Hong Kong Med J 2014;20:32–6 | Number 1, February 2014 | Epub 9 Jan 2014
DOI: 10.12809/hkmj133952
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Occlusion therapy in amblyopia: an experience from Hong Kong
Emily WH Tang, FRCSEd1;
Brian CY Li, MB, ChB1;
Ian YL Yeung, MRCS (Ed), MRCOphth1,2;
Kenneth KW Li, FRCSEd1,2
1 Department of Ophthalmology, United Christian Hospital, Kwun Tong,
Hong Kong
2 Eye Institute, LKS Faculty of Medicine, The University of Hong Kong,
Pokfulam, Hong Kong
Corresponding author: Dr EWH Tang (etang@graduate.hku.hk)
Abstract
Objectives: To review the results of patching for
amblyopia management in Hong Kong.
Design: Retrospective case series.
Setting: Regional hospital, Hong Kong.
Patients: Records of all patients attending Paediatric
Ophthalmology Clinic at United Christian Hospital,
Hong Kong from 1 January 2009 to 31 March
2009 were retrospectively reviewed. Records of all
children who underwent patching for amblyopia in
the study period were evaluated.
Results: The mean age of 50 children (50 eyes)
was 4 (standard deviation, 1; range, 2-7) years and
mean pretreatment visual acuity was 0.35 (0.15;
0.02-0.63) [~20/60]. The values for mean, standard
deviation, and range of treatment duration were
27, 16, 4-67 months respectively, and corresponding values for
prescribed patching per day were 4, 1, 2-8 hours.
The mean, standard deviation, and range of visual
acuity at final post-treatment assessment were 0.66,
0.16, 0.1-1.0 (~20/30), respectively. The overall success rate (ie
final visual acuity >0.7 or 20/30) was 62%. Children
with moderate amblyopia (20/40-20/80) and severe
amblyopia (20/100-20/400) had success rates of
74% and 55%, respectively. The mean visual acuity
improvements for moderate and severely amblyopic
children were 2.3 lines and 5.8 lines, respectively.
The mean, standard deviation, and range of patching
prescriptions for moderate and severely amblyopic children were 5, 1, 2-7 hours and 5, 1, 3-6 hours,
respectively. Recurrence ensued in 7% of the children
with moderate amblyopia and 46% of those with
severe amblyopia. Reported compliance was good
(>75% of the time) in 68% of the children.
Conclusion: Occlusion therapy is the mainstay
of treatment in Hong Kong. The overall success
rate was comparable to that achieved in the
Amblyopia Treatment Study. Recurrence was more
common in patients with severe amblyopia, for
whom maintenance therapy may reduce the risk of
recurrence. The duration of treatment was much
longer in our locality than in western countries.
Reported compliance was suspicious possibly due
to traditional cultural contexts. It is important to
emphasise compliance to all parents.
New knowledge added by this
study
- The Amblyopia Treatment Study (ATS) result cannot be directly applied to Hong Kong children. Heavier dosage for moderate amblyopia and longer treatment for both moderate and severe amblyopia appear necessary for successful treatment of affected Hong Kong children.
- The current practice for occlusion therapy in Hong Kong should not be changed to ATS recommendations; maintenance therapy should be considered with a view to reducing recurrences in children with severe amblyopia (visual acuity 20/100 to 20/400).
Introduction
Amblyopia is the most common cause of monocular
visual impairment in both children and young adults.1 2
Since year 2002, the Pediatric Eye Disease Investigator
Group has undertaken various randomised controlled
trials, known as the Amblyopia Treatment Study
(ATS). The ATS has provided insights into how
amblyopia can be most effectively managed with
respect to aspects such as dose response, the required amount of prescribed occlusion, compliance with
treatment, use of atropine, and the upper age limit for treatment.3 4 5 6
Despite recent research on amblyopia treatment,
studies show that the uptake of ATS guidelines and
their results into clinical practice are sporadic and
incomplete in both the UK and the US.7 Apparently,
one third of paediatric ophthalmologists have made
no changes whatsoever to their practice. Other studies found that 55% of paediatric ophthalmologists
had decreased their prescribed patching regimens,
which was contrary to ATS recommendations.8 9
In Hong Kong, patching is still the mainstay of
treatment for unilateral amblyopia. Yet, the impact
of the ATS guidelines on clinical practice is also
inadequate. In our locality, prescriptions for patching
are usually based on the age of the child. The duration
and subsequent dosages are tapered or adjusted
according to the individual child’s response and visual
acuity (VA) improvement. Our study therefore aimed
to compare current amblyopia management and
results of patching at a government hospital in Hong
Kong against the guidelines and results reported in
the ATS.
