Hong Kong Med J 2014;20:121–5 | Number 2, April 2014 | Epub 7 Oct 2013
DOI: 10.12809/hkmj133988
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Lymphoscintigraphy in the evaluation of lower extremity lymphedema: local experience
MC Lam, MB, ChB; WH Luk, FRCR, FHKAM (Radiology); KH Tse, MB, ChB
Department of Radiology and Organ Imaging, United Christian Hospital, Kwun Tong, Hong Kong
Corresponding author: Dr MC Lam (karrylam1121@gmail.com)
Abstract
Objective: To review our local experience in the use
of lymphoscintigraphy to evaluate lymphedema of
the lower extremities.
Design: Retrospective case series.
Setting: A local regional hospital in Hong Kong.
Patients: Images and records of all patients
presenting to our hospital with suspected lower
limb lymphedema from 1998 to 2011 for whom
lymphoscintigraphy was performed were reviewed.
Main outcome measures: Lymphoscintigraphy
findings and clinical outcomes.
Results: In all, 24 patients (13 males and 11
females; age range, 14-83 years) had undergone
lymphoscintigraphy for suspected lower limb
lymphedema. Eight cases were confirmed positive, including one with lymphangiectasia, five with
lymphatic obstruction, and two with lymphatic
leakage. No complication was encountered.
Conclusion: Lymphoscintigraphy is safe and
effective for the evaluation of lymphedema in lower
extremities.
New knowledge added by this
study
- Our local experience confirmed the diagnostic value of lymphoscintigraphy in the evaluation of lymphedema of lower extremities.
- Prompt diagnosis of lymphedema is crucial as effective treatment may be available. Lymphoscintigraphy aids the diagnosis of lymphedema, identification of causes and the approximate site of lymphatic obstruction, and should therefore be considered under appropriate clinical settings.
Introduction
Lymphedema is the accumulation of tissue fluid in
the interstitial spaces, resulting from anatomical
or functional lymphatic obstruction or defective
lymphatic drainage.1 Local data about the
prevalence of this condition are not available, but
it is estimated to affect 2 to 3 million inhabitants
in the US.2 Lymphoscintigraphy has emerged and
become the standard investigation in the evaluation
of lymphedematous extremities. We reviewed our
experience in the use of lymphoscintigraphy for this
purpose in a single regional hospital.
Methods
We retrospectively identified all the cases with
suspected lower limb lymphedema referred for
lymphoscintigraphy from 1998 to 2011. Case records
and imaging studies were reviewed.
Imaging techniques
Studies conducted from 1998 to 2007 were performed
with a single detector system (Picker Prism 1000; Picker International, Cleveland [OH], US). Studies
performed after 2007 were performed with a single
photon emission computed tomography–computed
tomography imaging system (Siemens Symbia T6;
TruePoint SPECT CT, Siemens Medical Solutions,
Illinois, US). The interdigital web space between the
first and second digits on the patient’s lower limbs
was anaesthetised with local anaesthetic cream,
and subsequently 0.5 mCi of Technetium-99m
filtered sulphur colloid (through 0.22 micron filter)
was injected into the preanaesthetised interdigital
web spaces, creating a wheal. About 1 to 2 minutes
after the injection, patients were encouraged to
exercise their toes. Two-phase dynamic images were
obtained at 5 minutes (from toes to knee) and 10
minutes (from knee to groin). Anterior whole-body
scans were obtained at 15, 30, 45, and 60 minutes.
Delayed 4-hour and 24-hour whole-body scans were
obtained whenever deemed necessary.
Results
There were 24 patients with suspected lymphedema
of lower extremities who had undergone lymphoscintigraphy. The patients were aged 14 to 83
(mean, 58) years; 13 were males and 11 were females.
Apart from mild pain during injection, all patients
tolerated the examination well without any serious
complication.
