DOI: 10.12809/hkmj134012
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
An outbreak of refrigerant-induced acute hepatitis in Hong Kong
YM Kan, MB, BS, FHKAM (Medicine); CF Lau, MRCP, FHKAM (Medicine); WC Chan, MRCP; WS Chan, MB, BS, FHKAM (Medicine); YM Tung, MRCP, FHKAM (Medicine); CK Loo, MRCP, FHKAM (Medicine)
Department of Medicine and Geriatrics, Kwong Wah Hospital, Yaumatei, Hong Kong
Corresponding author: Dr YM Kan (kanym@ha.org.hk)
Abstract
We report a cluster of acute hepatitis in five air-conditioning
maintenance workers following
accidental exposure to 2,2-dichloro-1,1,1-trifluoroethane (HCFC-123). They presented to us
with complaints of feverishness, generalised malaise,
and epigastric discomfort. Their blood biochemistry
tests were compatible with acute hepatitis. Viral
hepatitis serology, tests for autoimmune hepatitis,
and analyses for drugs and alcohol consumption
were all negative. No focal hepatic lesion was
detected by ultrasound imaging. Percutaneous liver
biopsy samples were taken from two of them. The
patients were managed with supportive treatment.
All had spontaneous, but slow, recovery. Their liver
function tests returned to normal after 4 months and
their outcomes were favourable. Physicians should
be aware of this occupational disease entity.
Case report
A 30-year-old air-conditioning maintenance
worker presented to the Accident and Emergency
Department in September 2010 with complaints
of feverishness, dry cough, general malaise, poor
appetite, and epigastric discomfort for 1 week. His
initial symptoms 1 week before included feverishness
and dry cough. He took paracetamol (500 mg, 4
times a day for 2 days) after consulting a general
practitioner and diagnosed as having acute upper
respiratory tract infection. Two days after visiting the
general practitioner, he developed general malaise,
nausea, and epigastric bloating. He had good past
health and his family history was unremarkable. He
was a social drinker and his last drink was almost 3
months ago. On physical examination, he was febrile
and showed a tinge of jaundice. He was conscious
and well-oriented. His pulse rate was 140 beats/min,
the blood pressure was 130/75 mm Hg, and his body
temperature was 39.3°C. Abdominal examination
showed right upper quadrant tenderness but no
other sign of acute abdomen; Murphy’s sign was
negative.
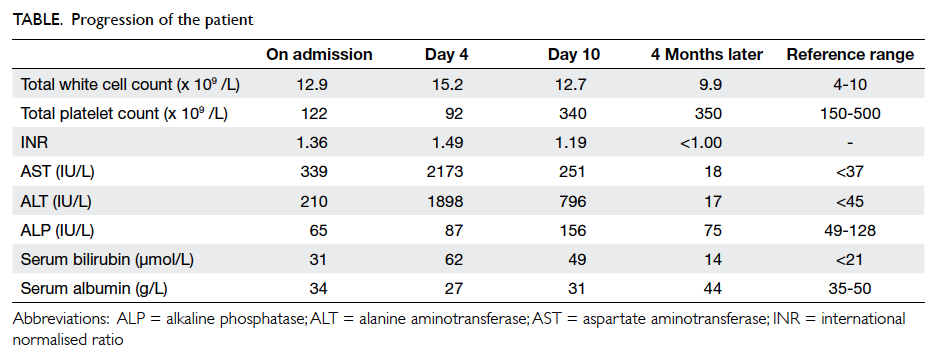
Initial investigation showed elevated blood leukocyte count and mild thrombocytopenia (Table). His liver function tests were deranged and clotting profile was impaired. Serology for hepatitis A, B, C and E, Epstein-Barr virus, and cytomegalovirus was negative. Tests for antinuclear antibodies and
anti-smooth muscle antibodies were also negative.
His toxicology screening was negative, except for
a serum paracetamol level of 77 mmol/L (taken 6 hours after the last dose of paracetamol). Ultrasound
of the abdomen was unremarkable. His liver function tests further deteriorated after admission (Table)
and he remained febrile. Computed tomography of the abdomen was then performed, which revealed
minimal amount of ascites and non-specific pericholecystic fluid collection.
He received intravenous hydration and vitamin
K as supportive treatment for his acute hepatitis. He
remained fully oriented, and his serum ammonia
level was normal.
Upon further enquiry, the patient recalled that he experienced dizziness, drunk feeling, and
unsteady gait after exposure to a refrigerant during maintenance of an air-conditioning system in a
computer server room with an area of around 200 m2. His job was to flush the air-conditioning system and pipeline with a cleansing refrigerant. He said he was not provided with any protective gear. He was, therefore, asked to call his co-workers to see if they
had developed similar symptoms.
Eight workers worked in rotation for 2 weeks.
They were posted to clean and repair the air-conditioning
system in an enclosed area without any
local exhaust ventilation system. In the first week,
they were not provided with any effective protective
gears. They worked for 6 hours a day in the first
week. In the next week, they were provided with
3M face masks and their work duration shortened
to 3 hours a day because they felt dizzy during
work and needed to leave the room for a rest. Thus,
exposure to leaked refrigerant was estimated to be
high in such an enclosed workplace in the absence
of effective protective gear. All workers experienced
headache, dizziness, unsteady gait, and drunk feeling
15 minutes after exposure to the chemical released.
