Hong Kong Med J 2014;20:139–44 | Number 2, April 2014 | Epub 14 Mar 2014
DOI: 10.12809/hkmj134134
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Public lacks knowledge on chronic kidney disease: telephone survey
KM Chow, MB, ChB, FRCP;
CC Szeto, MD, FRCP;
Bonnie CH Kwan, MB, BS, FRCP;
CB Leung, MB, ChB, FRCP;
Philip KT Li, MD, FRCP
Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, Hong Kong
Corresponding author: Dr KM Chow (Chow_Kai_Ming@alumni.cuhk.net)
Abstract
Objectives: To examine knowledge of chronic
kidney disease in the general public.
Design: Cross-sectional telephone survey.
Setting: Hong Kong.
Participants: Community-dwelling adults who
spoke Chinese in Hong Kong.
Results: The response rate was 47.3% (516/1091)
out of all subjects who were eligible to participate.
The final survey population included 516 adults
(55.6% female), of whom over 80% had received a
secondary level of education or higher. Close to
20% of the participants self-reported a diagnosis of
hypertension. Few (17.8%) realised the asymptomatic
nature of chronic kidney disease. Less than half of
these individuals identified hypertension (43.8%) or
diabetes (44.0%) as risk factors of kidney disease.
Awareness of high dietary sodium as a risk factor for
chronic kidney disease was high (79.5%).
Conclusions: The public in Hong Kong is poorly
informed about chronic kidney disease, with
major knowledge gaps regarding the influence of
hypertension on kidney disease. We are concerned
about the public’s unawareness of hypertension
being a risk factor for kidney disease. Future health
education should target areas of knowledge deficits.
New knowledge added by this
study
- Despite the wealth of evidence for hypertension being a risk factor of chronic kidney disease, less than half the general public in Hong Kong are aware of the association.
- Only 17.8% of respondents in a telephone survey recognised the asymptomatic nature of chronic kidney disease.
- There is an urgent need for better public education focused on risk factors of chronic kidney disease, so as to improve the chance of opportunistic screening for kidney disease.
Introduction
Several recent surveys have documented low levels
of knowledge about chronic kidney disease among
patients.1 2 3 In a US survey of almost 400 patients at
all stages of chronic kidney disease not on dialysis,1
more than half reported no or little knowledge about
the symptoms of kidney disease, or medications that
can be harmful to the kidney. Furthermore, awareness
of chronic kidney disease in the community is low,
and limited knowledge about this disorder in the
general public poses an even more significant hurdle
in disease prevention. A large representative sample
of Chinese adults yielded a 10.8% prevalence of
chronic kidney disease, whereas only 12.5% of them
were aware they had this condition.4
Data on general public knowledge on chronic
kidney disease are essential to understanding
knowledge gaps and formulating education programmes. Without knowing knowledge gaps,
public health education programmes cannot
be planned in a strategic manner. To examine
knowledge on kidney disease and identify areas
of misconception in the general population, we
conducted a cross-sectional telephone survey in
Hong Kong. We anticipated that assessment of
knowledge gaps would be important to improve the
public education and has the potential of preventing
chronic kidney disease.5
Methods
Between 4 and 7 March 2013, we carried out
a telephone survey of adults in Hong Kong.
Respondents were required to be adults aged 18
years or older, and to speak Cantonese or Mandarin.
The sampling method entailed selecting telephone
numbers randomly from the latest Hong Kong Residential Telephone Directories (both Chinese
and English versions) as seed numbers. In order
to include unpublished telephone numbers, the
last two digits of the selected seed numbers were
replaced by two new and random digits generated by
computer. When telephone contact was established
successfully with a target household, only a person
aged 18 years or more was chosen for an interview.
When there was more than one eligible subject in
the household, only one was chosen for the survey
(by convenience).
As a result, a total of 11 600 telephone calls
were made, and 2659 families were successfully
contacted. Ineligible contacts included invalid lines,
non-residential lines, voice machines, facsimile
numbers, and language problems. Of those successfully
connected, 1383 cut the line before confirmation,
562 targeted persons refused the interview, 185
families had no eligible participant, and 13 were not
interviewed because the target participants were not
available. Finally, a total of 516 respondents were
successfully interviewed, yielding a response rate of
47.3% (out of the 1091 eligible families contacted).
