Hong Kong Med J 2014 Dec;20(6):556.e1–3
DOI: 10.12809/hkmj134106
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Pneumonitis and extreme failure to thrive
KL Hon, MD, FCCM1; TF Leung, FRCPCH, FHKAM (Paediatrics)1; YS Yau, MRCP (UK), FHKAM (Paediatrics)2
1 Department of Paediatrics, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, Hong Kong
2 Department of Paediatrics, Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Prof KL Hon (ehon@cuhk.edu.hk)
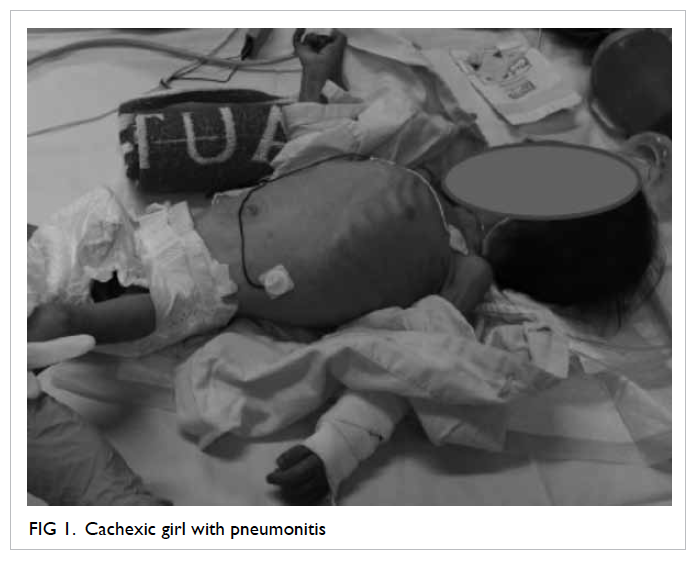
Failure to thrive is an uncommon, challenging,
but important basket of differential diagnoses to
manage in the city of Hong Kong. Diagnosis may
be non-organic or functional. During outbreaks
of avian influenza in Mainland China and MERS/SARI (Middle East respiratory syndrome/severe
acute respiratory illness) coronavirus infection in
the Middle East in early 2013,1 a 27-month-old girl
was brought by her parents to Hong Kong following
a long period of hospitalisation and investigations in
Mainland China for recurrent pneumonia, chronic
diarrhoea, lymphadenopathy, oral candidiasis, and
failure to thrive. Reportedly, no bacterial or viral
pathogens had been found. Antenatal anti–human
immunodeficiency virus (HIV) antibody testing was
negative in the mother. There had been no adverse
reaction to Bacille Calmette-Guérin and routine
immunisations. The child had been exclusively
breastfed and her growth and development were
normal until 9 months of age. The child was admitted
to the paediatric intensive care unit (ICU) of a Hong
Kong hospital for management. She was noted to have
profound failure to thrive with a body weight of only
5 kg (Fig 1). Chest X-ray showed diffuse pneumonitis (Fig 2). She required oxygen supplementation but mechanical ventilation was not needed.
Which of the following investigations will most
likely give the underlying diagnosis?
1. White cell counts and differentials for
congenital neutrophil abnormality
2. Complement C3 and C4 levels for congenital
complement deficits
3. Immunoglobulin A for immunoglobinopathy
4. H7N9, coronavirus, mycoplasma, and
chlamydia serology for atypical pneumonia
5. HIV testing
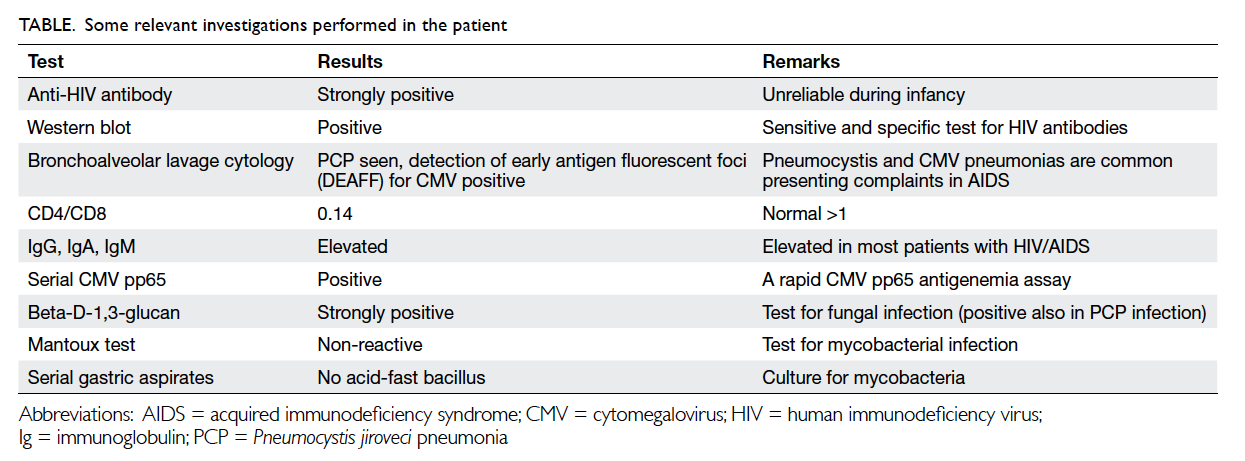
After performing various investigations
(Table), the child tested positive for HIV infection,
confirming that she had acquired immunodeficiency syndrome (AIDS). Computed tomographic
scan of thorax showed pneumonitis (Fig 3).
