DOI: 10.12809/hkmj134171
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Peritoneal implantation of ureter in cadaveric renal transplant
CF Tsang, MB, BS, MHKIBSC1;
WK Ma, FRCS, FHKAM (Surgery)2;
FK Cheung, FRCS, FHKAM (Surgery)1
1 Urology Division, Department of Surgery, Princess Margaret Hospital,
Laichikok, Hong Kong
2 Urology Division, Department of Surgery, The University of Hong Kong,
Queen Mary Hospital, Hong Kong
Corresponding author: Dr WK Ma (kitkitma@yahoo.com)
Abstract
We report here a case of complication of peritoneal
implantation of ureter in cadaveric renal transplant.
The patient presented with anuria and delayed graft
function. The diagnosis was suspected upon physical
examination and radiological investigation. The
complication was managed with reimplantation of
the ureter into the bladder and the patient recovered
with good graft function. We discuss this case,
review the literature on this rare complication, and
share our suggestions on how it can be prevented.
Introduction
Oliguria or anuria early after cadaveric renal
transplant (CRT) is not uncommon and can be
related to numerous causes. We report here a rare
case of complication of ureteric implantation in the
peritoneum in CRT causing anuria. Diagnosis was
suspected early on day 1 after operation by clinical
examination and abdominal X-ray (AXR), and
confirmed with non-contrast computed tomography
(CT) of the abdomen and pelvis. The complication
was managed with immediate reimplantation of
the ureter into the bladder and the patient had an
uneventful recovery thereafter with good graft
function. To our knowledge, this is the first reported
case in Hong Kong and the fifth in the world. We
believe the actual incidence is underreported and
would like to share our suggestions on how to avoid
this rare complication.
Case report
A 29-year-old man with Alport’s syndrome developed
end-stage renal failure in 2009 and was started on
intermittent peritoneal dialysis in 2011. His serum
creatinine level and estimated glomerular filtration
rate were 1458 µmol/L and 5.1 mL/min, respectively.
In September 2013, he received CRT from a 60-year-old
man with brain stem death due to haemorrhagic
stroke. The donor’s serum creatinine was 88 µmol/L
and there were no hypotensive episodes or inotrope
infusion before organ harvesting.
The cadaveric right kidney was transplanted
into the right iliac fossa of the recipient, with good
perfusion and turgor after release of vascular clamps.
No urine was noted at cut-end of the graft ureter at
the time of implantation. A needle test to aspirate
pre-filled gentamicin solution from the bladder was
done and extravesical ureteroneocystostomy with
Lich-Gregoir technique was performed with a 7-French, 15-cm long, double J ureteric stent in situ.
The total operating time was 2 hours and 20 minutes;
with cold ischaemic time of 7 hours 41 minutes and
second warm ischaemic time of 33 minutes. The
patient was haemodynamically stable but remained
anuric 12 hours after operation with a serum
creatinine level of 1268 µmol/L. An urgent Doppler
ultrasound of the graft kidney was done and showed
good perfusion of graft with patent renal artery
and vein. Repeated physical examination revealed
a slightly distended abdomen and AXR showed the
distal coil of double J stent above the pelvis level
(Fig a), leading to the suspicion of implantation of the ureter into the peritoneum. Subsequent non-contrast
CT of the abdomen and pelvis confirmed
placement of the ureteric stent outside the bladder
(Fig b and c).
