Hong
Kong Med J 2019 Jan;25(1):76–7; 76.e1-3
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Dynamic dual-source computed tomography imaging for
myocardial perfusion
Allen Li, MB, ChB, FHKAM (Radiology)1; YH
Chan, MB, BS, FHKAM (Medicine)2; BE Wu, MB, BS, FHKAM
(Medicine)3; CS Lam, MB, BS, FHKAM (Medicine)2
1 Department of Radiology and Nuclear
Medicine, Tuen Mun Hospital, Tuen Mun, Hong Kong
2 Department of Medicine and Geriatrics,
Pok Oi Hospital, Yuen Long, Hong Kong
3 Department of Medicine and
Therapeutics, Prince of Wales Hospital, Shatin, Hong Kong
Corresponding author: Dr Allen Li (liallen@yahoo.com)
A 54-year-old man who was an ex-smoker was admitted
to Pok Oi Hospital in August 2015 with acute chest pain that was
subsequently confirmed to be a non-ST elevation myocardial infarction.
Echocardiogram revealed anterior wall hypokinesia. Computed tomography
(CT) coronary angiography demonstrated chronic total occlusion of the
right coronary artery and a 90% stenotic lesion in the proximal to mid
left anterior descending artery that was deemed to be the culprit lesion.
Percutaneous coronary intervention was subsequently performed with a
drug-eluting stent deployed across the proximal to mid left anterior
descending artery stenosis. Angiographic results were excellent.
At clinical follow-up, the patient complained of
persistent chest discomfort. Repeated echocardiogram was unremarkable
showing normal left ventricular function without any regional wall motion
abnormality. A CT stress myocardial perfusion and viability study was
requested to guide subsequent management. The study protocol included
quantitative evaluation of myocardial perfusion with pharmacological
stress using a dynamic approach, followed by a delayed scan for the
presence or absence of late myocardial enhancement.
Adenosine stress myocardial perfusion study with
colour-coded maps demonstrated perfusion defects in the apicoseptal
segment, the mid-inferoseptal segment, and to a lesser extent the basal
