© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
HEALTHCARE FOR SOCIETY
The Hong Kong Hospital Authority reform: a historical perspective
Part 2: From reform blueprint to practice
Part 2: From reform blueprint to practice
William SW Ho, FCSHK, FHKCCM
Hong Kong College of Community Medicine, Hong Kong SAR, China
Preface
The previous article (Part 1) in this series1 describes
the historical transition of Hong Kong’s public
hospital system from being part of the Civil Service
to a separate corporatised entity established by
statute, charged with modernising its management
and service quality. After the Hong Kong Hospital
Authority (HA) was inaugurated on 1 December
1990, it took merely 12 months of preparation for
the takeover of the entire public hospital system
overnight on 1 December 1991. This article describes
how the Authority turned the ambitious blueprint
laid down in the Scott Report,2 further modified and
elaborated in the Provisional Hospital Authority
(PHA) Report,3 into reality.4 Current HA staff may
be amazed that so many systems and processes that
have long been taken for granted were once non-existent.
This historical account may give not only
an understanding of how the existing practices came
about, but also a useful case study in healthcare
organisational management.
Comprehensive reform dimensions
Mission and strategies
For the first time, the public hospital system
had a mission statement as laid down by the HA
Board after a 3-day workshop in February 1991,5
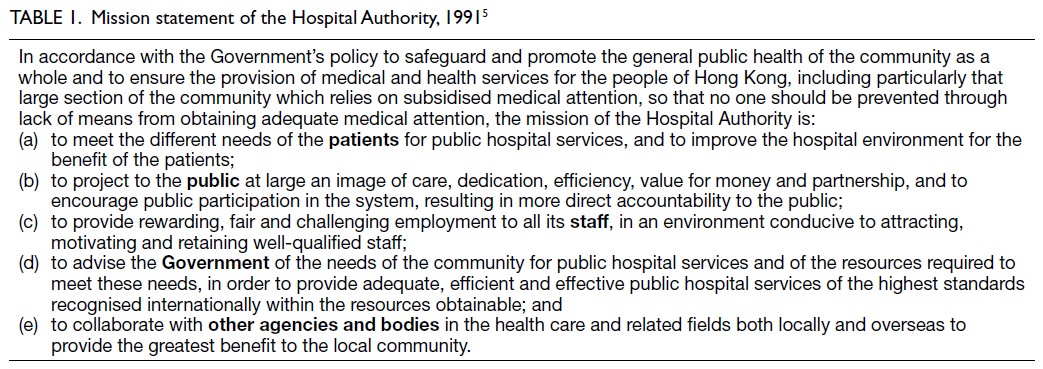
developed according to the organisational function spelt out in the HA Ordinance (Table 1). This
rather lengthy mission statement merely reiterates
upfront the communitarian healthcare policy of
the Government, and goes on to enunciate the
Authority’s responsibility towards each of the major
stakeholder parties.
From this first version of the mission
statement, major strategies were derived, which
served to focus the whole organisation on priority
goals and targets to improve population health and
service quality. This was a far cry from the past,
when there were hardly any coordinated directions
beyond simple bed-to-population or manpower
ratios to cope with population growth, and where
service improvements were heavily influenced by
the preferences of powerful medical consultants and
their respective political clout in securing resources
within the former Medical and Health Department.