Trained interviewers from Hong Kong
Institute of Asia-Pacific Studies administered the
survey by telephone, and each interview lasted
10 minutes. Participants were asked close-ended
questions on general knowledge about chronic
kidney disease. The survey domains and instrument
were developed to assess knowledge of the
respondents on the general function of the kidneys,
causes and symptoms of chronic kidney disease,
and management and treatment of kidney disease.
Some of the multiple-choice questions were refined and modified from a questionnaire previously tested
in Singapore.2 Pre-testing of the questionnaire
was carried out on members of the public through
focus group discussions. The questionnaire was
tested for face validity as well as content saturation.
The finalised questionnaire was administered to patients at primary care public medical centres in
persons with no known chronic kidney disease.2 We
also collected demographic information (age, sex,
education level, and self-reported health conditions)
from the respondents.
Statistical analyses were performed using the
Statistical Package for the Social Sciences (Windows
version 16.0; SPSS Inc, Chicago [IL], US). Numerical
data were expressed as mean ± standard deviation.
Percentages were compared by means of Fisher’s
exact test or Chi squared test. A two-tailed P value
of <0.05 was regarded as statistically significant.
Results
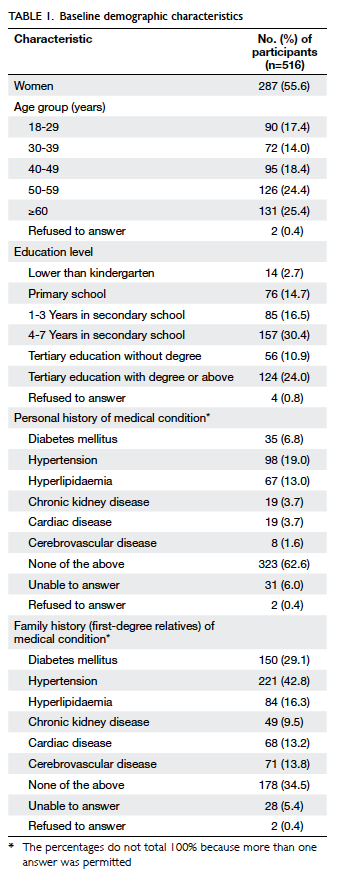
Table 1 lists the characteristics of the respondents,
who had a median age of 50 years. Over 80% of them
had received a secondary or higher level of education.
Only 3.7% (n=19) of the respondents were aware of
any personal history of chronic kidney disease, and
19.0% (n=98) admitted they had hypertension. A
family history of hypertension and diabetes was
reported in 42.8% and 29.1% of the respondents,
respectively.
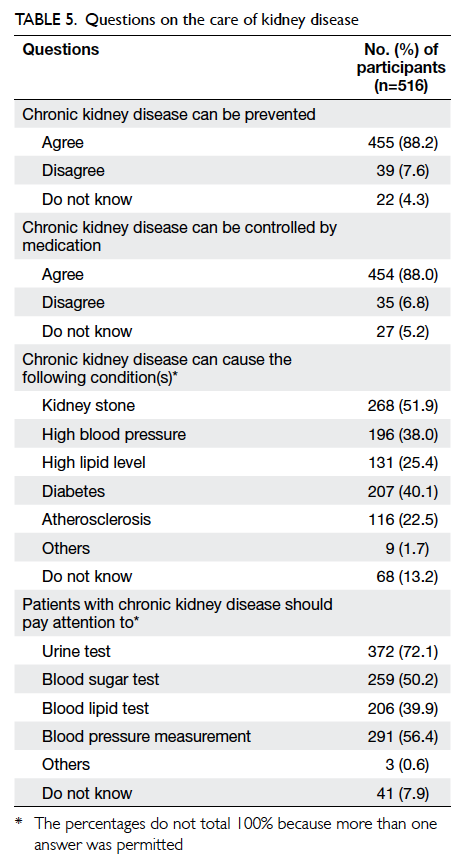
Table 2 lists the answers to questions on the
function of the kidneys and general knowledge on
kidney disease. Only 27.9% of the respondents knew
that only one kidney is needed for a human being
to lead a normal life, although most (84.7%) were
aware of the kidney’s function. Most respondents
(79.5%) listed high dietary sodium as a risk factor
for chronic kidney disease, but hypertension and
diabetes were selected less frequently. Less than half
of the respondents knew that hypertension (43.8%)
and diabetes (44.0%) can cause kidney disease, but
52.7% answered that frothy urine can be an early
manifestation of kidney disease. However, only
17.8% correctly identified the asymptomatic nature
of chronic kidney disease.
