DOI: 10.12809/hkmj134090
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Should we perform polypectomy or not?
WY Mak, MB, BS, MRCP (UK); YT Hui, MRCP (UK), FHKAM (Medicine); Jodis TW Lam, FHKAM (Medicine), FRCP (Edin)
Department of Medicine, Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Dr WY Mak (mwy612@ha.org.hk)
A 78-year-old woman, with a known history of
rheumatoid arthritis, complained of dizziness and
was found to have iron-deficiency anaemia with a
haemoglobin level of 105 g/L in January 2013. She
was on treatment with methotrexate, sulphasalazine,
and non-steroidal anti-inflammatory medications.
Oesophagogastroduodenoscopy performing for
anaemia showed a linear ulcer over the anterior
wall of the stomach. Subsequent colonoscopic
examination was done to look for the cause of iron-deficiency
anaemia and revealed a 1 cm–long everted
umbilicated polypoid lesion in the ascending colon
(Fig a). On close examination of the lesion using
narrow band imaging (NBI), the mucosal pattern was
normal with no endoscopic features of adenomatous
polyp. Upon further air insufflation, the everted lesion
invaginated and turned into a diverticulum (Fig b).
Thus, a diagnosis of an inverted colonic diverticulum
(ICD) was made.
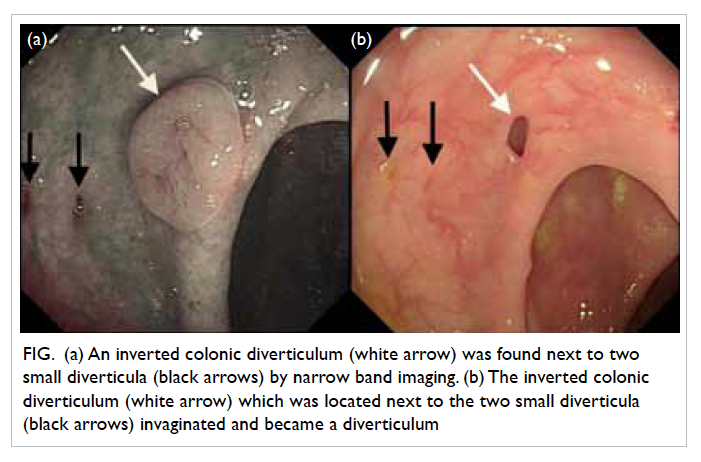
Figure. (a) An inverted colonic diverticulum (white arrow) was found next to two small diverticula (black arrows) by narrow band imaging. (b) The inverted colonic diverticulum (white arrow) which was located next to the two small diverticula (black arrows) invaginated and became a diverticulum
Inverted colonic diverticulum is a rare
condition. A retrospective analysis of colonic
examinations showed that the prevalence was only
0.7%.1 The majority (approximately 75%) of ICDs were
found in the sigmoid colon.1 Right-sided colonic ICD,
as illustrated in our case, was not commonly seen.
An ICD is typically described as a broad-based lesion
with normal overlying mucosa lying within a bed of
colonic diverticula. It can resemble an adenomatous
polyp of variable size. It is essential to correctly
diagnose this condition as inadvertent ‘polypectomy’
may potentially lead to bowel perforation. Currently,
there are several endoscopic strategies that can help
in distinguishing ICD from an adenomatous polyp.
Firstly, gentle air insufflation may cause evertion of inverted diverticula. In some cases, a jet of water may
be used to flatten the lesion.2 Secondly, probing the
lesion gently with a biopsy forceps will show a soft
lesion with easy indentation. Interestingly, it was
recently suggested that the presence of Aurora rings
can support the diagnosis of an ICD.3 Aurora rings are
described as concentric rings surrounding the base
of an ICD which can be demonstrated with the use
of NBI or chromoendoscopy. If doubt exists, double-contrast
barium enema or computed tomography
colonography may help to distinguish between the
two entities. Endoscopic ultrasound (EUS) has also
been used to characterise such lesions. In a report,
the diagnosis of sigmoid ICD was made by the EUS
features of a thickened but normal-looking colonic
mucosa in a polyp-like lesion.4 Most importantly,
endoscopic removal and biopsy of ICD should be
avoided as potentially fatal bowel perforation may
occur.5
In conclusion, ICD is an uncommon but
important clinical finding. Endoscopists should
always be aware of the possibility of ICD during
colonoscopic examination as inadvertent biopsy
or resection of these lesions can lead to potentially
serious complications.
References
1. Merino R, Kinney T, Santander R, et al. Inverted colonic
diverticulum: an infrequent and dangerous endoscopic
finding [abstract]. Gastrointest Endosc 2005;61:AB257. CrossRef
2. Cappell MS. The water jet deformation sign: a novel
provocative colonoscopic maneuver to help diagnose an
inverted colonic diverticulum. South Med J 2009;102:295-8. CrossRef
3. Share MD, Avila A, Dry SM, Share EJ. Aurora rings: a
novel endoscopic finding to distinguish inverted colonic
diverticula from colon polyps. Gastointest Endosc
2013;77:308-12. CrossRef
4. Yoshida M, Kawabata K, Kutsumi H, et al. Polypoid
prolapsing mucosal folds associated with diverticular
disease in the sigmoid colon: usefulness of colonoscopy and
endoscopic ultrasonography for diagnosis. Gastrointest
Endosc 1996;44:489-91. CrossRef
5. D’Ovidio V, Di Camillo M, Pimpo MT, Meo D, Vernia
P, Caprilli R. An unusual complicated polypectomy and
inverted colonic diverticula. Colorectal Dis 2010;12:491-2. CrossRef