Three levels of governance
Empowered by the HA Ordinance, the Government-appointed
Members of the HA (commonly referred
to collectively as the HA Board) governed all
public hospitals independently of the Civil Service,
thus enjoying much greater flexibility in the use
of available funds and the management of human
resources, while accountable to the Secretary for
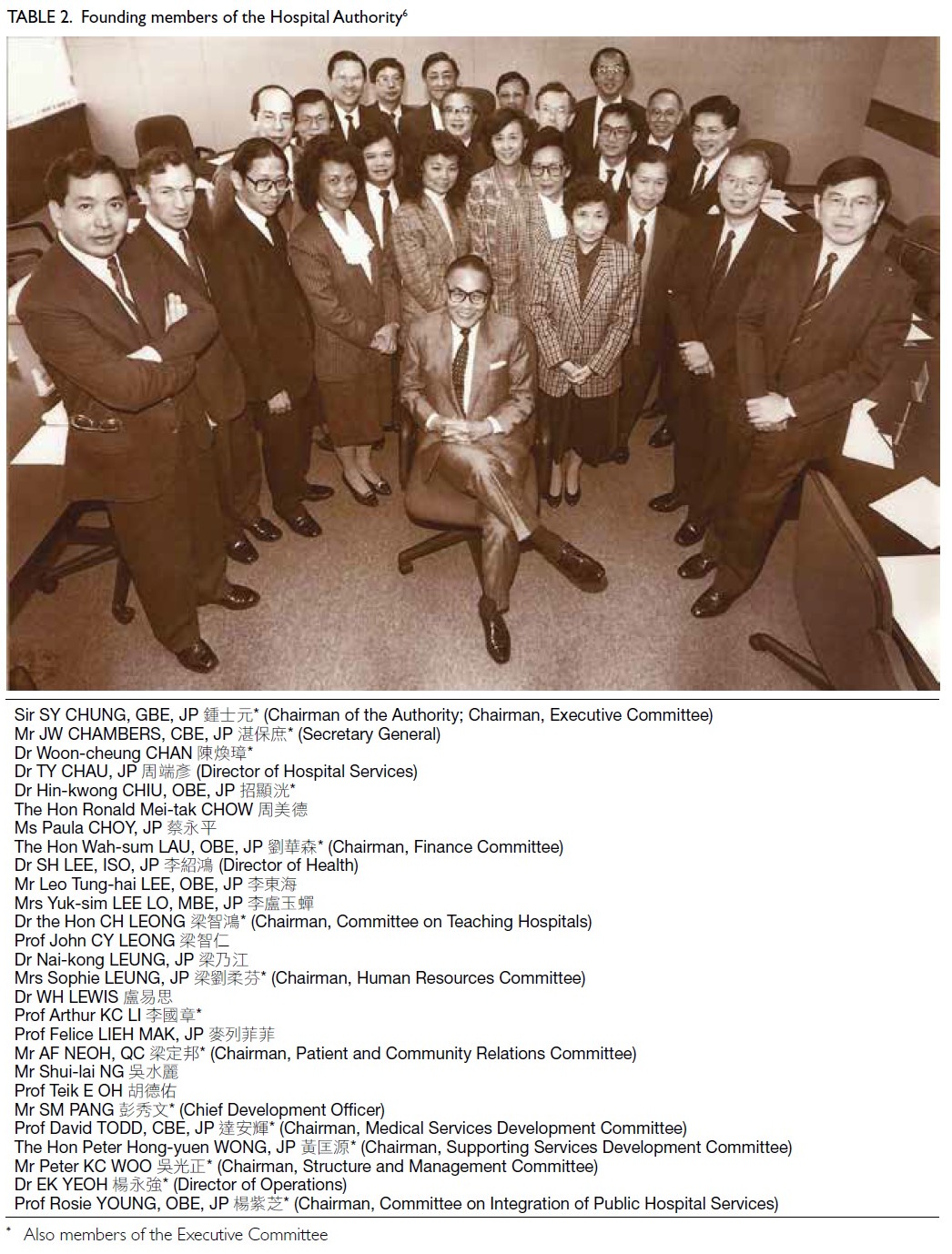
Health and Welfare. The Chairman of the PHA, Sir Sze-yuen Chung 鍾士元爵士, was reappointed as
Chairman of the HA (Table 26).
Eight functional committees under the HA
Board served to introduce external expertise
and steer managerial modernisation in specific
areas. The chairmen and vice-chairmen of these committees together with the three principal officers
constituted an Executive Committee, which was the
chief decision-making body of the Authority chaired
by the HA Chairman. In addition, an independent
Public Complaints Committee was established to
deal with appeal cases not settled at the hospitals.
At the second level, three Regional Advisory
Committees were established to enable community
participation. At the third level, each hospital was
governed by a Hospital Governing Committee with
the introduction of community leaders. For Schedule
2 (ex-subvented) hospitals, the parent body would
nominate a two-thirds majority of the members
(with the rest appointed by the HA) and would chair
the Hospital Governing Committee.
Two levels of management
The previous three-tiered structure of the Medical
and Health Department—Headquarters, Regional
Offices, and Hospitals—was simplified into two
levels to enhance efficiency and hospital autonomy.
The Regional Offices were abolished with their staff
absorbed into the HA Head Office.
