Hong Kong Med J 2014;20:113–20 | Number 2, April 2014 | Epub 21 Oct 2013
DOI: 10.12809/hkmj134023
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Uterine compression sutures for management of
severe postpartum haemorrhage: five-year audit
Victoria YK Chai, MB, BS, MRCOG; William
WK To, MD, FRCOG
Department of Obstetrics and Gynaecology,
United Christian Hospital,
Kwun Tong, Hong Kong
Corresponding author: Dr WWK To (towkw@ha.org.hk)
Abstract
Objectives: To audit
the use of compression
sutures for the management of massive postpartum
haemorrhage and compare outcomes to those
documented in the literature.
Design: Retrospective
study.
Setting: A regional
obstetric unit in Hong Kong.
Patients: Patients with
severe postpartum
haemorrhage encountered over a 5-year period
from January 2008 to December 2012, in which
compression sutures were used for management.
Main outcome measures: Successful
management
with prevention of hysterectomy.
Results: In all, 35
patients with massive postpartum
haemorrhage with failed medical treatment, for
whom compression sutures were used in the
management, were identified. The overall success
rate for the use of B-Lynch compression sutures alone
to prevent hysterectomy was 23/35 (66%), and the
success rate of compression sutures in conjunction with other
surgical procedures was 26/35 (74%).
This reported success rate appeared lower than that
reported in the literature.
Conclusion: Uterine
compression was an effective
method for the management of massive postpartum
haemorrhage in approximately 70% of cases,
and could be used in conjunction with other
interventions to increase its success rate in terms of
avoiding hysterectomy.
New knowledge added by this
study
- Compression sutures are effective in the management of postpartum haemorrhage arising from uterine atony as well as placenta praevia.
- In an unselected case series audit in a regional obstetric training unit, the efficacy of uterine compression sutures appeared to be lower than that reported in the literature.
- Uterine compression sutures should be adopted as part of the management of severe postpartum haemorrhage in local obstetric units. Contingent treatment protocols for further interventions should be available if compression sutures fail.
Introduction
Postpartum haemorrhage (PPH) is a serious
and
life-threatening obstetric complication. It is usually
defined as an estimated blood loss of more than
500 mL after delivery and occurs in around 5% of
all deliveries.1 As
increased maternal morbidity
and morbidity are associated with further blood
loss, alternative definitions for severe PPH,
such as estimated blood loss exceeding 1000
mL, are commonly used in various guidelines.2
Conventionally, the first-line treatment options
for PPH include conservative management with
uterotonic drugs (oxytocin or prostaglandins),
while second-line therapy includes uterine packing,
external compression with uterine sutures, selective
devascularisation by ligation, or embolisation of the uterine
artery.3 4 5 6 7 These
various treatment
modalities have been included as an integral part of
the HEMOSTASIS management algorithm widely
advocated in the UK.8 The
use of such measures
should reduce the need for hysterectomy, which is
associated with further blood loss and additional
morbidity.9
The B-Lynch suture has been the most
wellestablished
compression suture technique since
reporting of the first published series in 1997, and
described oversewing of the uterus with a continuous
suture to apply ongoing compression.4
Since then,
the technique has been adopted for control of
bleeding in severe PPH due to uterine atony as well
as placenta praevia/accreta.10
11 Modifications of the
original technique, as well as various other suturing techniques,
have since been advocated.5
12 13 14
The
current case series described the use of compression
sutures in the management of massive PPH that
failed to respond to medical therapy over a review
period of 60 months encountered in a single obstetric
training and service unit of the Hong Kong Hospital
Authority. The compression suture techniques
employed in this series were the basic B-Lynch
or the slightly modified Bhal technique.15
Various
associated prognostic factors were assessed and
compared to evaluate whether they could predict
success or failure.
Methods
A retrospective review of all patients
having a
severe PPH over a 60-month period (January 2008
to December 2012 inclusive) was performed, based
on details logged in a comprehensive obstetric
database currently used in all Hospital Authority
obstetric units. Specific codings for “primary PPH”,
“compression sutures of uterus”, “caesarean section
with hysterectomy”, and “peripartum hysterectomy”
were searched for and identified from the clinical
management system of the hospital. Cases of
severe PPH with blood loss exceeding 1 L were also
identified from the Labour Ward registry. The case
notes or operative records of each of these patients
were also reviewed to verify whether management
entailed use of compression suturing techniques.