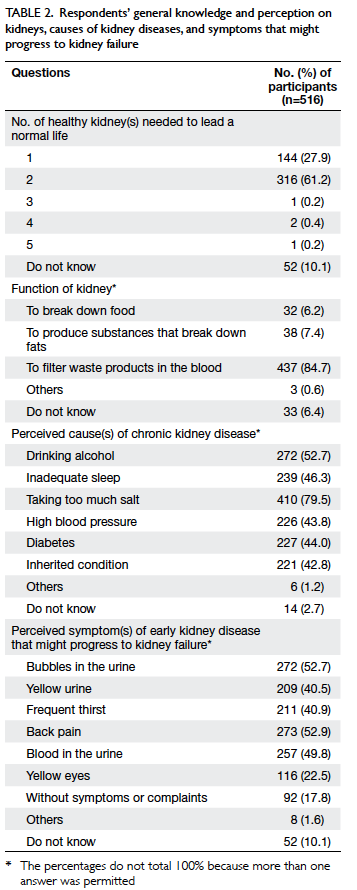
Table 2. Respondents’ general knowledge and perception on kidneys, causes of kidney diseases, and symptoms that might progress to kidney failure
We further analysed factors that are associated
with a lack of knowledge that hypertension can cause
chronic kidney disease. There were no significant
differences between groups in terms of age and
gender. On the other hand, respondents with higher
levels of education were more likely to self-report
a personal or family history of hypertension and a
personal history of diabetes mellitus (Table 3), and
were more likely to know that hypertension is a
cause of kidney disease. Similarly, a higher education
