© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Bilateral lumbar hernia
Iris Chung, MB, BS, MHKICBS1; KY Wong,
FRCSEd, FHKAM (Surgery)2
1 Department of Surgery, Queen Mary
Hospital, Pokfulam, Hong Kong
2 Department of Surgery, Tung Wah
Hospital, Sheung Wan, Hong Kong
Corresponding author: Dr Iris Chung (iris.ihtc@gmail.com)
Lumbar hernias were proposed in 1672 by Barbette
but the first case was not published until 1731 wherein Garangeot reduced
a lumbar hernia during autopsy1;
the first repair was conducted 19 years later by Ravaton.2 The lumbar region, formed by the twelfth rib, iliac
crest, erector spinae, and external oblique denotes the site for
herniation. Lumbar hernias are most commonly categorised anatomically, as
superior lumbar hernia (Grynfeltt-Lesshaft triangle), inferior lumbar
hernia (Petit triangle), or diffuse involvement. Other classifications
include aetiology (primary or secondary) and sac content (extra-, para- or
intra-peritoneal); however, none of these categorisations have any
treatment value. In 2007, Moreno-Egea et al2
proposed a preoperative classification with surgical implications (hernia
size, location, content, aetiology, muscle atrophy and recurrence), but
this has yet to be universally applied.
Owing to the rarity of lumbar hernia, a surgeon may
only come across one case throughout their career.3 With only 300 cases reported, they comprise less than
2% of all abdominal hernias.3
Bilateral occurrences are even less frequently documented, with the first
primary and secondary cases published in 2002 by Karmani et al4 and in 2006 by Bhasin et al5, respectively. Tung Wah Hospital performs an average of
500 hernia repairs annually, the majority of which are inguinal hernias;
repair of lumbar hernias is uncommon, owing to their low incidence. Our
most recent experience was in March 2017 when a 66-year-old man was
referred to our centre for incidental finding of painless swellings over
bilateral flanks which spontaneously reduced when the patient was supine;
cough impulses were present. Aside from injuring his right lower ribs 2
months prior to presentation (treated conservatively), there was no trauma
or surgical history. His past health includes hyperlipidaemia, benign
prostatic hyperplasia, and obstructive sleep apnoea. His body mass index
was 23 kg/m2. A clinical diagnosis of bilateral reducible
superior lumbar hernias (within the Grynfeltt-Lesshaft triangle) was made
(Fig 1). Prior to consulting us, the patient
underwent computed tomography imaging with findings compatible with our
diagnosis. Open repair was performed under general anaesthesia with the
patient lying prone. Dissection of the latissimus dorsi muscle via a
linear incision revealed the hernias bounded superiorly by the twelfth
rib, anteriorly by the posterior border of the internal oblique muscle,
and posteriorly by the anterior border of the sacrospinalis muscle.
Defects of 3 cm and 1.5 cm within the right and left superior lumbar
triangle, respectively, were delineated; the sacs contained
retroperitoneal fat and were easily reduced (Fig 2). Primary closure was performed with
interrupted non-absorbable sutures, and an onlay polypropylene mesh
anchored to the thoracolumbar fascia for reconstruction. No drain was
inserted. Postoperative recovery was uneventful, and the patient was
discharged from the hospital the following day. Interval follow-up
reported no complications including wound infection, pain, or recurrence.
Cosmetically, the patient was satisfied and remained asymptomatic on
latest consultation.
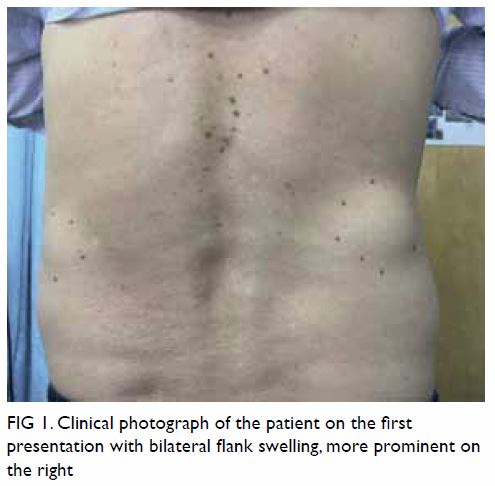
Figure 1. Clinical photograph of the patient on the first presentation with bilateral flank swelling, more prominent on the right
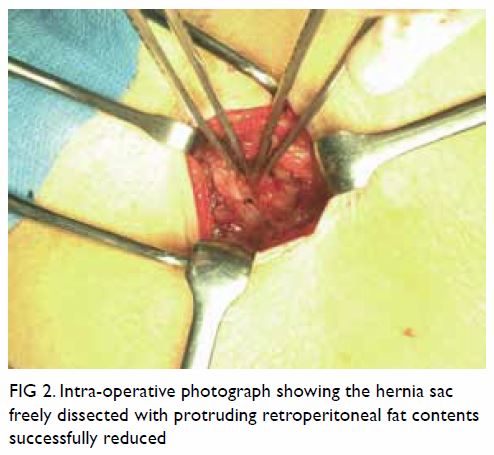
Figure 2. Intra-operative photograph showing the hernia sac freely dissected with protruding retroperitoneal fat contents successfully reduced
Lumbar hernias are usually asymptomatic or present
with non-specific complaints such as back or abdominal discomfort. A
reducible mass with cough impulse may not always be present. Low suspicion
can lead to misdiagnosis of alternative soft tissue pathologies like
lipomas or retroperitoneal tumours. Sac contents can range from empty to
intra- or retro-peritoneal organs, which can produce atypical signs such
as intestinal or urinary obstruction. Symptoms of back or abdominal pain
with no obvious localising signs should suggest lumbar hernias as a
differential, especially if there are risk factors. In all, 14% of cases
have coexisting abdominal wall hernias; therefore, these patients should
be screened.6 Imaging, such as
computed tomography, can reveal any disrupted abdominal wall muscle
layers, sac contents, and concomitant hernias. Although the physical
findings were straightforward in our patient, the available imaging
contributed towards diagnostic certainty, and we recommend the use of
imaging to aid with preoperative planning.