Methods
This was a retrospective case series study, for which
approval was obtained from the local research
ethics committee. Records of all children attending
the Paediatric Ophthalmology Clinic at the United
Christian Hospital, Hong Kong from 1 January 2009
to 31 March 2009 were reviewed. All children who had received patching for amblyopia were identified.
Two patients with structural abnormalities due to
cataract and retinal pathologies, one with bilateral
amblyopia warranting alternating patching, and three
others with incomplete data or follow-up of less than
3 months were excluded. In all, 50 patients (50 eyes)
were therefore identified and relevant demographic
data were obtained.
Patching protocol
Visual acuity was measured using Sheridan Gardiner
test for patients aged under 4 years and Snellen charts
for those 4 years old or older. Optical correction was
provided for all patients before commencement of
patching. Refraction with or without cycloplegia was
performed for the optical correction, which followed
our departmental guidelines, at the discretion of the
attending optometrist. Children were deemed to
require cycloplegic refraction if they had unreliable
retinoscopy or autorefraction readings (the very
young, the uncooperative, or having pseudomyopia);
accommodative esotropia; extreme refractive errors
(especially myopia); anisometropia (>2 dioptres); or
suspected amblyopia with >3 lines of difference in
VA.
Prescription of patching was based on the
age of the child, and the number of hours per day
corresponded to the age. For instance, 3 hours per
day for a 3-year-old and 5 hours per day for a 5-year-old.
Patching duration was titrated according to the
patient’s response and improvement of VA. Patching
therapy was stopped when the best-corrected visual
acuity (BCVA) of the amblyopic eye caught up or
equalled that of the fellow eye, or when the patient
reached 8 years old. Maintenance therapy was given
to patients with severe pretreatment amblyopia after
successful patching therapy and those with recurrent
amblyopia. Such prescriptions were for 2 hours per
day for around 6 to 8 months. Patients were regularly
reviewed every 3 to 4 months to monitor treatment
response including VA, refractive errors, compliance,
recurrence, and occurrence of occlusion amblyopia.
Outcome and statistical analysis
Demographic and baseline characteristics of the 50
patients were collected and analysed. Data relating
to BCVA before and after patching, duration and
intensity of patching, and compliance (percentage
subjectively reported by parents) were collected and
analysed.
Snellen VA was converted to equivalent logMAR
vision for statistical analysis. Treatment success was
defined as a BCVA of 20/30 (0.7) or better. Improved
VA in both the moderate and severe amblyopia groups
were compared with the corresponding ATS 2B and
ATS 2A study groups, respectively. All statistical
analysis was performed using statistical software
(Statistical Package for the Social Sciences; Windows version 16.0; SPSS Inc, Chicago [IL], US). The paired
t test, independent t test and Mann-Whitney U test
were used as appropriate, and a P value of less than
0.05 was considered significant.
Results
The demographic data and treatment results of the
50 patients are shown in Table 1. There were 42
patients with moderate (20/40-20/80) and severe
amblyopia (20/100-20/400) as defined by the ATS.
The overall success rate (ie final VA >0.7 or 20/30)
was 62% (31/50); respective success rates in those
with moderate (20/40-20/80) and severe amblyopia
(20/100-20/400) were 74% (23/31) and 55% (6/11).
The mean VA improvement at 4 months for moderate
and severe amblyopia children was 1.0 lines and 6.0
lines, respectively. The mean final VA improvement
for the moderately and severely amblyopic children
was 2.3 and 5.8 lines, respectively. The respective
mean ± standard deviation of moderately and severely
amblyopic children for the following outcome
measures were: patching prescription, 5 ± 1 (range,
2-7) hours/day and 5 ± 1 (range, 3-6) hours/day; and
patching duration, 23 ± 13 (range, 6-57) months and
38 ± 15 (range, 19-66) months. Reported compliance
was good (>75% of the time) in 68% (n=34), fair
(50-75% of the time) in 22% (n=11), and poor (<50%
of the time) in 18% (n=5) of the children. Visual
outcomes in relation to patient compliance in patients
with moderate and severe amblyopia are shown in
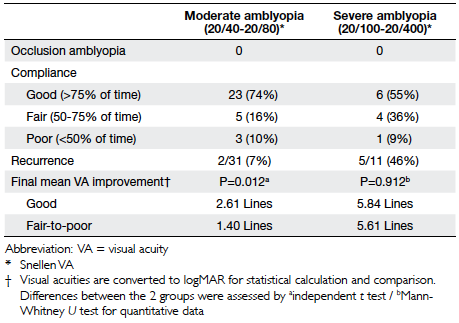
Table 2.