Lymphoscintigraphy findings
A predictable sequence should be seen in patients
with normal lymphatic anatomy and function. In the
lower limb, there should be symmetrical migration
of radionuclide through discrete lymph vessels (3-5 per calf and 1-2 per thigh). Ilioinguinal nodes should
be visualised within 1 hour. Typically, 1 to 3 popliteal
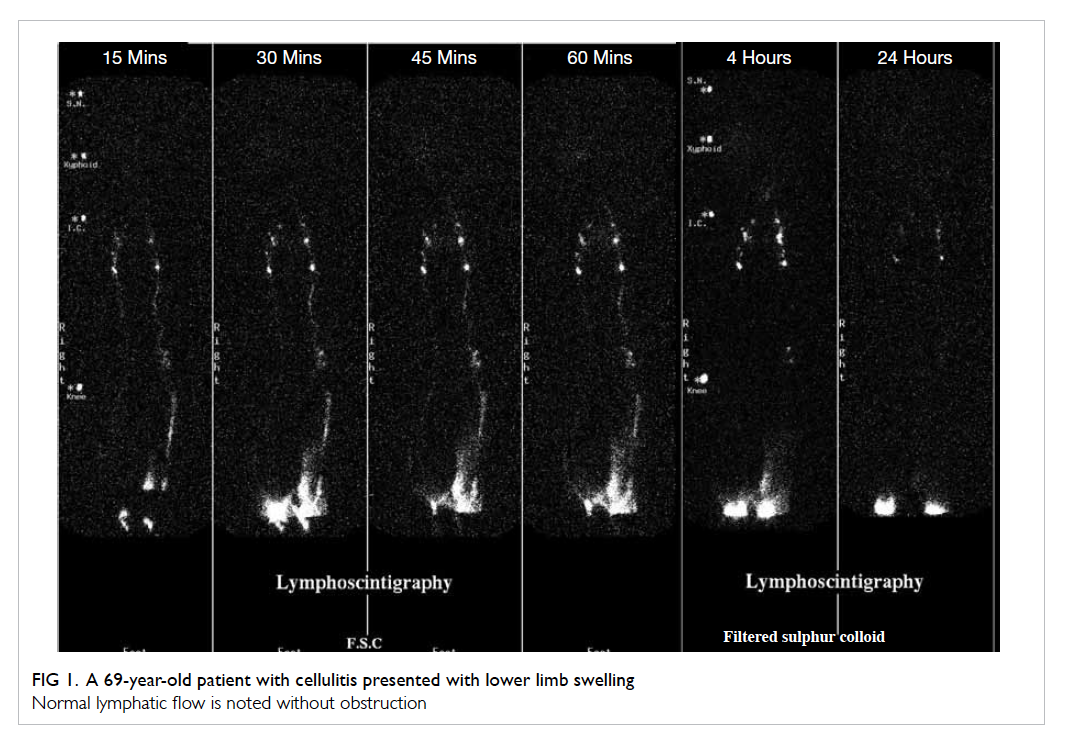
nodes and 2 to 10 ilioinguinal nodes are seen. Figure 1 shows a normal lymphoscintigraphic examination
of the lower limbs.
Abnormal lymphoscintigraphy scans manifest
a wide range of findings, including interruption of
lymphatic flow, collateral lymph vessels, dermal
backflow, reduced number of lymph nodes, dilated
lymphatics, delayed or non-visualisation of lymph
nodes and even the lymphatic systems.
