© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
SPECIAL ARTICLE
Medical history of Hong Kong
Introduction—Anatomy of a city: why Hong
Kong’s history of medicine matters now
Ria Sinha, BSc, PhD
Medical Ethics and Humanities Unit, School of Clinical Medicine, The University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr Ria Sinha (riasinha@hku.hk)
As COVID-19 fades from view, the most significant
pandemic of the 21st century is already being
written into history. Hong Kong’s experience of
the coronavirus outbreak was both local and yet
enmeshed in global networks of disease transmission,
biomedicine, technology, geopolitics and public
response. How one wonders, will the story be told
to future generations of schoolchildren, medical
students, health professionals and the public? Over
time, a singular narrative often emerges, defined by
the major events of the outbreak, with the messiness
of everyday details, early public uncertainty, frequent
policy changes and misinformation gradually erased
from memory. Given the mountain of information
that emerged and changed on a daily basis, this is
inevitable, but medical historiographies should
preserve this complexity to ensure a balanced and
critical analysis of present and future events.
A maritime entrepôt frequently reshaped by
migration, imperial power, political turmoil, and
capitalist ambitions, Hong Kong has long been
at the mercy of local, regional and global health
threats. From 19th-century communicable diseases
to 21st-century pandemics and chronic health
conditions, from bacteriology’s early laboratories
to genomics and precision medicine, and from
missionary, government and private hospitals to a
plural public health system, the city’s medical story
is one of collisions and entanglements, between
people, pathogens, medical systems, institutions,
and technological innovation. This exciting and
timely new series on Hong Kong’s rich history of
medicine endeavours to bring diverse local archives
and stories to life, reminding us of the challenges of
the foregone medical landscape and the endeavours
of those who sought to construct the robust medical
system we benefit from today.
Challenges in health governance
and building local medical capacity
Countless medical and healthcare professionals
contributed to shaping local medical expertise, laying a foundation to serve the needs of a mixed
and growing population. Local capacity building was
often hampered by economic constraints imposed
by the British Government and the city was reliant
on transient doctors for much of the 19th century,
from naval surgeons to private practitioners, as
well as grassroots traditional Chinese medicine
practitioners who ministered to local and migrant
Chinese communities. Yet early medical practice
was challenging, and several Colonial Surgeons died
in service or from complications of repeated bouts
of sickness after leaving the colony.1 Efforts to unify
physicians and consolidate knowledge were initially
limited to Western medicine practitioners through
the formation of the China Medico-Chirurgical
Society, but diaries and journals show there was
professional interest in the healing properties of
Chinese medicine.2 Attempts to establish Western
medicine as a primary healthcare framework
for the majority Chinese population began with
early medical missionaries under the auspices of
the London Missionary Society, but success was
dependent on circumstance, government policies
and funding. There were also well-intentioned yet
culturally problematic endeavours to shoehorn
Chinese medicine, which was largely community
based, into an institutional model, as seen in the case
of Tung Wah Hospital, which opened in 1872 at the
heart of the Chinese community but was returned to
colonial oversight after the plague outbreak.3
A decisive development was the founding of the
Hong Kong College of Medicine for Chinese in 1887,
a forerunner of The University of Hong Kong’s Faculty
of Medicine. The College represented a loftier late
19th century effort to translate biomedical science
into Chinese settings, training local practitioners to
expand the reach of Western medicine into China.4
Women’s and children’s health nonetheless lagged
behind and was dependent on the timely presence
and dogged determination of individuals such as Dr
Alice Hickling, who galvanised government support
and funding for maternity services.5 Mental health,
too, has a long and troubled history in Hong Kong,
complicated by a lack of knowledge, appropriate facilities and empathy towards the afflicted.6 The
subsequent establishment of large teaching hospitals
promoted the professionalisation of nursing, the
emergence of more locally trained physicians and
allied health professionals, and ultimately led to
the formation of the Hospital Authority in 1990 to
manage public hospitals. This gradually expanded
and embedded medical practices in the city’s social
fabric, while connecting Hong Kong to British,
Chinese, and global networks.
Hong Kong as a node in local and
global medical history
Hong Kong’s history situates local practice within
global circuits of knowledge, and few cities
exemplify the globality of medicine as vividly as
Hong Kong. The territory has always been a hub,
a place of opportunity, trade and new beginnings
propelled by high mobility. As the population grew
and communication and transportation channels
expanded, port health controls became essential to
screen for deadly diseases such as smallpox, various
febrile diseases, and distant threats such as yellow
fever. Syphilis was a prime example of a well-travelled
and much-feared sexually transmitted disease that
quickly became established in the squalid brothels
and among unregulated sex workers, driven by a
gender imbalance and propagated by thousands of
transiting naval personnel and Chinese immigrants.7
Such episodes compelled the instatement of
successive, though sometimes repressive, health
policies to manage the situation and treat the afflicted. The colonial government frequently drew
on British experiences and laws as a remedy but was
often unprepared for the challenges of governing a
multicultural population.