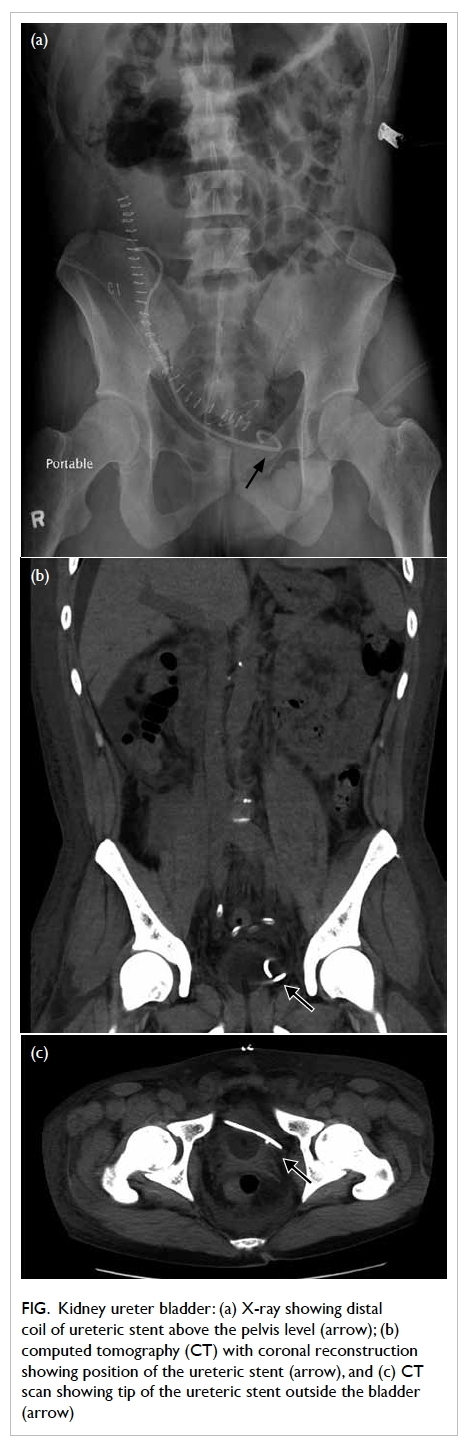
Figure. Kidney ureter bladder: (a) X-ray showing distal coil of ureteric stent above the pelvis level (arrow); (b) computed tomography (CT) with coronal reconstruction showing position of the ureteric stent (arrow), and (c) CT scan showing tip of the ureteric stent outside the bladder (arrow)
Exploration and reimplantation of ureter
were performed immediately. It was noted that the
ureter was implanted into the thickened peritoneum
at a level just above the right upper lateral bladder
wall, with urine draining into the intra-abdominal
cavity. The detrusor layer was thin and not well
developed. The anastomosis was taken down and
ureteroneocystostomy was refashioned with the
same Lich-Gregoir technique. There was immediate
return of good urine output and his serum creatinine
levels improved to 186 µmol/L and 126 µmol/L on
postoperative day 3 and week 4, respectively.
Discussion
Post–renal transplant urological complications are
not uncommon. Commonly reported complications
include thromboembolic events of vascular
anastomosis, acute tubular necrosis, lymph leak,
and urinary reflux. Recent retrospective series
have reported incidence rates of 2.8% to 15.5% of
urological complications after CRT.1 2 3 These are
significantly decreased rates compared with those
in an earlier series after introduction of various
modified techniques of implantation and use of
ureteric stents.1 Peritoneal implantation of ureter
constitutes an incidence of 0.1% to 0.2% only.3 4 Gibbons et al4 reported a case of ureteric implantation
into an ovarian cyst in addition to two cases
into the peritoneum in a series of 1000 CRT recipients.
We believe the actual incidence is underreported,
given the general impression that this complication
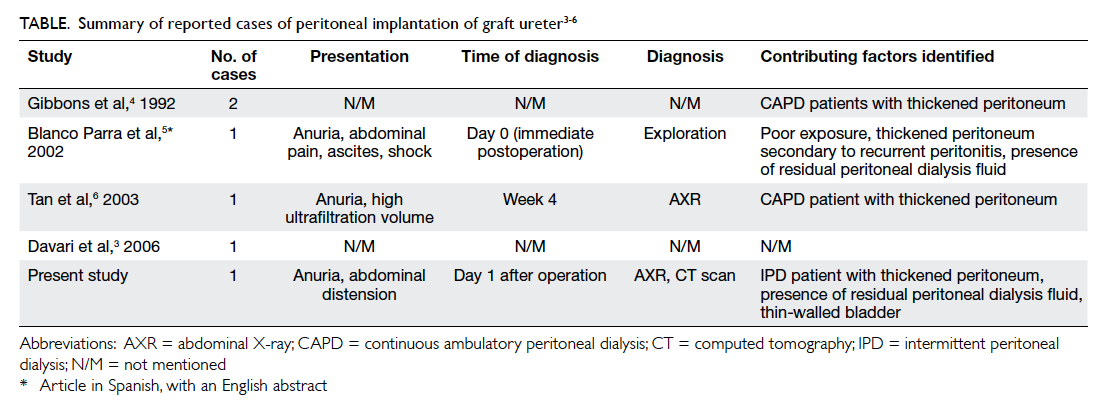
is solely technically related. The Table3 4 5 6 summarises
all reported cases of peritoneal implantation of graft
ureter in the current literature.