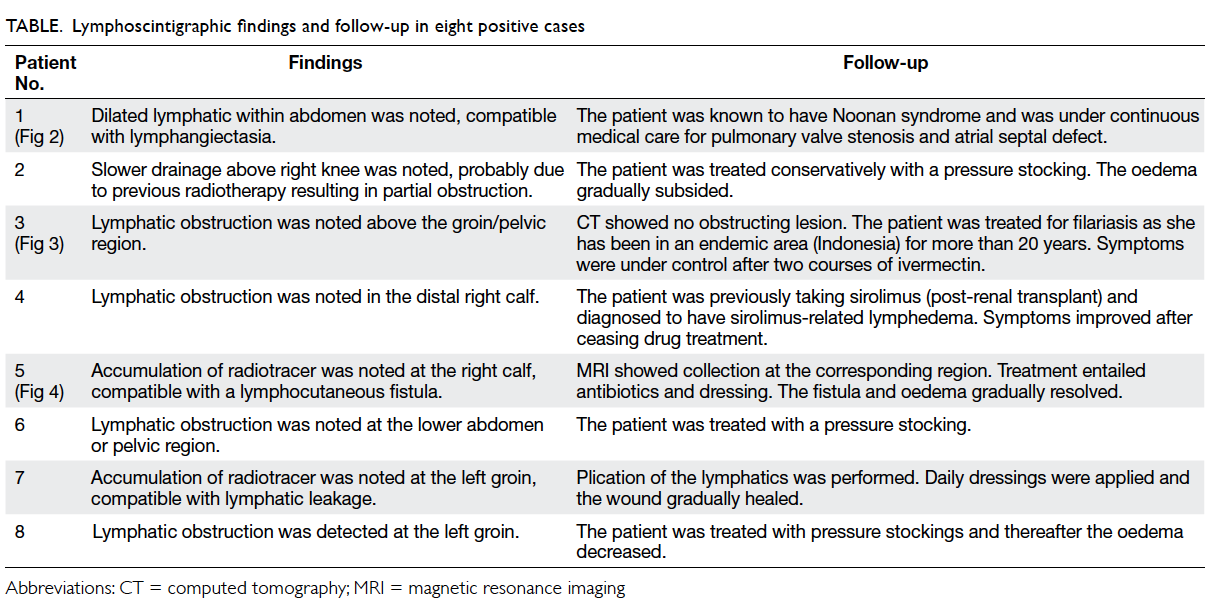
There were eight patients confirmed to be
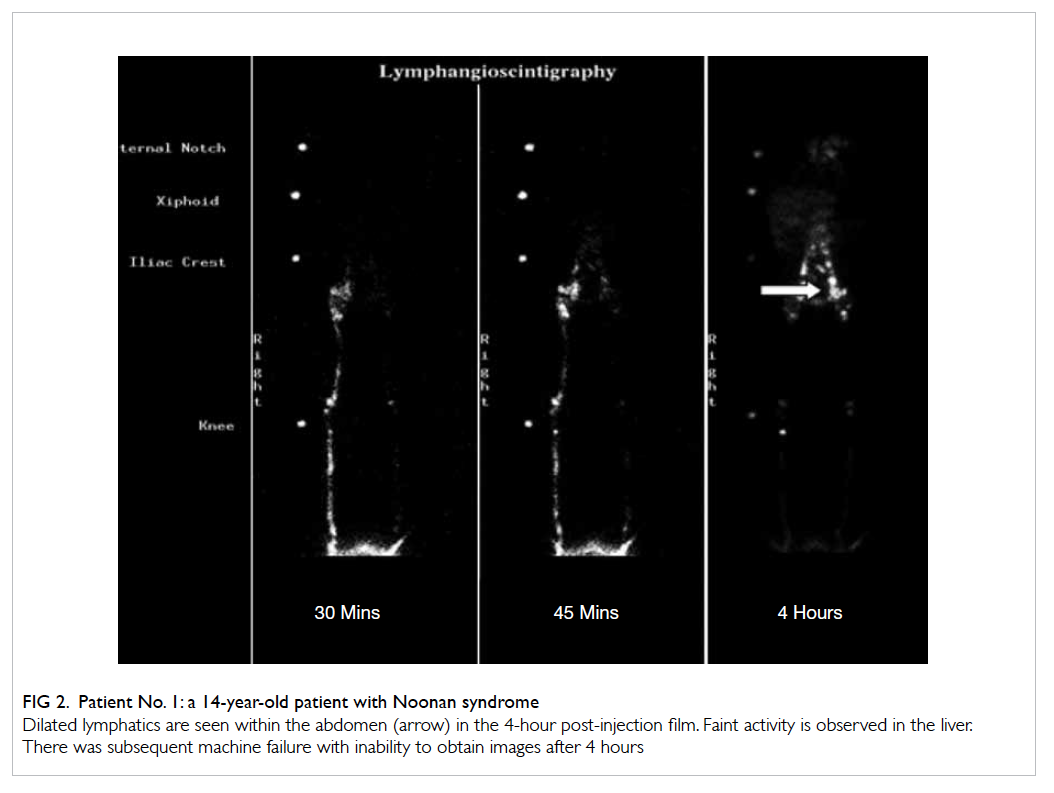
positive for lymphedema. These included one
with lymphangiectasia (Fig 2), five with lymphatic
obstruction (Fig 3), and two with lymphatic
leakage (Fig 4). The Table summarises the
lymphoscintigraphic findings and follow-up data on
these eight cases.