level and a personal history of diabetes mellitus were
associated with better knowledge about the causal
relationship between diabetes and chronic kidney
disease (Table 4).
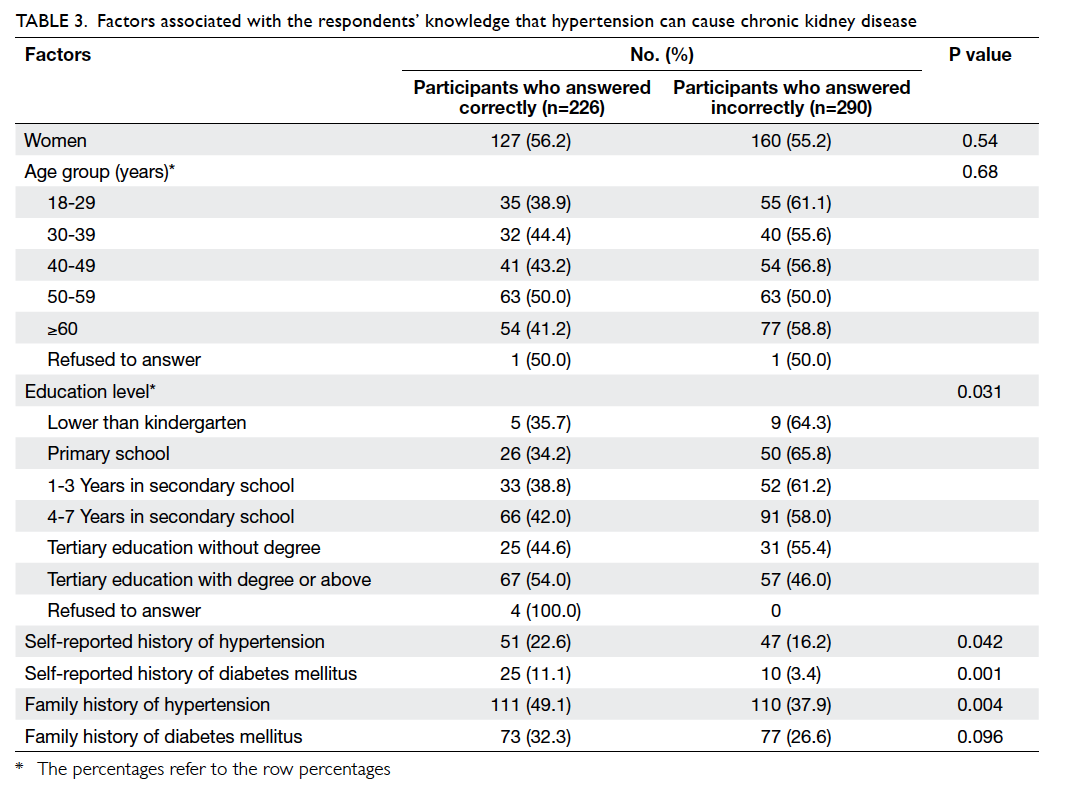
Table 3. Factors associated with the respondents’ knowledge that hypertension can cause chronic kidney disease
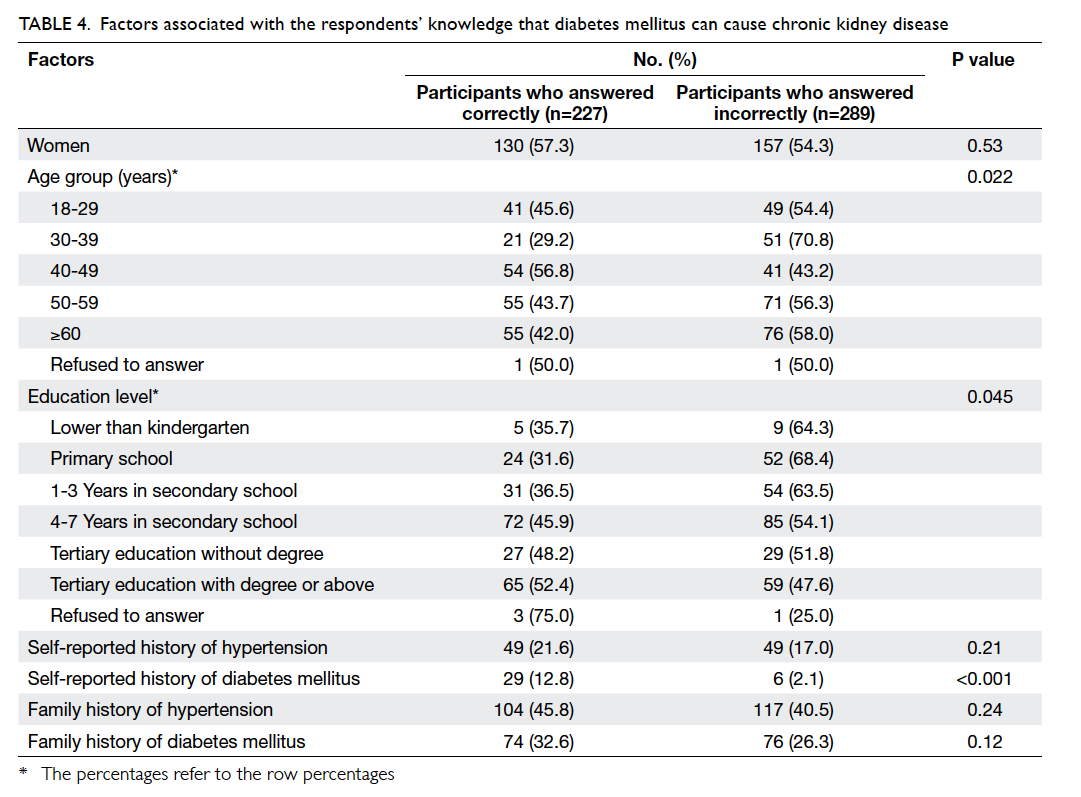
Table 4. Factors associated with the respondents’ knowledge that diabetes mellitus can cause chronic kidney disease
Table 5 shows the perceived sequelae of
chronic kidney disease. Overall, more than 80%
of respondents said that kidney disease could be
prevented, and could be controlled by medication.
