ultrasound
monitoring should be performed every 2 weeks
between 16 and 24 weeks of gestation (Fig). This may help optimise the early detection of cervical
shortening in time and, hence, allow ultrasound-indicated
cerclage be performed instead of rescue
cerclage. Nevertheless, such practice requires a
greater demand on manpower to perform ultrasound
examinations and may not be applicable in small
units with few staff. In order to improve the quality
of care for patients with potential cervical
insufficiency, allocation of resources for serial
ultrasound monitoring for this group of patients is
warranted.
Conclusions
Patients eligible for history-indicated cerclage
according to the RCOG recommendation remain
few. The majority of patients may benefit from serial
ultrasound monitoring of cervical length with or
without ultrasound-indicated cerclage, which is
preferably performed at a cervical length between
1.5 and 2.5 cm.
Declaration
The authors have no conflicts of interest to declare.
References
1. Shirodkar VN. A new method of operative treatment for
habitual abortion in the second trimester of pregnancy.
Antiseptic 1955;52:299-300.
2. McDonald IA. Suture of the cervix for inevitable
miscarriage. J Obstet Gynaecol Br Emp 1957;64:346-50. Crossref
3. Spong CY. Prediction and prevention of recurrent
spontaneous preterm birth. Obstet Gynecol 2007;110:405-15. Crossref
4. Flood K, Malone FD. Prevention of preterm birth. Semin
Fetal Neonatal Med 2012;17:58-63. CrossRef
5. Rush RW, Isaacs S, McPherson K, Jones L, Chalmers I,
Grant A. A randomized controlled trial of cervical cerclage
in women at high risk of spontaneous preterm delivery. Br
J Obstet Gynaecol 1984;91:724-30. Crossref
6. Berghella V, Daly SF, Tolosa JE, et al. Prediction of preterm
delivery with transvaginal ultrasonography of the cervix in
patients with high-risk pregnancies: does cerclage prevent
prematurity? Am J Obstet Gynecol 1999;181:809-15. Crossref
7. Rust OA, Atlas RO, Reed J, van Gaalen J, Balducci J.
Revisiting the short cervix detected by transvaginal
ultrasound in the second trimester: why cerclage therapy
may not help. Am J Obstet Gynecol 2001;185:1098-105. Crossref
8. Berghella V, Odibo AO, Tolosa JE. Cerclage for prevention
of preterm birth in women with a short cervix found on
transvaginal ultrasound examination: a randomized trial.
Am J Obstet Gynecol 2004;191:1311-7. Crossref
9. To MS, Alfirevic Z, Heath VC, et al. Cervical cerclage for
prevention of preterm delivery in women with short cervix: randomised controlled trial. Lancet 2004;363:1849-53. Crossref
10. Final report of the Medical Research Council/Royal
College of Obstetricians and Gynaecologists multicentre
randomised trial of cervical cerclage. MRC/RCOG
Working Party on Cervical Cerclage. Br J Obstet Gynaecol
1993;100:516-23. Crossref
11. Berghella V, Odibo AO, To MS, Rust OA, Althuisius SM.
Cerclage for short cervix on ultrasonography: meta-analysis
of trials using individual patient-level data. Obstet
Gynecol 2005;106:181-9. Crossref
12. Owen J, Hankins G, Iams JD, et al. Multicenter randomized
trial of cerclage for preterm birth prevention in high-risk
women with shortened midtrimester cervical length. Am J
Obstet Gynecol 2009;201:375.e1-8. Crossref
13. Olatunbosun OA, al-Nuaim L. Turnell RW. Emergency
cerclage compared with bed rest for advanced cervical
dilatation in pregnancy. Int Surg 1995;80:170-4.
14. Althuisius SM, Dekker GA, Hummel P, van Geijn HP;
Cervical incompetence prevention randomized cerclage
trial. Cervical incompetence prevention randomized
cerclage trial: emergency cerclage with bed rest versus bed
rest alone. Am J Obstet Gynecol 2003;189:907-10. Crossref
15. Daskalakis G, Papantoniou N, Mesogitis S, Antsaklis A.
Management of cervical insufficiency and bulging fetal
membranes. Obstet Gynecol 2006;107:221-6. Crossref
16. Cervical cerclage (Green-top Guideline No. 60), May 2011. London: Royal College of Obstetricians and Gynaecologists; 2011.
17. Berghella V, Keeler SM, To MS, Althuisius SM, Rust OA.
Effectiveness of cerclage according to severity of cervical
length shortening: a meta-analysis. Ultrasound Obstet
Gynecol 2010;35:468-73. Crossref
18. To MS, Skentou C, Liao AW, Cacho A, Nicolaides KH.
Cervical length and funneling at 23 weeks of gestation
in the prediction of spontaneous early preterm delivery.
Ultrasound Obstet Gynecol 2001;18:200-3. Crossref