inferoseptal segment (Fig 1). For quantitative evaluation, the normal
areas had a myocardial blood flow of approximately 128 mL/100 mL/min,
whereas areas with ischaemia had a flow of around 40 mL/100 mL/min. No
delayed enhancement of the corresponding segments was evident to suggest
scarring due to prior myocardial infarction (Fig 2).
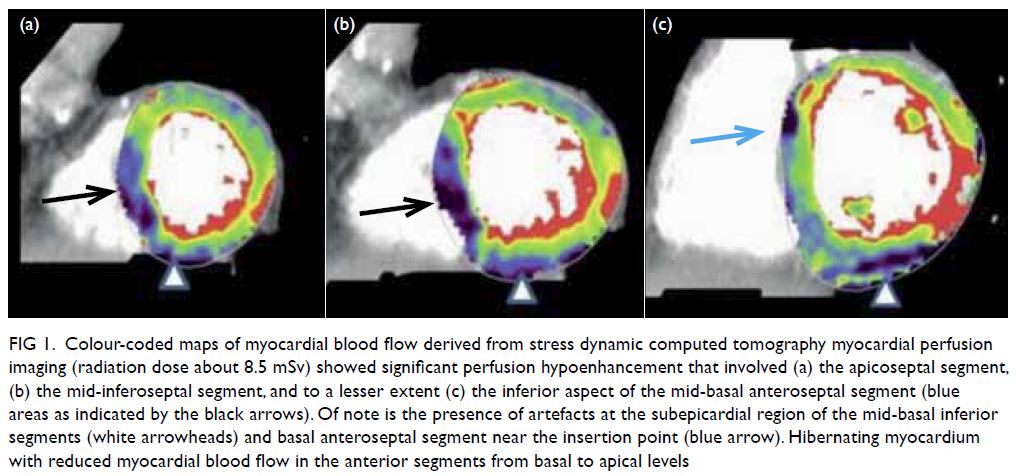
Figure 1. Colour-coded maps of myocardial blood flow derived from stress dynamic computed tomography myocardial perfusion imaging (radiation dose about 8.5 mSv) showed significant perfusion hypoenhancement that involved (a) the apicoseptal segment, (b) the mid-inferoseptal segment, and to a lesser extent (c) the inferior aspect of the mid-basal anteroseptal segment (blue areas as indicated by the black arrows). Of note is the presence of artefacts at the subepicardial region of the mid-basal inferior segments (white arrowheads) and basal anteroseptal segment near the insertion point (blue arrow). Hibernating myocardium with reduced myocardial blood flow in the anterior segments from basal to apical levels
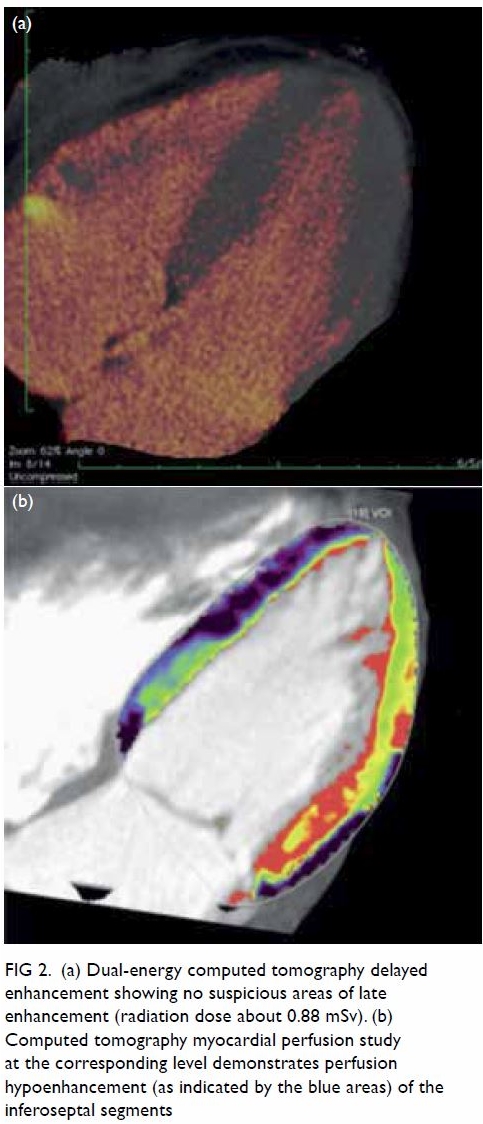
Figure 2. (a) Dual-energy computed tomography delayed enhancement showing no suspicious areas of late enhancement (radiation dose about 0.88 mSv). (b) Computed tomography myocardial perfusion study at the corresponding level demonstrates perfusion hypoenhancement (as indicated by the blue areas) of the inferoseptal segments
Eventually the patient underwent a percutaneous
coronary intervention to the chronic total occlusion of the right coronary
artery in 2016 via a combined radial and femoral arterial approach with
successful stent deployment across the occluded segment. Final angiography
showed excellent results with mild residual stenosis in patent ductus
arteriosus ostium (Fig 3). To date, the patient remains symptom-free
with improvements in both his exercise tolerance and mood, and psychiatric
reports revealing reduced dosage of antidepressants.