On the other hand, over 60% of them did not identify
hypertension as a complication of chronic kidney disease. Furthermore, nearly half (43.6%) of the
subjects did not know the importance of checking
the blood pressure in patients with chronic kidney
disease, and less than a quarter (22.5%) believed
that chronic kidney disease can increase the risk of atherosclerosis.
Discussion
The main findings from this survey define the key
knowledge gaps concerning the kidney disease. In
particular, the public in Hong Kong is unfamiliar with
the relationship between hypertension and kidney
disease. Almost four in five knew that high dietary
sodium intake can be associated with kidney disease,
but the risk of hypertension causing kidney disease
was underestimated. Only 43.8% of respondents
considered hypertension as a factor that increases
the risk of kidney disease, and 43.6% did not perceive
the need for patients with kidney disease to have
blood pressure monitored. Another key issue was
that close to 20% of the respondents self-reported
a diagnosis of hypertension. Quantifying such
knowledge deficit indicates that high blood pressure
is relatively neglected and provides useful input for
future public education.
Low public awareness of hypertension as a cause of kidney damage has been demonstrated in
other national surveys. A cross-sectional survey
of 1435 primary care patients without kidney
disease in Singapore reported that only 51.2% knew
that chronic kidney disease could be caused by
diabetes, hypertension, and hereditary conditions.2
Overall, the public remains relatively unaware of
the two leading causes of chronic kidney disease
(hypertension and diabetes) in all developed and
many developing countries. Similar to hypertension,
the rising worldwide prevalence of diabetes and
the lack of knowledge about its relationship with
chronic kidney disease are of great concern.6 The
AusDiab study involving a survey of 852 Australian
subjects from the general population found an even
lower level of understanding of hypertension; 25.7%
of respondents reported poor diet as a cause of
kidney disease but only 2.8% identified hypertension
as risk factor.7 According to a cross-sectional survey
of 2017 African Americans, 12.1% knew that having
hypertension was a risk factor for kidney disease.8 A
strikingly prevailing theme among all these surveys
(including ours) was the tendency of the public
to name aspects of lifestyle instead of medical
conditions as risk factors for kidney disease. In other
words, there is relatively higher awareness of dietary
risk factors for kidney disease compared with high-risk
medical condition, notably hypertension. This
was affirmed in a community-based qualitative
exploratory analysis on kidney disease knowledge
among rural populations in the US.9 Analysis of the
audiotape scripts identified a representative theme:
lifestyle choices, such as drinking sodas and diet,
were routinely brought up as a means to explain the
occurrence of kidney disease.9
More accurate and prioritised knowledge of
kidney disease risk factors will lead to better disease
awareness and increase chances of opportunistic
screening. It is of concern that the general public
underestimates the importance of blood pressure
control. The most recent Global Burden of Disease
Study launched by the World Bank and the World
Health Organization announced that high blood
pressure has shifted from the fourth to the top risk
factor in terms of the global disability-adjusted
life-years.10 Inability to consider hypertension
as the risk factor for kidney disease implies that
many subjects perceive themselves at lower risk
of kidney disease, do not get screened, and have
less concern for certain health behaviours. In fact,
insufficient knowledge can drive the problem of
antihypertensive medication non-adherence, which
has recently been confirmed to confer an increased
risk of end-stage renal disease. Using the Canadian
health insurance databases of 185 476 patients with
hypertension, among those who were in possession
of their prescribed medication, more than 80% of the
time had a 33% lower risk of end-stage renal disease.11 Targeting health care professionals is probably not
the utmost concern, because only 3.4% of primary
care physicians failed to recognise hypertension
as a risk factor for chronic kidney disease according
to a cross-sectional representative survey of
primary care providers in the community.12 On the
other hand, targeting public education to prevent
asymptomatic renal disease should be explored.
We have previously confirmed a high frequency of
abnormal blood pressure readings and subclinical
urinalysis abnormalities (17.4%) in a screening
programme of 1201 apparently healthy community-dwelling
adults in Hong Kong.13 A successful public
educational programme should therefore aim at
better informing the asymptomatic nature of early
chronic kidney disease, and address the risk factors
such as hypertension. For this reason, the role of
hypertension in kidney disease was chosen as the
key message for World Kidney Day 2009.14
One important limitation of our survey
was that individual-level data of subjects who
declined the interview were missing. The fact that
we could not compare the baseline characteristics
of participants and those who declined raises the
possibility of response bias. Response bias implies
that the small percentage of subjects who responded
could have differed systematically from the majority
who did not answer telephone calls or cut the line
before confirmation. Moreover, the sample of
respondents in this residential telephone registry
may not be generalised to other populations, such
as those who mostly use mobile phones. Thus,
requirement of a landline telephone in order to be
sampled by the current random digit-dial telephone
survey raised the possibility of non-coverage bias.