Management structure: Head Office level
A tripartite top management structure of principal
officers—Director of Operations, Chief Development
Officer, and Secretary General—was initially
adopted, reporting to the Executive Committee
of the HA Board, until a suitable candidate for the
Chief Executive (CE) position emerged.
The appointment of the three principal officers
was completed upon the HA’s establishment on 1
December 1990. There was a balanced mix of talents.
The Director of Operations, Dr EK Yeoh 楊永強, was
a senior medical consultant recruited from within the
system. The Chief Development Officer, Mr SM Pang
彭秀文, was an experienced hospital administrator
recruited from Australia. The Secretary General, Mr
John Chambers 湛保庶, was former Secretary for
Health and Welfare from the Administrative Officer
rank of the Civil Service. Recruitment of various
deputies was also completed by the time the HA
formally took over the operations of all hospitals on
1 December 1991. Dr Yeoh was eventually appointed
to the CE position in 1994.
Management structure: Hospital level
Under the new management structure, each hospital
was headed by a Hospital Chief Executive (HCE),
with more power and autonomy than the previous
Medical Superintendents, and assisted by a number
of General Managers in clinical and business
functions. The HCEs reported directly to the CE
of the HA. Appointment of HCEs went through
a nurturing process, assisted by a Management
Transformation Implementation Task Force from the
Head Office. The first batch of HCEs was appointed
in March 1992, and appointments for all other
hospitals were largely completed within 3 years.
Eighteen of the newly appointed HCEs were senior
doctors, reflecting a major effort by the HA to bring
new blood into management roles from clinicians within the system. Seventeen other HCEs were
former Medical Superintendents, and four HCEs of
smaller hospitals came from nursing or allied health
backgrounds.7 Internal hospital appointments to new
management positions and structural remodelling
followed accordingly.
Each clinical department was headed by a
Chief of Service, who reported to the HCE, and was
assisted by a Departmental Operations Manager
(DOM) who would be a senior nurse.8 Each ward
was headed by a Ward Manager, also a senior nurse,
who reported to the DOM. All nurses working in a
clinical department therefore ultimately reported
to the Chief of Service as part of an integrated
multidisciplinary team, rather than to the Chief
Nursing Officer in a hierarchical manner as in the old
days. The General Manager (Nursing), who replaced
the Chief Nursing Officer position, became part of
the HCE’s top management team and no longer held
line authority over the DOMs.
Under the new management culture, an inverted
pyramid model was advocated, where frontline
clinical units were regarded as the most important
and better supported by the revamped management
structure and capabilities.9 Decentralisation of
decision making and participatory management
were to be encouraged.
Staffing
No reform would be successful by merely putting
old wine in new bottles. Whatever new mission
statement, management positions, systems and
processes were put in place would need to be
embraced and operationalised by the very people
within the system. Given the staff unions’ animosity
towards the old regime and suspicion of the new,
as reflected in Part 1 of this series,1 winning them
over was of utmost importance. An attractive new
remuneration package would be a crucial first
step. On the other hand, as the Government would
ultimately shoulder the HA’s staff costs, consideration
should be given to the long-term financial burden
and comparability with Civil Service terms.10 Both
fronts had to be tackled by the HA.
Under the principle of “what the total cost to
Government of running the service would be had all
staff been given Civil Service terms”, the approach was
taken to divide all staff in the former Government
hospital system into pay bands for separate analysis,
as the ‘fringe benefits’ differed across bands. An
arbitrary snapshot of the situation as at 1 April 1989
was taken to calculate the total cost per staff band,
divided by the number of staff members to yield the
averaged-out cost per staff member in that band.