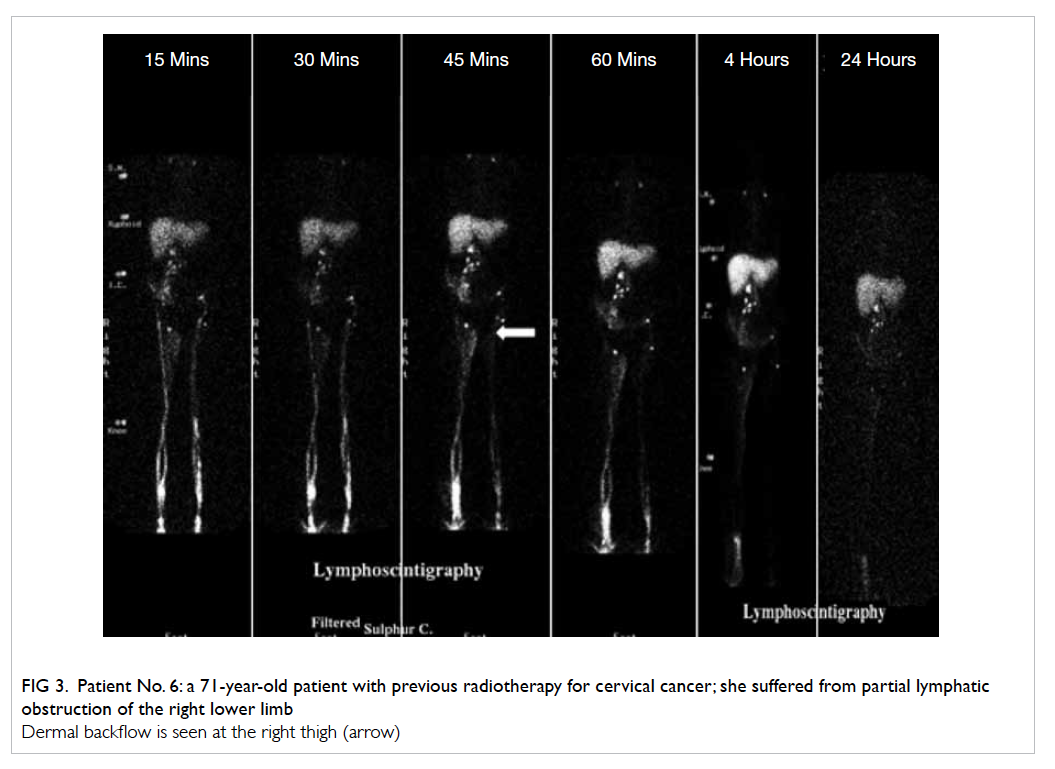
Figure 3. Patient No. 6: a 71-year-old patient with previous radiotherapy for cervical cancer; she suffered from partial lymphatic obstruction of the right lower limb
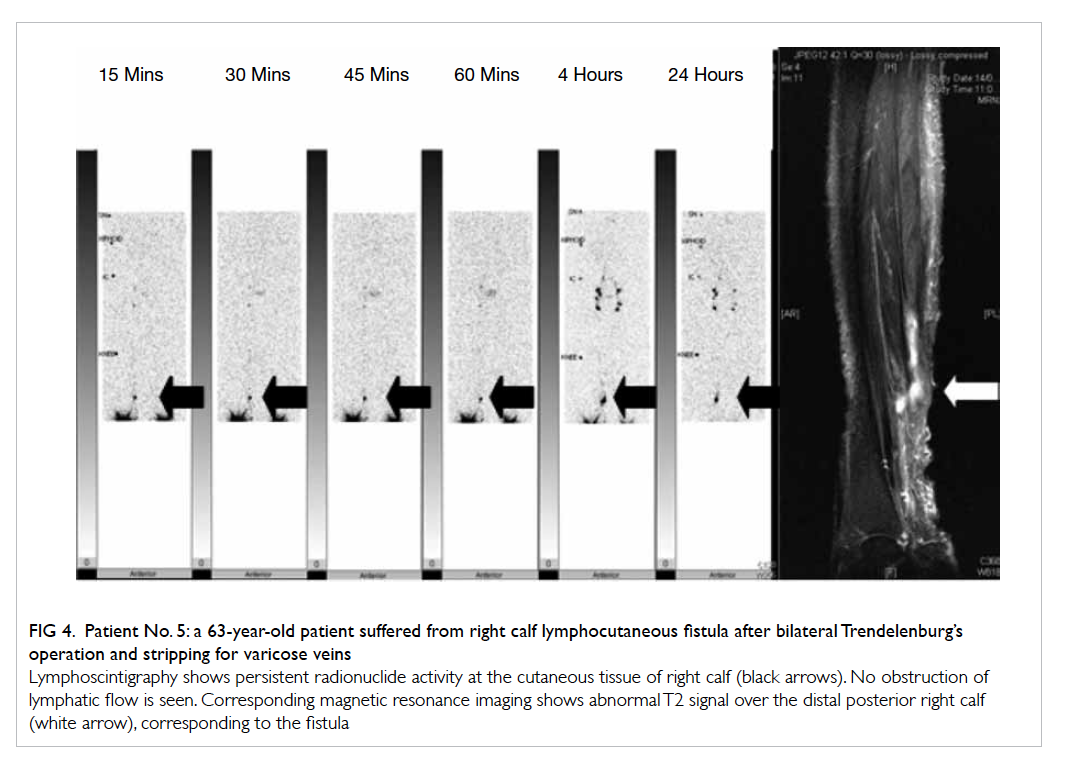
Figure 4. Patient No. 5: a 63-year-old patient suffered from right calf lymphocutaneous fistula after bilateral Trendelenburg’s operation and stripping for varicose veins
Discussion
Lymphedema of the extremities is typically a chronic
disease, which is often misdiagnosed and results in
significant functional impairment, and may give rise
to reduced coordination and mobility.3 Therefore,
prompt and accurate diagnosis of the condition is
important.
Decades ago, lymphangiography had been
used to investigate lymphatic disorders, but it
was a time-consuming investigation involving
direct cannulation of lymph vessels. Moreover, complications such as infections, hypersensitivity,
oil embolism, and lymphatic obstruction were
reported.4 Lymphoscintigraphy has replaced
lymphangiography and become the investigation of
choice. Its advantages include being non-invasive, free from adverse effects, and low radiation exposure
to patients. Furthermore, it can be repeated and
can even be used to follow-up after treatment
response.5 The reported sensitivity and specificity of
lymphoscintigraphy is approximately 66 to 100% and 83.5 to 99%, respectively.6
Lymphedema can usually be diagnosed
clinically. The differential diagnosis of suspected
lower-extremity lymphedema includes obesity,
chronic venous insufficiency, Milroy’s disease,7
and systemic diseases (eg hypoalbuminaemia).
Lymphoscintigraphy enables confirmation of the
diagnosis in unclear cases, assessing the risk of
developing lymphedema,8 predicting the outcome of
therapy,9 and assessing the results of lymphedema
treatment.10 11 12 13
Lymphoscintigraphy can usually identify
the approximate anatomical site of lymphatic
obstruction adequately. However, when greater
anatomical details are warranted, cross-sectional
imaging techniques like computed tomography
and magnetic resonance imaging can be used to
supplement the findings.14 This point was well
illustrated in this study.