All reported patients presented with
postoperative anuria, with one patient developing
ascites, abdominal pain, anuria, and sudden shock.5
Timing of diagnosis had been reported from
immediate postoperation to few weeks later. A high
level of suspicion remains the key for reaching the
diagnosis. Common contributing factors identified
from the literature and our case include long-term
peritoneal dialysis with thickened peritoneum,
and the presence of residual peritoneal fluid
mimicking urine in the bladder. Therefore, this
complication should be suspected in such a patient
with unexplained delayed graft function. Tan et al6
suggested that an unexplained rise in ultrafiltration
volume in transplanted peritoneal dialysis patients
accompanied by a fall in baseline serum creatinine is
highly suggestive of the diagnosis. If ureteric stenting
was employed, imaging such as AXR and CT scan
can help identify the position of the ureteric stent
and confirm the diagnosis. Definitive diagnosis
can only be established upon exploration.
A note of caution on ways to prevent this rare
surgical complication would be more beneficial than
treating it. We suggest several measures to avoid it,
which have not been discussed in previous reports.
Regarding the technique of ureteric implantation, the
classic transvesical Leadbetter-Politano technique
in which two cystostomies are required, is now
replaced by the extravesical Lich-Gregoir technique
which requires only one cystostomy and, hence,
less bladder dissection, shorter ureteral length,
and no interference with native ureteral function.7
This technique, however, may pose challenges in
recipients previously on peritoneal dialysis, as the
peritoneum is thickened due to exposure to dialysis
fluid and episodes of peritonitis, if any. A thickened
peritoneum, with the presence of residual peritoneal
fluid upon incision, can easily be mistaken as the
bladder during transplantation. In our practice, the
bladder is filled with 80 to 100 mL of gentamicin
solution before the procedure and needle aspiration
test is done before ureteric implantation to aid
identification of the bladder. Our case illustrated that
even with these standard precautions, one may not be
able to completely prevent this complication. Tagging
up the extravesical tissue with parallel stay sutures on
both sides of the 2 to 3 cm submucosal tunnel before
creating the cystostomy will help identify the
bladder and peritoneum vigilantly, avoiding shifting
of the incision site to the peritoneum instead of the
bladder wall after the needle test. If the bladder is
scarred and non-compliant due to neuropathic
bladder or prolonged anuria, identification of the
junction between the peritoneum and bladder wall
may become difficult. Preoperative emptying of all
peritoneal dialysis fluid is advocated so that if there
is nil drainage of bladder content after making the
incision, entry into the abdominal cavity instead of
the bladder can be suspected. Direct visualisation of
the urethral catheter should be the best way to ensure
the correct cavity is entered. A larger cystostomy,
however, is often required and is not preferred.
Another innovative trick to pick up the
complication, should the implantation be done
already, is to notice the colour of effluent from the
bladder after ureteroneocystostomy. Any urine or
antibiotic solution drained in the early postoperative
period is at least lightly blood-stained because of the
disturbance to the mucosal edges during cystostomy.
The absence of blood-stained effluent after ureteric
implantation should raise the suspicion that the
peritoneum, and not bladder, was opened.
Our report suggests that peritoneal
implantation of ureter in CRT is not only technically
related but also involves multiple contributing
factors. A high index of suspicion is required to
pick up this complication and meticulous measures
should be adopted to avoid its occurrence.
References
1. Zavos G, Pappas P, Karatzas T, et al. Urological
complications: analysis and management of 1525
consecutive renal transplantations. Transplant Proc
2008;40:1386-90. Crossref
2. Praz V, Leisinger HJ, Pascual M, Jichlinski P. Urological
complications in renal transplantation from cadaveric
donor grafts: a retrospective analysis of 20 years. Urol Int
2005;75:144-9. Crossref
3. Davari HR, Yarmohammadi H, Malekhosseini SA, Salahi
H, Bahador A, Salehipour M. Urological complications in
980 consecutive patients with renal transplantation. Int J
Urol 2006;13:1271-5. Crossref
4. Gibbons WS, Barry JM, Hefty TR. Complications
following unstented parallel incision extravesical
ureteroneocystostomy in 1,000 kidney transplants. J Urol
1992;148:38-40.
5. Blanco Parra M, Calviño J, Romero Burgos R, et al. Ureteral
implantation in peritoneum. Exceptional complication
in renal transplantation [in Spanish]. Actas Urol Esp
2002;26:579-80. Crossref
6. Tan SY, Lim CS, Teo SM, Lee SH, Razack A, Loh CS.
Peritoneal implantation of ureter in a cadaveric kidney
transplant recipient. Med J Malaysia 2003;58:769-70.
7. Zhao JJ, Gao ZL, Wang K. The transplantation operation
and its surgical complications. In: Ortiz J, Andre J, editors.
Understanding the complexities of kidney transplantation.
China: InTech; 2011: 466-7. Crossref