In all, 20% of lumbar hernias are congenital,
possibly from weakness in the abdominal muscle aponeurosis during
development.7 The remaining 80% are
acquired spontaneously (primary) or from preceding events (secondary).7 Associated risks include old age with weak abdominal
muscles due to ageing; obesity and chronic respiratory conditions that
increase intra-abdominal pressures; and extreme weight loss that decreases
fat content, resulting in rupture of the twelfth neurovascular bundle
orifice. Abdominal muscle weakening in secondary hernias can be due to
trauma, infection, or postoperative complications from inadequate closure
or subcostal nerve injury. Strangulation is rare as the neck is typically
wide; however, reported incarceration rates are as high as 25%, with 9% of
acquired cases presenting acutely.1
Historically, the use of flaps was incorporated in
lumbar hernia repair, as introduced by Dowd in 1907.2 It was not until the
1950s to 60s when Thorek8 and
Hafner et al9 advocated the use of
a mesh, and the 1990s when laparoscopic repairs were proposed by Burick
and Parascandola.10 With limited
cases to compare surgical approaches, the ideal method is inconclusive.
Operative approaches largely depend on available facilities and the
surgeons’ expertise. Primary closure with interrupted tension-free sutures
has been advocated for small defects, whereas larger hernias may be
repaired using a non-absorbable mesh with or without anchoring to the
twelfth rib or iliac crest.11 Mesh repairs have been suggested to reduce
rates of recurrence, especially for patients in whom hernia occurrence is
related to muscular atrophy or major deformities.5
In particular, sublay placement has been advocated for protecting the
hernia orifice with help of underlying intra-abdominal pressure. Some
centres suggest a double mesh technique whereby an onlay mesh is
incorporated with a sublay mesh to ensure inclusion of the lower edge of
the iliac crest, because this bony limit often impedes proper placement of
mesh to fully cover the defect.5 12 Laparoscopic repair with a
sublay mesh via various transabdominal and extraperitoneal approaches have
been explored but no meaningful comparisons have been made to conclude any
definite advantages among laparoscopic approaches or in relation to open
approaches.
Owing to their rarity, lumbar hernias are easily
missed and misdiagnosed. High clinical suspicion is needed to avoid
treatment delay. There is no recommendation for the ideal method of
repair; therefore, surgical approaches should be tailored according to
patient preference and surgeons’ experience in managing this disease. If
laparoscopic expertise is not available, open mesh repair is a safe
alternative with satisfactory outcomes for small defects, as demonstrated
in our patient.
Author contributions
All authors contributed to the concept and design
of the study, acquisition of data, and interpretation of data, critical
revision of the manuscript for important intellectual content. I Chung
drafted the manuscript. All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of
interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Approval from an institutional review board or
ethics committee was not required because our study did not involve
clinical trials on human subjects. Any patient identifiers have been
removed.
References
1. Petersen K, Snikeris J, Hall TS.
Bleichner’s hernia—lumbar hernia. Am J Case Rep 2013;14:26-9. Crossref
2. Moreno-Egea A, Baena EG, Calle MC,
Martínez JA, Albasini JL. Controversies in the current management of
lumbar hernias. Arch Surg 2007;142:82-8. Crossref
3. Ploneda-Valencia CF, Cordero-Estrada E,
Castañeda-González LG, et al. Grynfelt-Lesshaft hernia a case report and
review of the literature. Ann Med Surg (Lond) 2016;7:104-6. Crossref
4. Karmani S, Ember T, Davenport R.
Congenital lumbar hernias: A case report. J Pediatr Surg 2002;37:921-2. Crossref
5. Bhasin SK, Khan AB, Sharma S. Bilateral
petit’s triangle hernia. JK Science 2006;8:163-4.
6. Fokou M, Fotso P, Ngowe Ngowe M, Essomba
A, Sosso M. Strangulated or incarcerated spontaneous lumbar hernia as
exceptional cause of intestinal obstruction: case report and review of the
literature. World J Emerg Surg 2014;9:44. Crossref
7. Stamatiou D, Skandalakis JE, Skandalakis
LJ, Mirilas P. Lumbar hernia: surgical anatomy, embryology, and technique
of repair. Am Surg 2009;75:202-7.
8. Thorek M. Lumbar hernia. J Int Coll Surg
1950;14:367-93.
9. Hafner C, Wylie J Jr, Brush BE. Petit’s
lumbar hernia: repair with Marlex mesh. Arch Surg 1963;86:180-6. Crossref
10. Burick AJ, Parascandola S.
Laparoscopic repair of a traumatic lumbar hernia: a case report. J
Laparoendosc Surg 1996;6:259-62. Crossref
11. Esposito C, Settimi A, De Marco M, et
al. Congenital lumbar hernia: two case reports and a review of the
literature. J Paediatr Surg Spec 2009;3:40-2.
12. Bigolin AV, Rodrigues AP, Trevisan CG,
et al. Petit lumbar hernia—a double-layer technique for tension-free
repair. Int Surg 2014;99:556-9.