The colonial port’s early public health regimen
was severely tested during the 1894 bubonic plague,
an outbreak that began in Yunnan, China, and
spread along trade routes to reach the overcrowded
residential districts of Hong Kong before extending
to India and around the globe. The Hong Kong
outbreak drew international scientific teams to
the territory and sparked debates over science and
urban sanitation methods that often intersected
with racialised assumptions and coercive policies.
It is a history that has been retold through multiple
disciplinary perspectives and invites ethical
reflection, but the crisis undoubtedly catalysed
extensive and controversial sanitary reforms, urban
planning and biomedical infrastructure development
to facilitate homegrown laboratory-based public
health.8 Socio-medical transformations following
the outbreak reinforced how crisis events can shape
public health policies for generations.
The late 20th century brought fresh forms of
global interdependence and collaboration. The 1997
H5N1 avian influenza outbreak underscored the
city’s international role in pandemic surveillance
and the fragile boundaries between human and
animal health.9 Six years later, SARS (severe acute respiratory syndrome) swept through
hospitals, housing estates, and international
flight paths, exposing the vulnerabilities of dense
urban living and rapid global mobility. Hong Kong
scientists, epidemiologists, medical professionals, and public health officials were pivotal in identifying
the causative pathogens, sharing information,
and controlling the outbreak.10 The aftermath saw
institutional reforms, including the establishment
of the Centre for Health Protection, and a durable
model for infection control and public health
governance that was tested during COVID-19.
Why preserving this history
matters now and for the future
Juggling a packed curriculum, medical students have
questioned why they should spend time learning
medical history. There are many pertinent responses,
but one that seems particularly relevant is that
history affords a critical perspective on medicine,
professional culture, identity and practice.11 One of
the most effective ways to actuate this is by embedding
interactive engagement into the curriculum through
field trips to museums, designing walking tours,
and encouraging self-directed research and learning
activities. Hong Kong is blessed with a fantastically
rich medical heritage, and witnessing this history
in the community and on the streets is a powerful
experiential tool to stimulate self-awareness, inspire
lifelong learning, and promote knowledge exchange
between health practitioners and the public. Indeed,
some medical historiographies demand reflection to
avoid future error. Trust is partly historical memory,
preserving and sharing authentic, accessible
historical narratives through museums, archives,
journals and innovative curricula that can stimulate
more participatory and forward-thinking forms of
health governance.
History also permits us to see into the future,
not in the conventional sense of ‘learning lessons
from the past’, which can be a problematic trope,
but in understanding local vulnerabilities to disease
and gaps in infrastructure or expertise. The recent
opening of a flagship Chinese Medicine Hospital
in Tseung Kwan O is testament to a post-handover
revival of traditional Chinese medicine, driven
by the Chinese Medicine Ordinance (Cap 549)
and the persistence of local healing cultures in the
community. Today, a visit to Watson’s pharmacy,
one of the oldest (Western medicine) dispensaries
in Hong Kong dating to the 1840s, reveals an array
of prepackaged Chinese medicines and a Chinese
medicine consultation booth. The question of
medical pluralism and potential for integrating these
divergent medical frameworks is an interesting one
that will benefit from further examination of their
historical coexistence.
To conclude, Hong Kong’s medical evolution
has been nothing short of remarkable, characterised
by local idiosyncrasies within a broader global
health network. Preserving and disseminating Hong Kong’s rich medical history is both a
collective responsibility and an opportunity
for interdisciplinary knowledge exchange.
Professionally, historical literacy supports leadership
and informs decision making and policy design. By
working together, health professionals and historians
can co-translate scattered memories into shared
knowledge, and shared knowledge into better care
and medical development. In a period of fast-moving
technological innovation, it is more important than
ever to capture local histories as a window to Hong
Kong’s medical development legacy and to avoid
the perpetuation of inaccurate information and
sources.
This series invites clinicians, nurses, allied
health professionals, public health practitioners, and
students to read Hong Kong’s medical past not as a
linear story but as a critical reflection that informs
medical and scientific progress. Many health topics
deserve historical attention and are too many to
discuss in this brief introduction, but a diverse series
will surely emerge. Upcoming articles will build
on existing histories of medicine, enriching Hong
Kong’s material culture of medicine and inspiring
a new generation of custodians. In a city where
the future is always arriving early, history can be a
valuable partner in foresight.