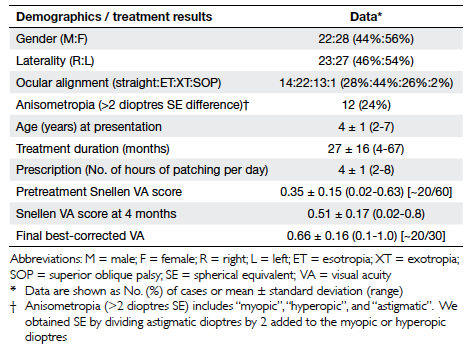
Table 1. Demographic data and treatment results of children with unilateral amblyopia attending Paediatric Ophthalmology Clinic in United Christian Hospital between January 2009 and March 2009
Subgroup comparisons
There were no significant differences in mean VA
improvement between children (i) aged <4 (n=16)
and ≥4 (n=34) years; (ii) having good (n=34) and fair-to-poor (n=16) compliance; and (iii) with straight
(n=14) and squint (n=36) eyes (Table 3).
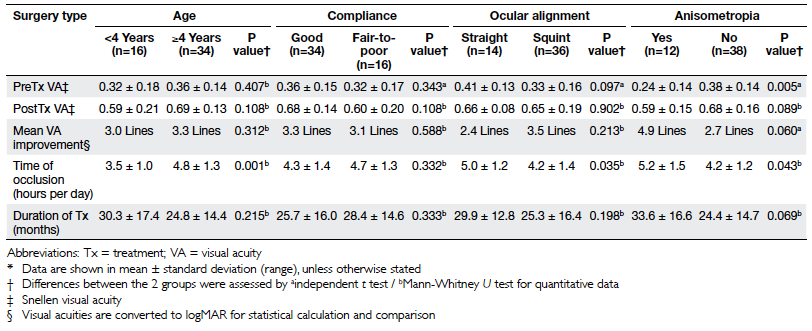
Table 3. Subgroup patient comparisons according to age, compliance, ocular alignment, and presence of anisometropia*
Regarding subgroup comparison for
anisometropia (n=12) and non-anisometropia (n=38)
groups, the former achieved significantly better mean
VA improvements (4.9 vs 2.7 lines, P=0.060). There
was no difference in the duration of treatment in the
two groups (Table 4).
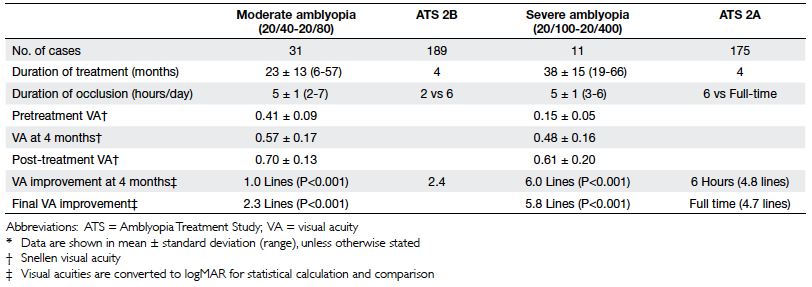
Table 4. Treatment duration and Snellen visual acuity outcomes with reference to the Amblyopia Treatment Study 2 (for children aged 3 to 7 years)*
Discussion
Amblyopia is a common condition in paediatric
ophthalmology, which is potentially reversible if
early treatment is given. It is an important condition
warranting efforts to maximise children’s visual
potential during their age of visual plasticity. In
our locality, the first-line treatment after refractive
correction is patching. Although ATS showed similar
results with patching as with atropine treatment,10 11
most parents in Hong Kong regard patching more
acceptable than atropine, because the latter usually
causes visual blurring and may affect the academic performance. This is an important consideration
for Hong Kong children who are often busy with
schoolwork, including ample near work. Adverse
reactions to atropine (flushing and fever) are also
common in this locality which also make this form of
treatment less popular.
Notably, the children in our series received
much longer durations of patching treatment
than those in ATS (27 vs 4 months), though the
final VA improvements were similar (Table 4).
In those with severe amblyopia, the mean VA
improvement at 4 months was slightly greater than
the final improvement. For severe amblyopia, 45% of the children (5/11) were assessed by the Sheridan
Gardiner test (suitable for children <4 years old) at
4 months instead of Snellen Acuity charts, though
the latter are considered more accurate. All 11
children were using Snellen Acuity charts during
the final VA assessment. Maintenance therapy might
have extended the treatment duration in certain
cases. Assuming Caucasian and Asian eyes as well
as environmental visual stimuli were similar, poor
compliance could be why longer patching therapy
was used to achieve similar VA improvements,
even after exclusion of structural abnormalities and
correction of refractive errors. In fact, the reported
compliance for occlusion therapy has been found to
be poor in other studies.12 13 The reported compliance
in our case series (68%) was good but suspicious.