They also had symptoms of dry cough, runny nose,
fever, malaise, and loss of appetite a few days later.
One of them also noticed passing tea-coloured urine
and two had epigastric bloating.
Four among his seven co-workers agreed to
undertake laboratory investigations. They were
all found to have deranged liver function tests
compatible with acute hepatitis. All investigations
including viral hepatitis serology, tests for
autoimmune hepatitis, and analyses for drugs and
alcohol consumption were found to be negative. The
circumstantial evidence, together with the clinical
and laboratory findings, made refrigerant-induced
acute hepatitis highly likely in this group of air-conditioning
maintenance workers.
Percutaneous liver biopsy in one of the affected patients revealed the presence of hepatocytic dropouts and mitotic figures in perivenular distribution. There was moderate lymphocytic infiltrate with scattered eosinophils in the portal
areas with mild bile duct proliferation. Perivenular hepatocytic cholestasis was also evident (Fig). These features, coupled with the clinical history and laboratory findings, were in keeping with a diagnosis of hydrochlorofluorocarbons-related hepatitis.
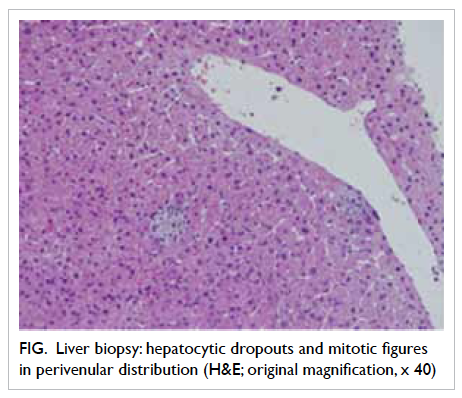
Figure. Liver biopsy: hepatocytic dropouts and mitotic figures in perivenular distribution (H&E; original magnification, x 40)
However, urine analysis of volatile organic hydrocarbons, metabolites of 2,2-dichloro-1,1,1-trifluoroethane (HCFC-123), on day 4 after admission of the index patient, turned out to be negative.
Over the following days, our index patient’s
symptoms improved progressively. His liver function tests, serum platelet count, and prothrombin time
(given by the international normalised ratio) started to improve since day 5 of admission (Table). His coworkers’
symptoms also improved gradually.
Four months later, the health conditions of all the workers were confirmed to be normal. Their liver
function tests had normalised. All had favourable outcomes.
We reported the cases to the Labour Department and the Department of Health since poisoning by halogen derivatives of hydrocarbon of the aliphatic series (ie HCFC-123) is a notifiable occupational disease in Hong Kong.
Discussion
HCFC-123 is a common refrigerant. It is one
of the major substitutes for ozone-depleting
chlorofluorocarbons used mainly as a refrigerant in
chillers for industrial air-conditioning and in other
applications such as foam blowing, cleansing agents,
and industrial solvents. It is a colourless liquid with a
light ether-odour and a boiling point of 27.6°C.1
Acute exposure to HCFC-123 has been shown
to produce severe hepatotoxicity in guinea pigs.2
A single acute exposure to 1000 ppm of HCFC-123 for 4 hours can cause increases in aspartate
aminotransferase and alanine aminotransferase levels compatible with hepatocellular necrosis.
Increased liver weight, focal liver necrosis, induction of peroxisomal activity and hepatocellular adenomas
have been found in subchronic studies in rats and dogs.3
The mechanism of hepatotoxicity of HCFC-123 was believed to be similar to that of 1-bromo-1-chloro-2,2,2-trifluoroethane (halothane). Halothane is metabolised to form reactive trifluoroacetyl
halide intermediates that can react with water to form trifluoroacetyl haptens which result in direct
hepatotoxicity. Since HCFC-123 is metabolised in the same oxidative way as halothane, HCFC-123 exposure might result in direct hepatotoxicity.
In animal studies, the relative concentrations of trifluoroacetyl-protein adducts formed in the liver
after administration of halothane and HCFC-123 were found to be similar.4 Alternatively, in-vitro
metabolic studies of the human liver cytochrome P450 2E1 showed that exposure of human beings
to HCFC-123 might result in higher concentrations of trifluoroacetyl-adducted liver proteins than
those produced by halothane. The development of autoantibodies against P450 2E1 or P58 arising
from immune reactions induced by trifluoroacetyl-adducted liver protein indicates that HCFC-related
hepatotoxicity might also be immune-related.3
Takebayashi et al1 reported a cluster of acute
liver dysfunction among workers exposed to HCFC-123 for less than 5 hours. Nine out of 14 workers
developed impairment of liver function tests and symptoms of poor appetite and abdominal pain.
Alanine aminotransferase level went up to more than 1700 U/L in these patients, but all had a favourable
outcome. By the end of 2 months after HCFC-123 exposure, their liver function tests had returned
to normal. This revealed that the incidence of liver dysfunction after HCFC-123 exposure is high.