This would form the basis for constructing the new
HA staff terms ‘at comparable cost’.11
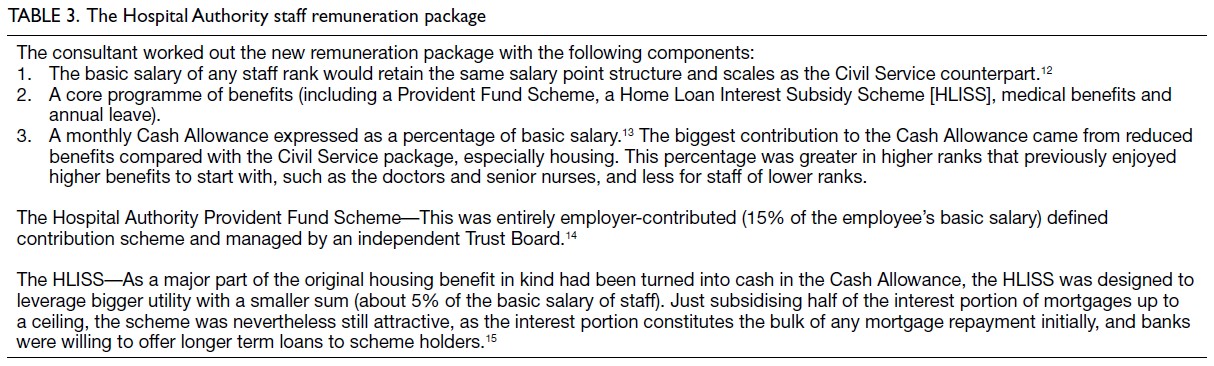
The PHA engaged Tower, Perrin, Forster
and Crosby to develop a new HA remuneration package (Table 312 13 14 15). To increase its attractiveness,
the idea was to change the pension portion into a
Provident Fund arrangement that would be invested
to generate a higher yield, and to reduce housing
and other ‘in kind’ benefits so as to translate more
of these into cash. Amid the booming economy at
the time, immediate cash, despite the ‘averaging
out’ effect, was often more attractive than potential
in-kind benefits, and certainly much more flexible
for the staff. Whether existing staff would choose to
switch over was a matter of individual consideration.
Having settled the new HA terms, another
challenge arose concerning the ‘bridging over’
arrangement for Civil Servants in Schedule 1 (ex-Government) hospitals opting into the new terms.
Unlike staff employed in Schedule 2 (ex-subvented)
hospitals who could simply take out their respective
provident fund balances from their previous
employers to join the new HA package, those working
in Schedule 1 hospitals were mostly on permanent,
pensionable terms. The staff unions hoped for
some kind of ‘pay-off’ to sever the link with the
Civil Service before switching over to the new HA
package. This would however incur a large sum of
upfront payment from the Government. Moreover,
not all staff would work to retirement age and attract
a pension. The idea of a deferred pension emerged,
namely, one only obtainable upon retirement from
the HA and computed using the same methodology
of years of service (as Civil Servants) and the last
salary drawn before switching over to HA term.16
All existing staff were given an irrevocable
choice within 3 years to switch to the new HA terms
or remain in their existing terms. Irrespective of
terms, all would be subject to the same management
on a fair basis within the HA. By the end of the
option period, 99.5% of Schedule 2 hospital staff
and 58.1% of Schedule 1 hospital staff changed over
to the new terms, giving an overall figure of 74.8%.
The generally inferior original employment terms
in various Schedule 2 hospitals compared with their Civil Service counterparts explained the former’s
high conversion rate. Among former Civil Servants
in the system, lower-ranking staff bands with less
to gain from the new package tended to record
fewer switching. Some also suspected that staff on
HA terms might have less job security than Civil
Servants ‘protected’ by their strong unions.
For clarity, all new hires after the HA
took over operation of all public hospitals on 1
December 1991 were only offered the HA terms of
employment. Settling staff terms of employment
was just a prerequisite, raising staff understanding
and performance in the management reform was
most important to ensure success. Major resources
were thereby committed to support tailored
management training courses for senior, middle
and frontline clinical staff, equipping them with
the concepts and know-how to carry out their
new roles. Additional resources were put into the
professional training of clinical staff to enhance their
competence, job satisfaction and retention. There
were also specific training courses for other staff to
uplift their performance in areas such as customer
service and complaints management. Expansion
of management functions also meant introduction
of external expertise in a host of non-clinical areas
such as information technology (IT), finance, legal,
engineering, human resources and other areas of
general management.
With improved staff packages, training and
professional advancement opportunities, there was
an atmosphere of progression and high morale in
the new organisation. As a result, staff wastage rate
quickly dwindled.
Direct patient service improvements
On clinical services, task forces were formed to tackle
overcrowding, waiting time, accident and emergency
service improvements, nursing services, and more
on a territory-wide basis. Clinical Coordinating
Committees were formed for each clinical specialty to foster inter-hospital collaboration and service
planning to improve system-wide performance in
quality and efficiency.