All identified cases where compression sutures had
been used or their use attempted were then reviewed in detail for
the mode of delivery, intrapartum
complications, cause of the PPH, sequence of
treatment modalities used, estimated total blood
loss, any complications resulting from the different
manoeuvres, and clinical outcome.
The application of the B-Lynch suture was
in accordance with the original description with
the hysterectomy wound still open, using either
Monocryl or Vicryl No.1 sutures in accordance
with the surgeon’s preference. In some cases,
two separate sutures were applied instead of one
continuous suture as described by Bhal et al.15 All
patients had an indwelling Foley catheter to monitor
urine output, and broad-spectrum antibiotics were
used for prophylaxis. All patients who had severe
haemorrhage treated by intra-operative transfusions
and all who had evidence of coagulopathy were
admitted to the intensive care unit after their
operation.
Results
There were a total of 26 029 deliveries
over the review
period. The point prevalence of primary PPH with
estimated blood loss exceeding 500 mL was 3.2%
(n=825), and that exceeding 1 L (severe PPH) was
105/26 029 (0.4%). Among the latter, 33 had vaginal
delivery and 72 caesarean sections; 25 of these
patients were managed by medical treatment alone.
Regarding the remaining 80 patients with severe
PPH, their management is shown in the Figure.
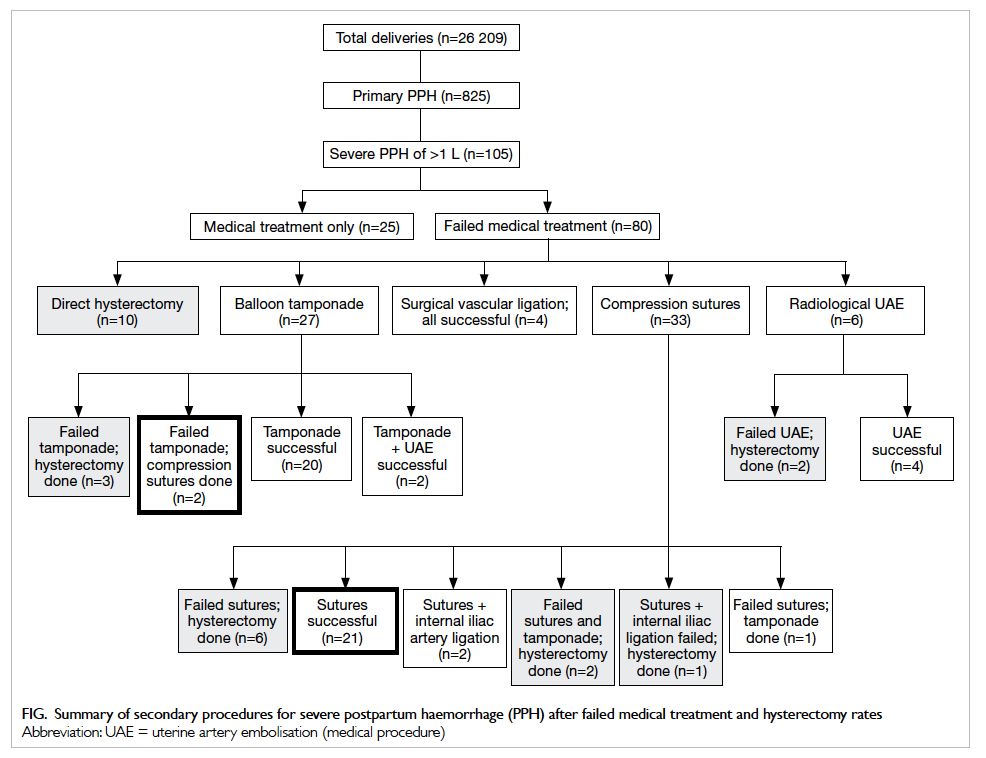
Figure. Summary of secondary procedures for severe postpartum haemorrhage (PPH) after failed medical treatment and hysterectomy rates
Within this study period, there were 24
peripartum hysterectomies, of which nine involved
attempted use of compression sutures and were
included in this case series. The other 15 cases
included the 10 who had an a priori hysterectomy (6
for placenta praevia/accreta, 4 for intractable uterine
atony) without resort to other more conservative
procedures, two for uterine atony with failed
treatment following radiological uterine arterial
embolisation, and three who had hysterectomy when
attempted intrauterine balloon tamponade failed
to control the bleeding. Cases that did not entail
recourse to uterine compression sutures were not
analysed any further.