References
1. Lim P. Forgotten Souls: A Social History of the Hong Kong
Cemetery. Hong Kong: Hong Kong University Press; 2011:
145-9. Crossref
2. Rydings HA. Transactions of the China Medico-
Chirurgical Society, 1845-6. J Hong Kong Branch R Asiat
Soc 1973;13:13-27.
3. Sinn E. Power and Charity: A Chinese Merchant Elite in
Colonial Hong Kong. Hong Kong: Hong Kong University
Press; 2003. Crossref
4. Ching F. 130 Years of Medicine in Hong Kong: From the
College of Medicine for Chinese to the Li Ka Shing Faculty
of Medicine. Singapore: Springer; 2018. Crossref
5. Chan-Yeung M. Dr Alice Hickling (1876-1928): the doctor
who changed the paradigm of maternal care in Hong Kong.
Hong Kong Med J 2021;27:389-91. Crossref
6. Wu HJ. From means to goal: a history of mental health
in Hong Kong from 1850 to 1960. In: Minas H, Lewis M,
editors. Mental Health in China and the Chinese Diaspora:
Historical and Cultural Perspectives. Cham, Switzerland:
Springer; 2021: 69-78. Crossref
7. Tsang CC. Hong Kong’s floating world: disease and crime
at the edge of empire. In: Peckham R, editor. Disease
and Crime: A History of Social Pathologies and the New
Politics of Health. Routledge; 2014: 21-39.
8. Hong Kong Museum of Medical Sciences Society. Plague,
SARS and the Story of Medicine in Hong Kong. Hong
Kong: Hong Kong University Press; 2006: 147-224.
9. Malik Peiris JS, de Jong MD, Guan Y. Avian influenza virus
(H5N1): a threat to human health. Clin Microbiol Rev
2007;20:243-67. Crossref
10. Peiris JS, Lai ST, Poon LL, et al. Coronavirus as a possible
cause of severe acute respiratory syndrome. Lancet
2003;361:1319-25. Crossref
11. Nagornykh O. Integrating the history of medicine into modern medical education: evidence-based structures,
methods, and relevance. 28 May 2025. Available from:
http://dx.doi.org/10.2139/ssrn.5274761. Accessed 10 Jan 2026.
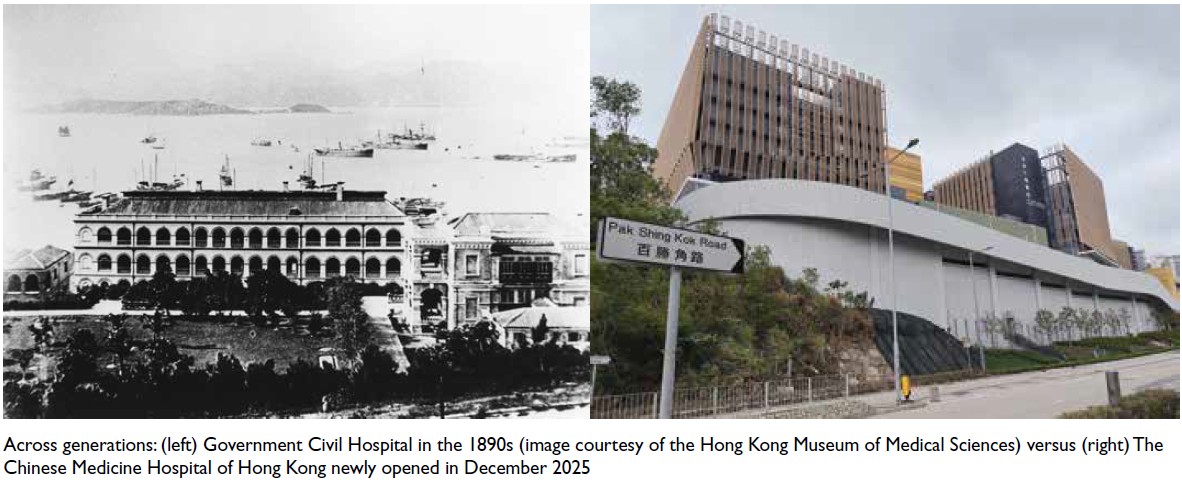
Across generations: (left) Government Civil Hospital in the 1890s (image courtesy of the Hong Kong Museum of Medical Sciences) versus (right) The Chinese Medicine Hospital of Hong Kong newly opened in December 2025