Priority areas of improvement included better
inter-hospital cooperation for patient diversion
from the most severely overloaded Schedule 1
hospitals to Schedule 2 hospitals, as well as better
bed management within each hospital, resulting in
drastic reduction in ‘camp beds’. A triage system
was implemented in all accident and emergency
departments to ensure minimal waiting time for
urgent cases. Computerised booking system for
Specialist Outpatient Clinics and doubling of
effort to increase throughput led to shorter waiting
lists and improved access to specialist care. New
signages, open counters, upgraded furniture and
hospital environment, as well as air-conditioning
projects also completely transformed the image of
public hospitals.
Infrastructure and capacity building
The Pamela Youde Nethersole Eastern Hospital
was completed in 1993, eventually adding more
than 1800 beds to the eastern part of Hong Kong
Island. In view of the low bed-to-population ratio
in northern New Territories, the HA planned and
built the North District Hospital, which opened in
1998. There were numerous other additional blocks,
extensions, and improvement projects for existing
hospitals. Investment in major equipment included
the first magnetic resonance imaging machine in the
public system installed at Queen Elizabeth Hospital,
and additional computerised tomography scanners
in major hospitals, etc.
Information technology
There were hardly any major IT systems in use
in public hospitals before the HA, save for very
basic ones for payroll and accounting. There was
massive investment to revamp these systems and
to build many other essential systems for patient
registration and appointments, billing and revenue
collection, medical records tracing, pharmaceutical
management, laboratory results reporting, inventory
management, medical equipment management and
so on. This original weakness turned out to be a
blessing, as it largely obviated the pain of needing to
integrate multiple legacy IT systems from different
provider organisations, as often encountered
overseas when trying to unify data definitions and
functionalities, etc. for territory-wide connectivity.
The HA also chose to mostly build rather than
buy IT systems to maximally fit its own needs and
circumstances.
Eventually, the HA embarked on a most
comprehensive Clinical Management System to
support the work of clinicians and enhance service quality and patient safety. The system became
internationally acclaimed in the field of medical
informatics, and indeed pride of the organisation.
It was clinician-driven from the start, tailored to
the clinical workflow, and incorporated advanced
features to help doctors and nurses in decision
making such as drug allergy and dosage alerts,
knowledge support for evidence-based medicine,
and so on.17
Patient and community relations
The HA launched the Patients’ Charter that explicitly
listed patients’ rights and responsibilities, with
extensive staff communication to change the former
‘we (doctor/nurse) know best’ attitude. Patient
feedback on service quality and staff performance
was systematically collected. Full-time Patient
Relations Officers were employed in hospitals to deal
with complaints and suggestions. Patient Resource
Centres were set up in hospitals, while an HA
InfoWorld was eventually established in the new HA
Building to provide a health promotion and patient
education platform for the public.
As mentioned above, the Public Complaints
Committee incorporating members of the
community provided an independent platform
for appeals. Partnership with the community was
enshrined through the appointment of external
members, including patient advocacy organisations,
to different levels of governance, a far cry from the
closed system of the past.
Financing the reform
After adjusting for the resources required to uplift the
terms of employment of Schedule 2 hospitals’ staff to
be comparable to that of Schedule 1 hospitals, the
baseline recurrent budget of the HA for maintaining
the same level, scope and volume of services at the
beginning of financial year 1992/93 was agreed
to be HK$10 301 million.18 There were additional
upfront allocations that represented a true increase
in investment in the HA to kick-start the reform,
including HK$198 million for new projects,19 HK$98
million for new management initiatives,20 HK$90