All the identified cases of PPH that
involved
the use of compression sutures had failed initial
medical management with oxytoxics, including
bolus syntometrine, syntocinon bolus or infusion,
intramuscular carboprost injections, and in nine
cases, additional intramyometrial carboprost
injections. The most common aetiology of PPH
was uterine atony (28/35), followed by major
placenta praevia (7/35), and the total estimated
intra-operative blood losses of 1000 to 9300 mL.
Approximately 80% (28/35) of the patients were
deemed to require intra-operative blood product
transfusion, and disseminated intravascular
coagulopathy was documented in at least 13 (37%) of them. In one
patient (No. 3), attempted Bhal sutures
failed to arrest the bleeding from uterine atony, and
subtotal hysterectomy was performed. She had a
stump haematoma and massive stump bleeding 3
days later, for which the cervical stump was removed.
The bladder was perforated and despite immediate
repair at operation, she subsequently developed a
vesico-vaginal fistula that was surgically repaired 2
months after the hysterectomy. This was the only
patient in our series with major organ trauma. There
was no maternal mortality (Table: left, right).
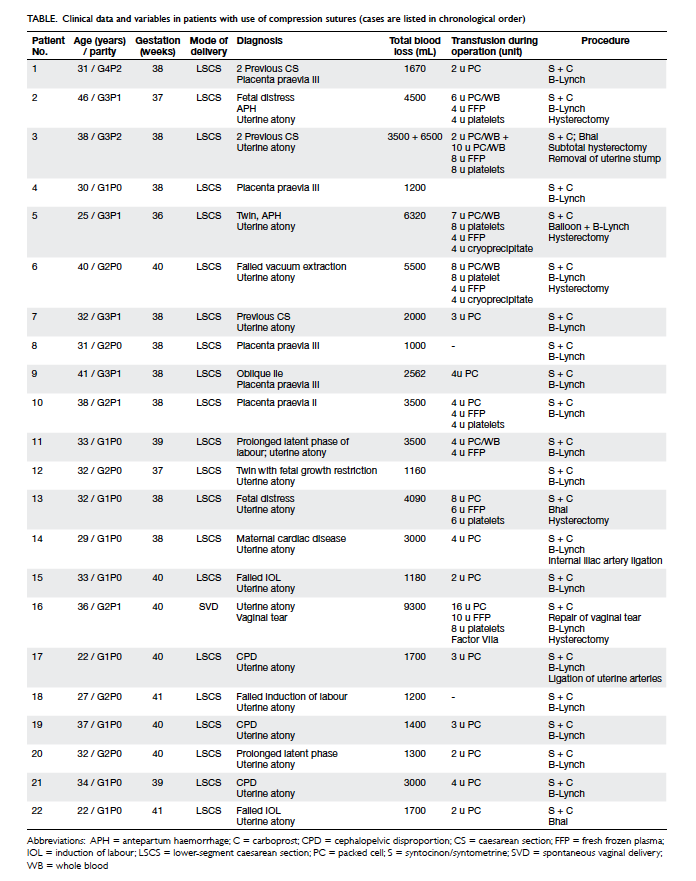
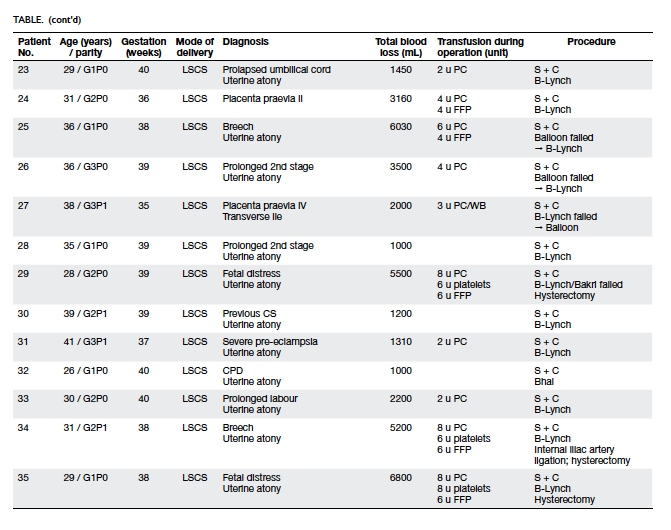
Table. Clinical data and variables in patients with use of compression sutures (cases are listed in chronological order)
One patient (No. 16) had a normal vaginal
delivery followed by massive PPH despite oxytoxics.