Hoet et al3 investigated an epidemic of liver
disease in nine industrial workers who had repeated accidental exposure to a mixture of HCFC-123 and
HCFC-124. The results of this study also showed that repeated exposure of humans to HCFCs can result in
serious liver injury in a high proportion of the exposed population. The liver biopsy showed hepatocellular
necrosis which was prominent in perivenular zone 3, and extended focally across portal tracts
and to centrilobular areas. The hepatocyte dropout was well-developed. The leukocytic inflammatory
infiltrates in the zones of necrosis were mononuclear. Trifluoroacetyl-adducted proteins were detected
in surviving hepatocytes by immunohistochemical staining. Serum autoantibodies against P450 2E1 or
P58, which are associated with halothane hepatitis, were also detected. In our index patient, the presence
of hepatocytic dropouts, increased mitotic figures and eosinophils might suggest acute hepatitis and
liver regeneration after a short period of refrigerant exposure.
At moderate levels of exposure to HCFC-123,
such as in some occupational accidents or prolonged
exposure in poorly ventilated areas, respiratory
effects (cough, dyspnoea, and tachypnoea), central
nervous system effects (dizziness, drowsiness,
weakness, fatigue, numbness, and coma), and gastro-intestinal
upsets are characteristic. Hepatic injury
(with elevated liver enzymes) and rhabdomyolysis
might also rarely occur.5 A retrospective study
showed that workers who had exposure to HCFC-123 experienced symptoms related to the central
nervous system, gastro-intestinal upset, and
irritation of mucous membrane.6 These may include
headache, dizziness, abdominal pain, nausea,
vomiting, dyspepsia, irritating smell, and eye or
throat irritation.6 The prevalence of these symptoms
also increased in the high-exposure group. Moreover,
the degree and prevalence of liver dysfunction were
higher in the high-exposure group.7
Urinary concentration of trifluoroacetic acid
(TFA), which is a major metabolite of HCFC-123, can
be used to determine the degree of HCFC exposure
in air. However, in our case, urinary concentration
of HCFC metabolite was negative. A small-scale
human study found that the concentration of TFA
in the urine peaked at 20 to 30 hours, and returned
to zero by 96 hours post-exposure.8 Since the urine
sample of our index case was collected 4 days after
exposure, a positive test would not be expected.
There is no specific antidotal treatment for
liver injury related to HCFC exposure. Supportive
treatment of liver dysfunction is recommended.
Fortunately, the outcome of HCFC-related liver
dysfunction is usually favourable. All our patients had
spontaneous recovery after cessation of exposure. To
our knowledge, there is no report of death or liver
transplant due to HCFC-123–induced hepatitis.
Poisoning by HCFC exposure is a notifiable
occupational disease in Hong Kong. We reported
this outbreak to the Labour Department and the
Department of Health so that the related parties
could conduct investigations and recommend
appropriate modifications in the relevant working
environment. It is essential to implement strict
measures to prevent HCFC exposure, and physicians
should be aware of the potential toxicities following
HCFC exposure.
References
1. Takebayashi T, Kabe I, Endo Y, et al. Acute liver
dysfunction among workers exposed to 2,2-dichloro-1,1,1-trifluoroethane (HCFC-123): a case report. J Occup Health
1998;40:169-70. CrossRef
2. Marit GB, Dodd DE, George ME, Vinegar A. Hepatotoxicity
in guinea pigs following acute inhalation exposure
to 1,1-dichloro-2,2,2-trifluoroethane. Toxicol Pathol
1994;22:404-14. CrossRef
3. Hoet P, Graf ML, Bourdi M, et al. Epidemic of liver
disease caused by hydrochlorofluorocarbons used as
ozone-sparing substitutes of chlorofluorocarbons. Lancet
1997;350:556-9. CrossRef
4. Harris JW, Poul LR, Martin JL, Anders MW. Tissue acylation
by the chlorofluorocarbon substitute 2,2-dichloro-1,1,1-trifluoroethane. Proc Natl Acad Sci USA 1991;88:1407-10. CrossRef
5. Concise International Chemical Assessment Document
No. 23. Available from: http://www.inchem.org/documents/cicads/cicads/cicad23.htm. Accessed Jun
2014.
6. Takebayashi T, Kabe I, Endo Y, et al. Exposure to
2,2-dichloro-1,1,1-trifluoroethane (HCFC-123) and acute
liver dysfunction: a causal interference. J Occup Health
1998;40:334-8. CrossRef
7. Boucher R, Hanna C, Rusch GM, Stidham D, Swan E,
Vazquez M. Hepatotoxicity associated with overexposure
to 1,1-dichloro-2,2,2-trifluoroethane (HCFC-123). AIHA J
(Fairfax, Va) 2003;64:68-79. CrossRef
8. Tanaka S, Kabe I, Takebayashi T, et al. Environmental and
biological monitoring of 2,2-dichloro-1,1,1-trifluoroethane
(HCFC-123). J Occup Health 1998;40:348-9. CrossRef