million for capital projects, and HK$70 million for
IT projects.18
Quantifiable results
Significant improvements in system capacity and
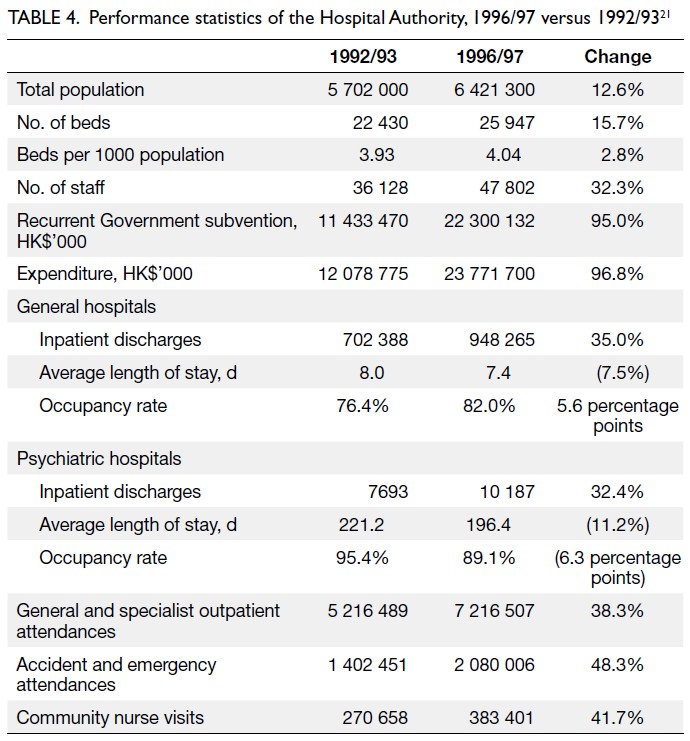
efficiency in the HA, underpinned by substantial
Government investment, can be seen in Table 4 which compares the full-year effect after the HA’s
takeover of management with that 5 years later.21
A number of observations can be made:
- The number of hospital beds increased more than population growth (15.7% vs 12.6%), improving the number of beds per 1000 population.
- Growth in inpatient discharges (35.0% general and 32.4% psychiatric) greatly exceeded growth in total bed numbers (15.7%), indicating more active patient management, as also reflected by shortened average lengths of stay for both general (by 7.5%) and psychiatric (by 11.2%) hospitals.
- The overall occupancy rate improved for general hospitals (from 76.4% to 82.0%), following better utilisation of beds in Schedule 2 hospitals and convalescent hospitals.
- Severe overcrowding in psychiatric hospitals was reduced (from 95.4% to 89.1% occupancy).
- An increase in staff productivity is evidenced by the increase in activities (35.0% for general inpatients, 32.4% for psychiatric inpatients, 38.3% for out-patients, 48.3% for accident and emergency attendances, and 41.7% for community nurse visits) exceeding the increase in staff numbers (32.3%). This does not yet reflect the immense improvements in service quality.
- Taking inflation into account,22 the increase in Government funding to the HA (real growth around 57.8%) and growth in expenditure (real growth around 59.2%) exceeded the increase in staff numbers and activities. As staff costs constituted more than 75% of total expenditure, this mainly reflected the creation of senior posts and general improvement in remuneration.
Analysis
The HA reform represented a bold social experiment
of unprecedented scale in Hong Kong’s history,
given that the HA became the second largest
employer, after the Civil Service, upon its takeover
of all Government and subvented hospitals in
one go. The direction of reform followed the then
prevalent international trend of new managerialism
and corporatisation to free the entity from rigidities
and confines of the Civil Service, and went much
further than the earlier Housing Authority reform.23
It coincided with a period of economic prosperity
during which the Government could afford investing
heavily in upgrading staff terms, funding new
management initiatives, hospital infrastructure,
computerisation, service improvements, and staff
training and development.
While Part 1 of this series describes the success
story of setting up the new HA,1 the management
takeover was when ‘the rubber hits the road’ that
could make or break any well-intentioned reform. Led
by a visionary Board with high-calibre experts from
various fields, the Authority took a pragmatic path
by selecting leaders for major executive positions
from among influential clinicians within the system
with a track record of being reformists who were
passionate to change the dysfunctional system of the
past.24 The atmosphere was nothing short of a brave
new world where the energy of doctors, nurses, allied
health staff and administrators was unleashed to
learn modern management concepts and methods,
and apply them to better the service. This was,
needless to say, highly appreciated by the public, to
the extent that the private sector felt threatened by
a loss of competitiveness in attracting both patients
and talented staff.25
While immense success was justified to
describe this early period, new issues also emerged.
The abolition of the previous Regional Offices
level and the emphasis on individual hospital’s
autonomy aimed to free up local initiatives and
promote internal competition to improve quality
and efficiency. However, this also led to reduced
cooperation and, arguably, an over-proliferation
of management positions (even small hospitals
were supposed to have their own HCEs and a full
complement of managers). This also meant that the
CE had dozens of direct reports, including HCEs
and Head Office deputies. As the system evolved, the
concept of hospital clustering became increasingly
emphasised to streamline management, initially by
function and eventually through formal structure.