Examination under anaesthesia was performed, and
vaginal tears were repaired. Laparotomy and B-Lynch
sutures were applied because of concurrent uterine
atony, but hysterectomy was finally performed. This
patient had the highest estimated blood loss (9.3 L)
in our case series and was the only one given Factor
VIIa for coagulopathy management.
Compression sutures were attempted together
with intrauterine balloon tamponade in five cases. In one patient
(No. 5) with uterine atony after caesarean
section for twin pregnancy, abdominal placement
of a Bakri balloon (for tamponade) was attempted
but failed to arrest the bleeding. The balloon was
removed and compression sutures were applied but
to no avail, and so a hysterectomy was performed.
In another patient with uterine atony following
caesarean section for fetal distress (No. 29), when
balloon tamponade failed to arrest bleeding, an
attempt to add on B-Lynch sutures in the form of a
“sandwich”16 led to
puncturing of the balloon, and so
a hysterectomy was performed. In two others with
uterine atony after caesarean section, abdominal
placement of a Bakri balloon failed to control
bleeding, but a B-Lynch suture was effective (Nos.
25 and 26). In a third patient (No. 27) with major
placenta praevia, B-Lynch sutures failed to arrest
haemorrhage. The sutures were therefore removed
and a Bakri balloon inserted via the hysterotomy
wound, and successfully controlled bleeding into the
lower uterine placental bed.
In two patients with uterine atony after
caesarean section (Nos. 14 and 17), continuous
bleeding from the vagina was observed after
application of B-Lynch sutures, and thus ligation
of the internal iliac arteries/uterine arteries was
performed with effective outcome. In a third
patient (No. 34), internal iliac artery ligation failed
to control the haemorrhage, and so a hysterectomy
was performed. Four other patients (Nos. 2, 6, 13,
and 35) failed to have their bleeding controlled by
compression sutures and underwent hysterectomies.
Thus, in our series the overall success
rate of
compression sutures alone as the primary second-line
(n=21) or rescue procedure (n=2) to prevent
hysterectomy was 23/35 (66%). The success rate
of compression sutures in conjunction with other
second-line procedures (two with iliac artery ligation
and one with intrauterine balloon tamponade) was
26/35 (74%). Specifically, when the aetiology of the
PPH was taken into consideration, the success rate
for B-Lynch compression sutures in patients with
uterine atony was 17/28 (61%) and that for placenta praevia cases
it was 6/7 (86%). The Bhal suture was
used in four cases only (Nos. 3, 13, 22, and 32) and its
success rate of 50% was not statistically significantly
different from that of B-Lynch sutures.
Particular putative patient risk factors
that
could reliably predict the success of compression
sutures as a means of avoiding hysterectomy included
age, parity, mode of delivery, operator experience,
aetiology of the PPH, and the extent of blood loss
at that time. Based on a multivariate stepwise
regression analysis, no significant risk factors for the
success of compression sutures could be identified in
the current data set.
Discussion
In this series, we were able to avoid
hysterectomy with
the use of uterine compression sutures, either alone
or in combination with other surgical interventions,
in only around 70% of patients with severe PPH. This
success rate was lower than that reported in many
other reported case series.4
5 11 12 13 14 17 18 19 20 21
The first description of uterine compression
sutures was published in 1996 as a single case
report from Zurich,22 which was followed by the
famous report of five consecutive cases utilising the
B-Lynch suture in 1997.4 Various modifications of
the B-Lynch suture, and various other compression
suture techniques have been reported since then.