Due to cultural reason, over-reporting of good
compliance was possible in our society. Traditionally,
the Chinese regard modest lies more positively than immodest truths.14 Hence, some parents may have
overstated the hours of occlusion. A similar situation
prevails when we deal with the compliance to anti-glaucomatous
eyedrops, in which the reasons for
medication non-adherence are complex and may
be societal rather than only medical.15 16 Objective
measurement of patching compliance and risk
factors analysis might be preferable for future studies.
Emphasis on compliance to patching is important to
communicate when commencing treatment and at
every subsequent follow-up visit.
Notably, recurrence was much more common
in patients with severe amblyopia (46%) than in those
in whom it was moderate (7%). This was consistent
with the ATS 2C results.6 Tapering of patching to
maintain therapy instead of abrupt termination may
help to reduce the risk of recurrence.
There was a concern about overtreatment, as
our dosages were much higher than those in ATS 2B (5 hours/day vs 2 hours/day) for moderate amblyopia.
Yet, no occlusion amblyopia was observed in our case
series. We believe vigilant and close monitoring of
the VA can avoid overtreatment.
Since this was a retrospective study, our case
series had several limitations, which included small
sample size, non-standardised treatment protocol,
heterogeneity of case mix, and lack of a control arm.
Nonetheless, this study supports the effectiveness
of the current Hong Kong practice for amblyopia
treatment by patching.
Conclusion
Our study showed treatment success rates comparable
to those of ATS for moderate amblyopia (74% vs 79%
in ATS 2B) and in all children (62% vs 62% in ATS
1). However, larger dosages for moderate amblyopia
and longer treatments for both moderate and
severe amblyopia appeared necessary for successful
treatment in Hong Kong children. Early treatment is
important. Maintenance therapy may help to reduce
recurrences in children with severe amblyopia. It
seems that ATS result cannot be directly applied to
Hong Kong children. It is important to emphasise
compliance to all parents.
References
1. Matta NS, Singman EL, Silbert DI. Evidenced-based
medicine: treatment for amblyopia. Am Orthopt J
2010;60:17-22. Crossref
2. Cools G, Houtman AC, Spileers W, Van Kerschaver E,
Casteels I. Literature review on preschool vision screening.
Bull Soc Belge Ophtalmol 2009;(313):49-63.
3. Pediatric Eye Disease Investigator Group. A randomized
trial of atropine vs patching for treatment of moderate
amblyopia in children. Arch Ophthalmol 2002;120:268-78. Crossref
4. Holmes JM, Kraker RT, Beck RW, et al. A randomized trial
of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology 2003;110:2075-87. Crossref
5. Repka MX, Beck RW, Holmes JM, et al. A randomized trial
of patching regimens for treatment of moderate amblyopia
in children. Arch Ophthalmol 2003;121:603-11. Crossref
6. Holmes JM, Beck RW, Kraker RT, et al. Risk of amblyopia
recurrence after cessation of treatment. J AAPOS
2004;8:420-8. Crossref
7. Newsham D. The effect of recent amblyopia research on
current practice in the UK. Br J Ophthalmol 2010;94:1352-7. Crossref
8. Wygnanski-Jaffe T. The effect on pediatric ophthalmologists
of the randomized trial of patching regimens for treatment
of moderate amblyopia. J AAPOS 2005;9:208-11. Crossref
9. Wygnanski-Jaffe T, Levin AV. The effect of the randomized
trial of patching regimens for treatment of moderate
amblyopia on pediatric ophthalmologists: 3-year outcome.
J AAPOS 2007;11:469-72. Crossref
10. Holmes JM, Beck RW, Kraker RT, et al. Impact of
patching and atropine treatment on the child and family
in the amblyopia treatment study. Arch Ophthalmol
2003;121:1625-32. Crossref
11. Felius J, Chandler DL, Holmes JM, et al. Evaluating the
burden of amblyopia treatment from the parent and child’s
perspective. J AAPOS 2010;14:389-95. Crossref
12. Stewart CE, Moseley MJ, Stephens DA, Fielder AR. Treatment
dose-response in amblyopia therapy: the monitored
occlusion treatment of amblyopia study (MOTAS). Invest
Ophthalmol Vis Sci 2004;45:3048-54. Crossref
13. Newsham D. Parental non-concordance with occlusion
therapy. Br J Ophthalmol 2000;84:957-62. Crossref
14. Fu G, Brunet MK, Lv Y, et al. Chinese children’s moral
evaluation of lies and truths—roles of context and parental
individualism-collectivism tendencies. Infant Child Dev
2010;19:498-515.
15. Friedman DS, Okeke CO, Jampel HD, et al. Risk factors for
poor adherence to eyedrops in electronically monitored
patients with glaucoma. Ophthalmology 2009;116:1097-105. Crossref
16. Wu HY, Yin JF. Clinical investigation of medication
adherence of glaucoma patients [in Chinese]. Zhonghua
Yan Ke Za Zhi 2010;46:494-8.