At the hospital level, it remains uncertain to what
extent the inverted pyramid model and participative
management was fully embraced, depending on
the style and preferences of the rather autonomous
HCEs. Nevertheless, these were merely minor
issues for any major reforms of this complexity, and paled in significance compared to the overall
achievement.
As in all such reforms involving tens of
thousands of staff, managing the transition was
critical. From a historical perspective, the bridging-over
arrangement and the new HA terms represented
a major victory for staff coupled with the clever
design plus political clout of the then HA Board in
obtaining extra resources. Such a generous offer had
apparently not been repeated since for any other
corporatisation exercise of Government functions.
On the other hand, the retained linkage to the
Civil Service pay scales and salary point systems also
imposed limitation in flexibility when responding to
changing circumstances. When the economy turned
south and particularly after the Asian Economic
Crisis in 1998 when the HA faced budget cuts from
the Government, continued hiring on the original
terms to cope with the ever-increasing service
demand became increasingly untenable. The HA had
no choice but to repeatedly create new ranks with
less favourable packages, to circumvent the rank-to-rank
comparability with the Civil Service, much to
the dismay of new hires. The old culture of the ‘iron
rice bowl’ expecting job stability and annual salary
increments also persisted.
Be that as it may, the experience of turning
such a comprehensive reform blueprint into reality
with success for such an enormous public system,
rendered the HA internationally famous, especially
in the healthcare management circles. This was
achieved not by simply copying other models, but
by integrating best practices from multiple fields
and adapting them to the local situation to address
Hong Kong’s unique circumstances. An important
factor worth mentioning was the cross-disciplinary
learning that happened during that period. There
were intense interactions among Board members,
each with distinct expertise in their own fields,
with the senior executives. Conversely, Board
members also came to better understand the public
healthcare system and its contextual issues. Among
the senior executives, there were also vibrant mutual
learning between those with clinical and non-clinical
disciplines (in management, finance, IT, legal,
engineering, etc.) which provided synergistic results.26
Epilogue
Once the newborn organisation was firmly on its feet
with a new set of management structure, processes
and systems in place, a new phase of reform outgrew
the original blueprint. As the appointed senior
executives including the CE were predominantly
clinician-managers, the subsequent trajectory was
heavily influenced by the clinical and public health
perspectives, rather than simply system efficiency
and customer-focus concerns. The next article (Part
3) describes the emergent philosophy and practice of deepening reform within the HA in the subsequent years.
Acknowledgement
The author would like to thank the Hospital Authority for
permission to use the historical photo of its founding members
in this article, as scanned from its Annual Report 1990-1991.
Declaration
The author declares full responsibility for the accuracy of the
content, which does not represent the views of the Hospital
Authority. Given the scale of the reform, not all aspects can
be covered in detail. Interested readers and scholars are
encouraged to consult the Hospital Authority’s publications
for further information.
Notes
1. Ho W. The Hong Kong Hospital Authority reform: a historical perspective. Part 1: From pre–Hospital Authority era to establishment of the Hospital Authority. Hong Kong Med J 2025;31:508-14.
2. Coopers & Lybrand WD Scott. The Delivery of Medical Services in Hospitals—A Report for the Hong Kong Government. Hong Kong: Hong Kong Government Printer; December 1985.
3. Chung SY. Provisional Hospital Authority Report. Hong Kong: Hong Kong Government Printer; December 1989.
4. Also refer Chung SY, The Hospital Authority of Hong Kong–Part I: From Inception to Reality and its Initial Success. The Medical and Dental Directory of Hong Kong, fifth edition, 1994.
5. Hospital Authority, Hospital Authority Annual Report 1990-1991, pp 5-6. This version of the mission statement was in use until 2009, when the HA Board considerably simplified it.
6. Hospital Authority. Hospital Authority Annual Report 1990-1991, Appendix 2.
7. This is quite different from the picture in the UK, United States or Australia where hospital chiefs are more often non-doctors.
8. Except for radiology and radiotherapy departments where the Department Manager (DM) would be a senior radiographer; pathology departments where the DM would be a senior laboratory technologist; and allied health departments where the DM would be from their own discipline.