In 2000, Cho et al13 described a haemostatic
multiple square suture to approximate the anterior
and posterior uterine wall. In 2002, Hayman et al5
proposed a uterine compression suture that involved
two vertical apposition sutures together with two
transverse horizontal cervico-isthmic sutures. In
2005, Hwu et al14 described the use of two parallel
vertical compression sutures placed in the lower
segment to control bleeding from placenta praevia.
These sutures compressed the anterior and posterior
uterine wall without penetrating the full thickness
of the posterior wall. Another modification was the
Pereira suture reported in 2005, which consisted
of longitudinal and transverse sutures applied with
superficial intramyometrial bites only.17 In the current
case series, the only modification to the B-Lynch
suture utilised was the Bhal technique.15 This entailed
two sutures instead of one, with the knots tied in
the anterior-inferior margin of the lower uterine
segment, without any difference in the compression
effects compared to the original B-Lynch suture. It
can be seen that the principle, namely, compression
of the uterine body, remains basically the same for all
types of compression sutures. The main differences
being the figure at which the suture is applied, the
numbers of longitudinal and/or transverse sutures
used, and whether or not the uterine cavity is
penetrated.23
In the literature, some series have described
compression sutures solely used for placenta
praevia/accreta,11 14 18 24 while others detailed their
use exclusively for atonic uteruses,19 20 and still
others referred to application of the technique to all
aetiologies.4 21 Apart from compressing the uterine
body in uterine atony, the original paper on the
B-Lynch suture also advocated its use for placenta
praevia. It was proposed that the sutures would
exert longitudinal compression and achieve evenly
distributed tension over the uterus, including the
lower segment.25 In addition, for cases of major
placenta praevia, B-Lynch also described the use
of additional independent figure-of-eight sutures
placed either anteriorly, posteriorly, or both on the
lower segment prior to suture application.4 Our
results from this series confirm the effectiveness of
the B-Lynch suture for patients with uterine atony
and placenta praevia.
Very high success rates with compression
sutures, usually in the range of 90﹪ to 100%, have
been reported since the first paper by B-Lynch in
1997.4 However, many of these reports had very small sample sizes (single case reports or cohorts of
15-20 patients).13 26 In recent years, larger case series
started to be reported. One of the largest published
series described experience from India, and reported
a success rate of 94% (45 out of 48 patients) using
Hayman sutures for PPH due to uterine atony.19 That
series did not include cases with placenta praevia/
accreta.19 Another interesting case series consisted
of a single surgeon’s experience in Argentina over a
20-year period, and involved 539 cases of excessive
obstetric bleeding from a variety of causes, including
uterine atony, placenta praevia/accreta, cervical scar
pregnancies as well as uterine/vaginal/cervical tears.21
Various surgical methods (often in combination) were
utilised to treat these cases, and the overall success rate
in those having the B-Lynch suture was 94% (81/86),
while for Hayman sutures, Cho sutures, and Pereira
sutures, the rates were 92% (34/37), 100% (37/37), and
100% (11/11), respectively.21 The very high success
rates reported in this personal series could be ascribed
to excellent surgical skills, optimal patient selection,
and choice of procedures by a super-specialist, but
may be difficult to reproduce elsewhere.
An earlier systematic review published in 2007
reported a success rate for uterine compression
sutures ranging from 68﹪ to 100% with an overall
success rate of 92%.6 Another review in 2010 compared
success rates of 95﹪ to 100% with eight different types
of compression sutures.27 However, both reviews
were based on case series with relatively small patient
numbers, which might indicate a reporting bias and
probably exaggerated the proportions with positive
outcomes. Interestingly, another review published in
2010 that focused on the long-term complications of
compression sutures and attempted to sum outcomes
with B-Lynch sutures from 32 separate case series.23
This reported an overall hysterectomy (failure) rate of
70/174 (40%), which was higher than most individual
case series.23
In this series, the mode of delivery was vaginal
in only one case (3%), the rest being delivered by
caesarean section (97%). This was likely due to a
bias in case selection in our practice. In patients
with severe PPH not delivered by caesarean section,
compression sutures were probably not the first-choice
surgical treatment due to consideration for
laparotomy and opening a hysterotomy wound.