Furthermore, our survey tool was not developed
through experts in health literacy and psychometric
analyses, and the questions were not field-tested
and validated. We are aware of better constructed
chronic kidney disease–specific knowledge survey
tools in other populations with known kidney
disease.15 Future research to assess kidney disease
knowledge in the Chinese community should follow
similar developments to improve the reliability and
validity of questionnaires. In addition, the diagnosis
of hypertension and chronic kidney disease in our
telephone survey respondents was not validated,
instead it was based entirely on self-reporting.
Conclusions
The general public in Hong Kong did not recognise
that the kidney is both a cause and victim of
hypertension. Public health education efforts that
target knowledge of kidney disease risk factors may
help reduce the burden of kidney disease.
Declaration
No conflicts of interest were declared by authors.
References
1. Wright Nunes JA, Wallston KA, Eden SK, Shintani AK, Ikizier TA, Cavanaugh KL. Associations among perceived and objective disease knowledge and satisfaction with physician communication in patients with chronic kidney disease. Kidney Int 2011;80:1344-51. CrossRef
2. Chow WL, Joshi VD, Tin AS, et al. Limited knowledge of chronic kidney disease among primary care patients—a cross-sectional survey. BMC Nephrol 2012;13:54. CrossRef
3. Tan AU, Hoffman B, Rosas SE. Patient perception of risk factors associated with chronic kidney disease morbidity and mortality. Ethn Dis 2010;20:106-10.
4. Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 2012;379:815-22. CrossRef
5. Collins AJ, Gilbertson DT, Snyder JJ, Chen SC, Foley RN. Chronic kidney disease awareness, screening and prevention: rationale for the design of a public education program. Nephrology (Carlton) 2010;15(Suppl 2):37-42. CrossRef
6. Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet 2013;382:260-72. CrossRef
7. White SL, Polkinghorne KR, Cass A, Shaw J, Atkins RC, Chadban SJ. Limited knowledge of kidney disease in a survey of AusDiab study participants. Med J Aust 2008;188:204-8.
8. Waterman AD, Browne T, Waterman BM, Gladstone EH, Hostetter T. Attitudes and behaviors of African Americans regarding early detection of kidney disease. Am J Kidney Dis 2008;51:554-62. CrossRef
9. Jennette CE, Vupputuri S, Hogan SL, Shoham DA, Falk RJ, Harward DH. Community perspectives on kidney disease and health promotion from at-risk populations in rural North Carolina, USA. Rural Remote Health 2010;10:1388.
10. Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med 2013;369:448-57. CrossRef
11. Roy L, White-Guay B, Dorais M, Dragomir A, Lessard M, Perreault S. Adherence to antihypertensive agents improves risk reduction of end-stage renal disease. Kidney Int 2013;84:570-7. CrossRef
12. Lea JP, McClellan WM, Melcher C, Gladstone E, Hostetter T. CKD risk factors reported by primary care physicians: do guidelines make a difference? Am J Kidney Dis 2006;47:72-7. CrossRef
13. Li PK, Kwan BC, Leung CB, et al. Prevalence of silent kidney disease in Hong Kong: the screening for Hong Kong Asymptomatic Renal Population and Evaluation (SHARE) program. Kidney Int Suppl 2005;94:S36-40. CrossRef
14. Bakris GL, Ritz E. The message for World Kidney Day 2009: hypertension and kidney disease: a marriage that should be prevented. Nephrology (Carlton) 2009;14:49-51. CrossRef
15. Wright JA, Wallston KA, Elasy TA, Ikizler TA, Cavanaugh KL. Development and results of a kidney disease knowledge survey given to patients with CKD. Am J Kidney Dis 2011;57:387-95. CrossRef