9. This puts patient care at the clinical frontline into centre stage at the ‘top’, while the ‘top management team’ should assume a more supportive rather than directive function at the ‘bottom’.
10. The Scott Report proposed the equalisation of staff terms by aiming at a level between that of Schedule 1 and Schedule 2 hospitals, which was vehemently opposed by those working in the former. From the start, therefore, the new HA package was designed to benchmark that of the Civil Servants, which meant an up-front recurrent investment to bring up those working in Schedule 2 hospitals.
11. While all staff of a particular pay band in the Civil Service may be entitled to a host of benefits, not all of them were enjoying all benefits at the same time (eg, government quarters depending on availability), hence the snapshot approach for computing comparable cost.
12. While not explicitly stated, it was implied that retention of the basic salary scales also meant retention of the yearly salary increment practice. In addition, the annual salary adjustments in line with inflation also followed that of the Civil Service.
13. Linking of the Cash Allowance as a percentage of basic salary was under the assumption that in time, the Government would also increase benefits for Civil Servants together with salary increase. However, it turned out that Government was cutting back Civil Service housing benefits a few years down the road. Following a report of the Director of Audit in 1994 that alleged breaching of the comparability principle, the Cash Allowance for new hires was delinked from basic salary.
14. As it played out, the HA Provident Fund Scheme was among the best-performing retirement funds in Hong Kong, both in terms of its administration and investment returns, thanks to the expertise in the Trust Board as well as professionals employed to manage the scheme.
15. With time, the interest portion of mortgages would decrease as will the Home Loan Interest Subsidy Scheme subsidy amount, but the staff member would generally have had pay rise or even promotion, hence could better afford the mortgage. It also meant regenerating available fund to the Scheme to support new applications.
16. Staff unions successfully negotiated using the last drawn salary point as Civil Servant (value updated to the date of retirement from HA) for calculation in the Frozen Pension arrangement. Another option was the Mixed Service Pension arrangement where the staff would retain full pension eligibility for total years served including as HA staff, but receive a reduced Cash Allowance and would not be eligible for the HA Provident Fund. There was also negotiation on the accumulated leave days, resulting in agreement that each staff member was allowed to carry over a maximum of 30 days of ‘sinking leave’.
17. In contrast, many overseas systems are fragmented across hospitals and often structured on the business/financial side while weak on clinical side. The Clinical Management System eventually evolved to become the territory-wide Electronic Health Record (eHR) system that spans the private sector as well.
18. Hospital Authority, Hospital Authority Annual Report 1992-93, p 18. Since HA only took over operation on 1 December 1991, the budget for 1992/93 was the first full-year budget.
19. This amount was for commissioning and opening of new beds and facilities, which would have to be spent with or without the HA’s establishment.
20. Mainly the salaries of all new management positions in the Head Office and hospitals.
21. Hospital Authority. Hospital Authority Annual Reports 1992/93 and 1996/97, Appendices.
22. Inflation figures in Hong Kong were 8.8% (1993), 8.7% (1994), 9.1% (1995) and 6.3% (1996). International Financial Statistics database, International Monetary Fund. Available from: https://data.worldbank.org/indicator/FP.CPI.TOTL.ZG?locations=HK. Accessed 29 Dec 2025. This gives a cumulative inflation of around 37.2% for the period.
23. The Housing Department, which is the executive arm of the Hong Kong Housing Authority, remained within the Civil Service.
24. The first two CEs of HA, Dr EK Yeoh and the author, were active members of the former Government Doctors’ Association, as were Deputy Directors Dr WM Ko 高永文 and Dr Hong Fung 馮康. It is noteworthy that Dr Yeoh, Dr York Chow 周一嶽 (one among the first batch of HCEs) and Dr Ko later became the three successive policy secretaries in the Government (Secretary for Health and Welfare/Secretary for Food and Health) spanning the period 1999 to 2017.
25. The private hospitals began to get their acts together and formed the Hong Kong Private Hospitals Association (HKPHA) in 2000, as well as introduced the UK-based Trent Accreditation system in an effort to improve their own management and quality of service. The author became Chairman of HKPHA in 2018 and thus conversant with its history.
26. Such cross-disciplinary learning seemed to have lost momentum in recent times, as fewer clinicians promoted to management positions pursue formal management courses, while non-clinician executives entirely home-grown within the system may not be able to bring in fresh perspectives and expertise as in the formative years.