Apparently, methods such as balloon tamponade28
were more common and convenient. The original
intrauterine Bakri balloon was designed to control
bleeding in patients with PPH caused by low-lying
placenta praevia/accreta.29 It could be inserted
easily and rapidly, without the need for laparotomy,
and under minimal anaesthesia. It can also be used
as a ‘tamponade test’ to aid decisions regarding
proceeding to laparotomy.3 Of the 27 cases of severe
PPH with balloon tamponade as the first- or second-line
procedure within our review period (Fig), 10 (37%) had vaginal delivery. Our experience with
the use of balloon tamponade has recently been
published in another case series.30
We were unable to identify any reliable
factors that would predict the success or failure of
compression sutures in this case series, possibly due
to the small size of our sample. Nor could we offer any
coherent hypothesis to explain our lower success rate
compared with that reported in the literature. As an
obstetric specialist is available on-site in our hospital
24 hours a day, specialist involvement was initiated
promptly in the management of all our cases. The 35
compression suture procedures were performed by
a total of eight surgeons with very similar training
and experiences in compression suture techniques.
They all used a relatively standard technique with
standard suture materials, and with standard
anaesthetic and transfusion support in accordance
with our hospital protocol. As compression sutures
placed for prophylactic purposes were not included
in this cohort, and all sutures were applied only in
the presence of severe PPH, the unselected nature
of our cases could have contributed to the lower
success rate. We believe that a success rate of around
70% would likely reflect the practical experience in a
general regional obstetric training unit locally.
Major complications of B-Lynch and other
compression sutures have been repeatedly described
in the literature. Cases of uterine necrosis presenting
several weeks post-delivery finally culminating
in total or subtotal hysterectomy have been
reported.31 32 Uterine necrosis was apparently the
result of ischaemia produced by compression sutures.
Haematometra might present with amenorrhoea33
and pyometria coupled with abdominal pain and
fever, weeks or months postpartum.34 The occurrence
of uterine cavity synechiae causing uterine outflow
obstruction has also been reported after compression
sutures, though infrequently.35 The combination of
compression sutures and additional vessel ligation
appeared more likely to cause complications such
as ischaemia and inflammation, but so far no deaths
have been reported in association with compression
sutures.23
Apart from compression suture and balloon
tamponade techniques, various fertility-preserving
methods had been employed for patients with PPH,
including pelvic devascularisation and radiological
arterial embolisation. Pelvic devascularisation
includes ligation of uterine artery and internal
iliac artery, but such techniques require surgical
expertise to apply and may be time-consuming.
Complications such as broad-ligament haematoma,
peripheral nerve ischaemia, and inadvertent ligation
of the lower limb arteries have been reported.36 37
Radiological embolisation of the uterine artery
warrants facilities and expertise in interventional
radiology, which may not be readily available in some obstetric units. In addition, in cases of
massive ongoing PPH, it may be difficult to transfer
patients to such radiological facilities. Infrequently,
complications such as ischaemia of the bladder and
uterus have also been reported.38 A systematic review
estimated a success (avoidance of hysterectomy) rate
of around 92% with uterine compression sutures,
91% after arterial embolisation, 84% after balloon
tamponade, and 85% after iliac artery ligation or
uterine devascularisation.6 Randomised controlled
trials of these treatment options would be difficult
to perform in such life-threatening emergencies.
To date, there is no good evidence to suggest that
one method is superior to another. As illustrated
in several of the cases in our series, the sequential
or concomitant use of these different interventions
may help to increase the success rate. The patient’s
condition, cause of the PPH, expertise of the surgeon,
and facilities available should all be considered when
choosing the most suitable treatment option.