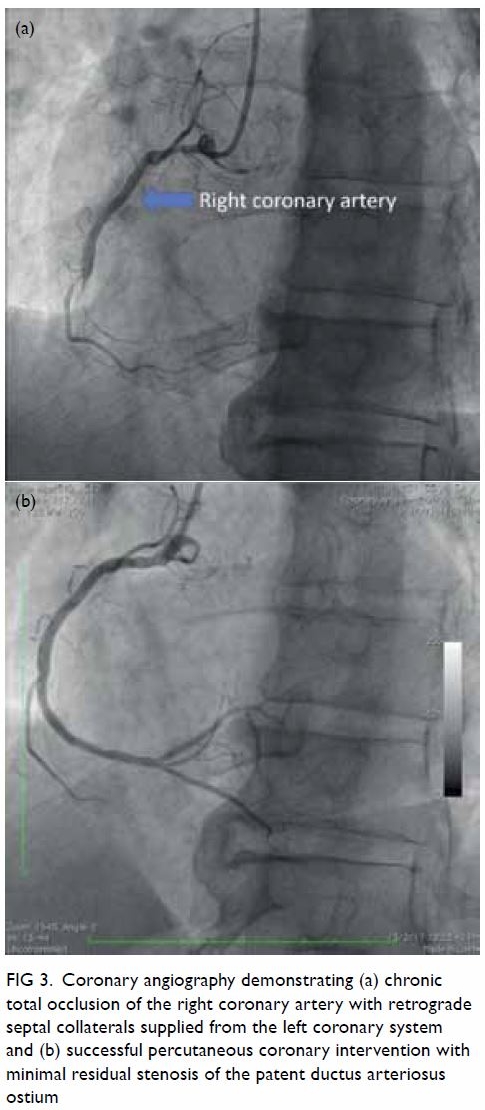
Figure 3. Coronary angiography demonstrating (a) chronic total occlusion of the right coronary artery with retrograde septal collaterals supplied from the left coronary system and (b) successful percutaneous coronary intervention with minimal residual stenosis of the patent ductus arteriosus ostium
Discussion
Various imaging modalities are available for stress
myocardial perfusion assessment.1
The present case demonstrates how a state-of-the-art dynamic and
quantitative assessment of myocardial perfusion using a dual-source CT
scanner enables detection of ischaemia along with viability assessment in
a rapid and non-invasive fashion within an acceptable radiation dose.2
Conventional “static” CT myocardial imaging allows
visual qualitative assessment of a single snapshot of myocardial iodine
contrast attenuation that requires precise timing of the arrival of
contrast to preserve diagnostic integrity. With a dual-source CT,
quantitative assessment of myocardial perfusion in multiple cardiac phases
with precise anatomic localisation of the ischaemic area becomes possible.
To date, many studies have assessed the reliability of dual-source
multiple-detector CT in the dynamic and quantitative evaluation of
myocardial perfusion.2 3 4 5
Stress CT myocardial perfusion is emerging as a
potentially promising non-invasive technique to detect myocardial
ischaemia both qualitatively and quantitatively. With new-generation
multiple-detector CT scanners, a one-stop non-invasive comprehensive
evaluation of the heart including the coronary artery, ventricular
function, myocardial perfusion, and viability is possible. Stress CT
myocardial perfusion provides incremental benefit to standard coronary CT
angiography, particularly for intermediate coronary lesions.2
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design: All authors.
Acquisition of data: A Li, YH Chan.
Analysis of data: A Li, YH Chan.
Drafting of manuscript: A Li, YH Chan.
Critical revision for important intellectual content: All authors.
Acquisition of data: A Li, YH Chan.
Analysis of data: A Li, YH Chan.
Drafting of manuscript: A Li, YH Chan.
Critical revision for important intellectual content: All authors.
Conflicts of interest
All authors have disclosed no conflicts of
interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
References
1. Ko SM, Hwang HK, Kim SM, Cho IH.
Multi-modality imaging for the assessment of myocardial perfusion with
emphasis on stress perfusion CT and MR imaging. Int J Cardiovasc Imaging
2015;31(Suppl 1):1-21. Crossref
2. Rossi A, Dharampal A, Wragg A, et al.
Diagnostic performance of hyperaemic myocardial blood flow index obtained
by dynamic computed tomography: does it predict functionally significant
coronary lesions? Eur Heart J Cardiovasc Imaging 2014;15:85-94. Crossref
3. Kim SM, Choi JH, Chang SA, Choe YH.
Additional value of adenosine-stress dynamic CT myocardial perfusion
imaging in the reclassification of severity of coronary artery stenosis at
coronary CT angiography. Clin Radiol 2013;68:659-68. Crossref
4. Bamberg F, Becker A, Schwarz F, et al.
Detection of hemodynamically significant coronary artery stenosis:
incremental diagnostic value of dynamic CT-based myocardial perfusion
imaging. Radiology 2011;260:689-98. Crossref
5. Varga-Szemes A, Meinel FG, De Cecco CN,
Fuller SR, Bayer RR 2nd, Schoepf UJ. CT myocardial perfusion imaging. AJR
Am J Roentgenol 2015;204:487-97. Crossref