Lymphoscintigraphy aids the diagnosis of
underlying lymphatic disorders and hence, guides
subsequent treatment, which have proven to be
effective in the management of lymphedema.15 16 17 18 19
Conservative treatment includes physical therapy,
drug therapy, and psychosocial rehabilitation.14
Operative treatment includes microsurgery,
liposuction, and surgical resection.14 The treatment
choice depends on the cause of lymphedema, disease
severity, functional impairment, and availability of
local expertise.
Conclusion
Lymphoscintigraphy is a safe and effective
investigation for suspected lymphatic disorders. Our
local experience supports its use in the investigation
of lower-extremity lymphedema in our locality.
References
1. Ter SE, Alavi A, Kim CK, Merli G. Lymphoscintigraphy. A reliable test for the diagnosis of lymphedema. Clin Nucl Med 1993;18:646-54. CrossRef
2. Rockson SG, Rivera KK. Estimating the population burden of lymphedema. Ann N Y Acad Sci 2008;1131:147-54. CrossRef
3. Szuba A, Shin WS, Strauss HW, Rockson S. The third circulation: radionuclide lymphoscintigraphy in the evaluation of lymphedema. J Nucl Med 2003;44:43-57.
4. Van Rensburgl. Lymphangiography—its technique and value. S Afr Med J 1965;39:271-7.
5. Williams WH, Witte CL, Witte MH, McNeill GC. Radionuclide lymphangioscintigraphy in the evaluation of peripheral lymphedema. Clin Nucl Med 2000;25:451-64. CrossRef
6. Bourgeois P. Critical analysis of the literature on lymphoscintigraphic investigations of limb edemas. Eur J Lymphology Relat Probl 1996;6:1-9.
7. James WD, Berger TG, Elston DM, Odom RB, editors. Andrews' diseases of the skin: clinical dermatology. Philadelphia: Saunders Elsevier; 2006: 849.
8. Bourgeois P, Leduc O, Leduc A. Imaging in the management and prevention of posttherapeutic upper limb edema. Cancer 1998;83(12 Suppl American):2805-13.
9. Szuba A, Strauss W, Sirsikar SP, Rockson SG. Quantitative radionuclide lymphoscintigraphy predicts outcome of manual lymphatic therapy in breast cancer–related lymphedema of the upper extremity. Nucl Med Commun 2002;23:1171-5. CrossRef
10. Campisi C. Lymphoedema: modern diagnostic and therapeutic aspects. Int Angiol 1999;18:14-24.
11. Ho LC, Lai MF, Yeates M, Fernandez V. Microlymphatic bypass in obstructive lymphedema. Br J Plast Surg 1988;41:475-84. CrossRef
12. Brorson H, Svensson H, Norrgren K, Thorsson O. Liposuction reduces arm lymphedema without significantly altering the already impaired lymph transport. Lymphology 1998;31:156-72.
13. Hwang JH, Kwon JY, Lee KW, et al. Changes in lymphatic function after complex physical therapy for lymphedema. Lymphology 1999;32:15-21.
14. International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema. 2009 Consensus Document of the International Society of Lymphology. Lymphology 2009;42:51-60.
15. McNeely ML, Peddle CJ, Yurick JL, Dayes IS, Mackey JR. Conservative and dietary interventions for cancer-related lymphedema: a systematic review and meta-analysis. Cancer 2011;117:1136-48. CrossRef
16. Badger CM, Peacock JL, Mortimer PS. A randomized, controlled, parallel-group clinical trial comparing multilayer bandaging followed by hosiery versus hosiery alone in the treatment of patients with lymphedema of the limb. Cancer 2000;88:2832-7. CrossRef
17. Miller TA, Wyatt LE, Rudkin GH. Staged skin and subcutaneous excision for lymphedema: a favorable report of long-term results. Plast Reconstr Surg 1998;102:1486-98; discussion 1499-501. CrossRef
18. Yamamoto Y, Sugihara T. Microsurgical lymphaticovenous implantation for treatment of chronic lymphedema. Plast Reconstr Surg 1998;101:157-61. CrossRef
19. Matarasso A, Hutchinson OH. Liposuction. JAMA 2001;285:266-8. CrossRef