Conclusion
In our experience, the use of compression sutures
for the management of massive PPH was effective
in preventing hysterectomy in around two thirds of
the cases. In this unselected cohort of patients with
severe PPH, our success rate appeared to be lower
than that reported in the literature. Other contingent
protocols should be available, should compression
sutures fail to control the haemorrhage. The
combined or sequential use of compression sutures
with other treatment modalities, such as balloon
tamponade, pelvic devascularisation or radiological
embolisation, may help to increase the success rate,
and should be explored further.
References
1. American College of
Obstetricians and Gynecologists. ACOG Practice Bulletin. Clinical
Management Guidelines for Obstetricians-Gynecologists. Number 76,
October 2006: postpartum hemorrhage. Obstet Gynecol
2006;108:1039-47.
2. Chandraharan E, Arulkumaran S.
Surgical aspects of postpartum haemorrhage. Best Pract Res Clin
Obstet Gynaecol 2008;22:1089-102. CrossRef
3. Condous GS, Arulkumaran S.
Medical and conservative surgical management of postpartum
hemorrhage. J Obstet Gynaecol Can 2003;25:931-6.
4. B-Lynch C, Coker A, Lawal AH,
Abu J, Cowen MJ. The B-Lynch surgical technique for the control of
massive postpartum haemorrhage: an alternative to hysterectomy?
Five cases reported. Br J Obstet Gynaecol 1997;104:372-5. CrossRef
5. Hayman RG, Arulkumaran S, Steer
PJ. Uterine compression sutures: surgical management of postpartum
hemorrhage. Obstet Gynecol 2002;99:502-6. CrossRef
6. Doumouchtsis SK, Papageorghiou
AT, Arulkumaran S. Systematic review of conservative management of
postpartum hemorrhage: what to do when medical treatment fails.
Obstet Gynecol Surv 2007;62:540-7. CrossRef
7. Royal College of Obstetricians
and Gynaecologists. RCOG Green-top guideline No 52. Prevention and
management of postpartum haemorrhage; May 2009.
8. Varatharajan L, Chandraharan E,
Sutton J, Lowe V, Arulkumaran S. Outcome of management of massive
postpartum haemorrhage using the algorithm "HEMOSTASIS". Int J
Gynecol Obstet 2011;113:152-4. CrossRef
9. Knight M; UKOSS. Peripartum
hysterectomy in the UK: management and outcomes of the associated
haemorrhage. BJOG 2007;114:1380-7. CrossRef
10. Allam MS, B-Lynch C. The
B-Lynch and other uterine compression suture techniques. Int J
Gynaecol Obstet 2005;89:236-41. CrossRef
11. Arduini M, Epicoco G, Clerici
G, Bottaccioli E, Arena S, Affronti G. B-Lynch suture,
intrauterine balloon, and endouterine hemostatic suture for the
management of postpartum hemorrhage due to placenta previa
accreta. Int J Gynaecol Obstet 2010;108:191-3. CrossRef
12. Ghezzi F, Cromi A, Uccella S,
Raio L, Bolis P, Surbek D. The Hayman technique: a simple method
to treat postpartum haemorrhage. BJOG 2007;114:362-5. CrossRef
13. Cho JH, Jun HS, Lee CN.
Hemostatic suturing technique for uterine bleeding during cesarean
delivery. Obstet Gynecol 2000;96:129-31. CrossRef
14. Hwu YM, Chen CP, Chen HS, Su
TH. Parallel vertical compression sutures: a technique to control
bleeding from placenta praevia or accreta during caesarean
section. BJOG 2005;112:1420-3. CrossRef
15. Bhal K, Bhal N. Mulik V,
Shankar L. The uterine compression suture—a valuable approach to
control major haemorrhage at lower segment caesarean section. J
Obstet Gynaecol 2005;25:10-4. CrossRef
16. Nelson WL, O'Brien JM. The
uterine sandwich for persistent uterine atony: combining the
B-Lynch compression suture and an intrauterine Bakri balloon. Am J
Obstet Gynecol 2007;196:e9-10. CrossRef
17. Pereira A, Nunes F, Pedroso S,
Saraiva J, Retto H, Meirinho M. Compressive uterine sutures to
treat postpartum bleeding secondary to uterine atony. Obstet
Gynecol 2005;106:569-72. CrossRef
18. Shazly SA, Badee AY, Ali MK.
The use of multiple 8 compression suturing as a novel procedure to
preserve fertility in patients with placenta accreta: case series.