Treatment for Pneumocystis jiroveci pneumonia
and cytomegalovirus infection was commenced.
Following stabilisation, the child was referred
to a paediatric infectious disease specialist for
continuation of care. Highly active antiretroviral
therapy was started when opportunistic infections
were under control. The child was last seen in June
2014; she was asymptomatic and had been thriving
well.
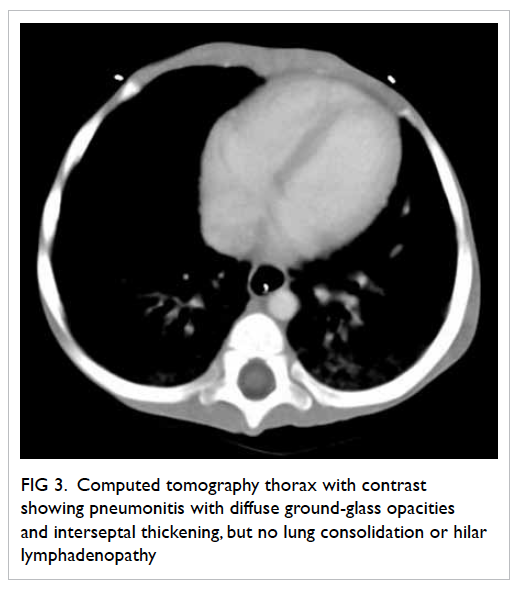
Figure 3. Computed tomography thorax with contrast showing pneumonitis with diffuse ground-glass opacities and interseptal thickening, but no lung consolidation or hilar lymphadenopathy
The parents refused HIV testing but reported
that the child had received blood products after onset
of illness while in the Mainland hospital. Both were
subsequently confirmed HIV positive. Nevertheless,
HIV was most likely to be vertically (mother to child)
transmitted.2 3 4 5 In many areas of the world, HIV/AIDS
has become a chronic rather than an acutely fatal
disease.3 Half of the infants born with HIV die before
2 years of age without treatment.2 3 4 5
Pneumonitis is usually caused by viruses or
atypical pathogens. Since the atypical pneumonitis
epidemic of coronavirus in 2003, Hong Kong and
the rest of the world have heightened surveillance
for outbreaks of atypical pneumonitis with novel
pathogens such as avian or swine influenza, or
coronavirus.1 In the cosmopolitan city of Hong Kong,
paediatric HIV remains a relatively rare diagnosis.
Nevertheless, due to the busy trafficking between
Hong Kong and Mainland China, paediatricians in
Hong Kong must be vigilant of such possibility in
Hong Kong children of Mainland parents. Despite
the misleading history by the parents about negative
screening for HIV, paediatricians at the paediatric
ICU were prompt to arrive at the definitive diagnosis
by requesting HIV testing and considering HIV
infection as a possibility to explain the combination
of pneumonitis and extreme failure to thrive in this
child.
This case is interesting and highlights the
importance of excluding HIV infection in a child with
dual symptoms of recurrent infections and failure to
thrive, even when the mother had tested negative
for HIV antibodies initially; the test may have been
performed in a window period during pregnancy.
Differential diagnoses for failure to thrive
include child abuse and neglect, cystic fibrosis (rare in
Hong Kong), gastroesophageal reflux, growth failure,
growth hormone deficiency, and HIV infection.6 7
The history and physical examination should guide
any laboratory or ancillary testing. Most infants and
children with growth failure related to environmental
factors need very limited laboratory screenings.
This child presented with recurrent infections
and candidiasis. Approach to recurrent infections
resulting in failure to thrive may include HIV testing,
sweat test for cystic fibrosis (if history is relevant),
metabolic and endocrinology screening, tuberculosis
testing, and stool studies.
Basing on disease onset, this is most likely a
case of vertical transmission of HIV. In infants, the
onset of AIDS symptoms can take a few months; in
contrast, it can be many years before adults develop
symptoms of HIV. Thus, repeated HIV testing is very
important to initiate timely treatment in the parents.
References
1. Hon KL. Severe respiratory syndromes: travel history
matters. Travel Med Infect Dis 2013;11:285-7. CrossRef
2. Sepkowitz KA. AIDS—the first 20 years. N Engl J Med
2001;344:1764-72. CrossRef
3. Knoll B, Lassmann B, Temesgen Z. Current status of HIV
infection: a review for non–HIV-treating physicians. Int J
Dermatol 2007;46:1219-28. CrossRef
4. Coutsoudis A, Kwaan L, Thomson M. Prevention of
vertical transmission of HIV-1 in resource-limited
settings. Expert Rev Anti Infect Ther 2010;8:1163-75. CrossRef
5. Thorne C, Newell ML. HIV. Semin Fetal Neonatal Med
2007;12:174-81. CrossRef
6. Nangia S, Tiwari S. Failure to thrive. Indian J Pediatr
2013;80:585-9. CrossRef
7. Hendaus M, Al-Hammadi A. Failure to thrive in infants
(review). Georgian Med News 2013;(214):48-54.