Aust NZ J Obstet Gynaecol 2012;52:395-9. CrossRef
19. Nanda S, Singhal SR. Hayman
uterine compression stitch for arresting atonic postpartum
hemorrhage: 5 years experience. Taiwan J Obstet Gynecol
2011;50:179-81. CrossRef
20. Zheng J, Xiong X, Ma Q, Zhang
X, Li M. A new uterine compression suture for postpartum
haemorrhage with atony. BJOG 2011;118:370-4. CrossRef
21. Palacios-Jaraquemada JM.
Efficacy of surgical techniques to control obstetric haemorrhage:
analysis of 539 cases. Acta Obstet Gynecol Scand 2011;90:1036-42. CrossRef
22. Schnarwyler B, Passweg D, von
Castelberg B. Successful treatment of drug refractory uterine
atony by fundal compression sutures [in German]. Geburtshilfe
Frauenheilkd 1996;56:151-3. CrossRef
23. Fotopoulou C, Dudenhausen JW.
Uterine compression sutures for preserving fertility in severe
postpartum haemorrhage: an overview 13 years after the first
description. J Obstet Gynaecol 2010;30:339-49. CrossRef
24. Makino S, Tanaka T, Yorifuji
T, Koshiishi T, Sugimura M, Takeda S. Double vertical compression
sutures: a novel conservative approach to managing post-partum
haemorrhage due to placenta praevia and atonic bleeding. Aust NZ J
Obstet Gynaecol 2012;52:290-2. CrossRef
25. B-Lynch C. Partial ischemic
necrosis of the uterus following a uterine brace compression
suture. BJOG 2005;112:126-7. CrossRef
26. Quahba J, Piketty M, Huel C,
et al. Uterine compression sutures for postpartum bleeding with
uterine atony. BJOG 2007;114:619-22. CrossRef
27. Mallappa Saroja CS, Nankani A,
El-Hamamy E. Uterine compression sutures, an update: review of
efficacy, safety and complications of B-Lynch suture and other
uterine compression techniques for postpartum haemorrhage. Arch
Gynecol Obstet 2010;281:581-8. CrossRef
28. Georgiou C. Balloon tamponade
in the management of postpartum haemorrhage: a review. BJOG
2009;116:748-57. CrossRef
29. Bakri YN, Amri A, Abdul Jabbar
F. Tamponade-balloon for obstetrical bleeding. Int J Gynaecol
Obstet 2001;74:139-42. CrossRef
30. Kong MC, To WW. Balloon
tamponade for postpartum haemorrhage: case series and literature
review. Hong Kong Med J 2013;19:484-90.
31. Treloar EJ, Anderson RS,
Andrews HS, Bailey JL. Uterine necrosis following B-Lynch suture
for primary postpartum haemorrhage. BJOG 2006;113:486-8. CrossRef
32. Joshi VM, Shrivastava M.
Partial ischemic necrosis of the uterus following a uterine brace
compression suture. BJOG 2004;111:279-80. CrossRef
33. Dadhwal V, Sumana G, Mittal S.
Hematometra following uterine compression sutures. Int J Gynaecol
Obstet 2007;99:255-6. CrossRef
34. Ochoa M, Allaire AD, Stitely
ML. Pyometria after hemostatic square suture technique. Obstet
Gynecol 2002;99:506-9. CrossRef
35. Wu HH, Yeh GP. Uterine cavity
synechiae after hemostatic square suturing technique. Obstet
Gynecol 2005;105:1176-8. CrossRef
36. O'Leary JA. Uterine artery
ligation in the control of postcesarean hemorrhage. J Reprod Med
1995;40:189-93.
37. Shin RK, Stecker MM, Imbesi
SG. Peripheral nerve ischaemia after internal iliac artery
ligation. J Neurol Neurosurg Psychiatry 2001;70:411-2. CrossRef
38. Porcu G, Roger V, Jacquier A,
et al. Uterus and bladder necrosis after uterine artery
embolisation for postpartum haemorrhage. BJOG 2005;112:122-3. CrossRef

