Hong Kong Med J 2026;32:Epub 2 Feb 2026
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Utilisation trends and early outcomes of robotic
arm–assisted total hip arthroplasty in a tertiary
joint replacement centre in Hong Kong
KL Fong1; Amy Cheung, FHKAM (Orthopaedic Surgery), FHKCOS2; Michelle Hilda Luk, FHKAM (Orthopaedic Surgery), FHKCOS2; Thomas KC Leung, FHKAM (Orthopaedic Surgery), FHKCOS2; Lawrence CM Lau, FHKAM (Orthopaedic Surgery), FHKCOS2; PK Chan, FHKAM (Orthopaedic Surgery), FHKCOS1; KY Chiu, FHKAM (Orthopaedic Surgery), FHKCOS1; Henry Fu, FHKAM (Orthopaedic Surgery), FHKCOS1
1 Department of Orthopaedics and Traumatology, The University of Hong Kong, Hong Kong SAR, China
2 Department of Orthopaedics and Traumatology, Queen Mary Hospital, Hong Kong SAR, China
Corresponding author: Prof H Fu (drhfu@ortho.hku.hk)
Abstract
Introduction: This study evaluated utilisation
trends and early outcomes of robotic arm–assisted
primary total hip arthroplasty (rTHA) compared
with conventional THA (cTHA) in Hong Kong.
Methods: This retrospective cohort study included
all patients who underwent primary THA in public
hospitals under the Hong Kong West Cluster
(HKWC) from 2019 to 2024. Data were retrieved
from the Hospital Authority’s electronic databases.
The primary outcome was the percentage utilisation
of rTHA relative to cTHA. Secondary outcomes
included operating time (skin-to-skin), length of
stay (LOS), 30- and 90-day reoperation rates, and
30- and 90-day emergency department attendance.
Differences in these outcomes between rTHA and
cTHA were examined.
Results: In total, there were 311 and 242 cases of
rTHA and cTHA, respectively. Robotic utilisation
increased from 32.0% in 2019 to 62.2% in 2024.
Regarding patient outcomes, rTHA increased
operating time by 14.59 minutes (142.02 ± 53.88 vs
127.43 ± 53.34; P=0.002). There was no significant
difference in median LOS between the two groups.
Robotic surgery was also associated with a lower
30-day reoperation rate (0.32% vs 2.07%; P=0.049).
One reoperation due to dislocation was performed in the rTHA group. In the cTHA group, one
dislocation, two periprosthetic fractures, and two
infections required revision surgery.
Conclusion: Given the increasing use of rTHA in
the HKWC, the present findings suggest that rTHA
is associated with a lower 30-day reoperation rate.
As the first local study on early outcomes of rTHA,
these results may serve as reference data for other
centres.
New knowledge added by this study
- Utilisation of robotic arm–assisted primary total hip arthroplasty (rTHA) nearly doubled between 2019 and 2024.
- Robotic arm–assisted primary total hip arthroplasty was associated with a lower 30-day reoperation rate.
- Early results suggested that rTHA was associated with fewer postoperative complications requiring reoperation.
- Long-term data are needed to further evaluate trends in operating time and length of stay, and to determine how these outcomes translate into improved functional outcomes.
Introduction
In Hong Kong, robotic surgery has gained popularity
across various specialties, with the Da Vinci robot
becoming the standard of care in urology and seeing
widespread use in general surgery.1 Orthopaedic
robotic systems are often semi-active and partially
controlled by the surgeon.2 In total hip replacement,
an image-based, semi-active, haptic-constrained
robotic arm system is commonly used. The Mako Robotic Arm Assisted Surgical System (Stryker Corp,
Fort Lauderdale [FL], US) is a surgical system for total
hip replacement approved by the US Food and Drug
Administration.3 Surgical planning is performed
using three-dimensional computed tomography
scans, enabling accurate, patient-specific planning.
Bone removal is performed under haptic control
by the robotic arm, with component implantation
angles also guided by the robot, enhancing precision and accuracy.4 5 Western literature has shown that
robotic arm–assisted primary total hip arthroplasty
(rTHA) yields better radiological and clinical
outcomes.6 7 8 However, local data on the early clinical
outcomes of robotic total hip replacement remain
limited. Robotics was first introduced locally by
the Hong Kong West Cluster (HKWC) in 2019, and
its use has been increasing. Our cluster has since
accumulated substantial experience and moved
beyond the learning curve. This study aimed to
evaluate utilisation trends and patient outcomes of
rTHA compared with conventional THA (cTHA).
Methods
Objective
The primary outcome was the percentage utilisation
of rTHA relative to cTHA in the HKWC from 2019
to 2024. Secondary outcomes included operating
time (skin-to-skin), length of stay (LOS), 30-day
and 90-day reoperation, and 30-day and 90-day
emergency department attendance. Length of stay
was defined as the duration of inpatient admission
following THA. Discharge criteria included the
ability to ambulate with a walking aid and the absence
of impending medical conditions. Reoperation was
defined as undergoing another hip procedure, such
as revision or implant removal, within 30 or 90
days of surgery. Emergency department attendance was defined as presentation to the accident and
emergency department within 30 or 90 days
following discharge.
Additionally, postoperative complication
rates were examined in terms of reoperation,
emergency department attendance, and the
corresponding diagnoses. Complications of interest
included dislocation, periprosthetic fracture, and
periprosthetic joint infection. The study adhered
to the STROBE (Strengthening the Reporting of
Observational Studies in Epidemiology) guideline.
Surgical technique
Total hip arthroplasty in both groups was performed
via a posterior approach with the patient in the left
lateral decubitus position. All patients received
a cementless, proximally coated femoral stem
(Accolade II; Stryker Corp, Mahwah [NJ], US) and a
porous acetabular shell (Trident Acetabular System;
Stryker Corp, Mahwah [NJ], US).3
In the cTHA group, the femoral osteotomy site
was marked based on a predetermined distance from
the lesser and greater trochanters. The acetabulum
was reamed freehand, down to the true floor and
healthy bleeding bone. Cup impaction was guided
by an alignment guide and intraoperative landmarks,
including the transverse acetabular ligament and the
anterior and posterior acetabular walls, to determine
the orientation of the acetabular component.9 10
All rTHAs were performed using the Mako
Robotic Arm Assisted Surgical System, which guided
acetabular reaming and component placement
within haptically confined boundaries. A trial cup
was inserted at the appropriate abduction angle,
with anteversion guided by the robotic arm.10
Study design and patient selection
This was a retrospective cohort study. Data were
retrieved from the Clinical Data Analysis and
Reporting System (CDARS) and the Clinical
Management System (CMS). The CDARS is a
database containing medical information for
research purposes, whereas the CMS is primarily
used for day-to-day clinical management. The
function to distinguish between rTHA and cTHA
was introduced in CDARS in 2021. Therefore, data
from 1 January 2021 to 31 December 2024 were
collected via CDARS, while data from 2019 to 2020
were obtained through CMS chart review. Both
systems follow standardised data protocols and can
be used concurrently.
All patients who underwent primary unilateral
rTHA or cTHA in the HKWC were included.
Diagnoses included osteoarthritis, avascular
necrosis, aseptic necrosis, developmental dysplasia
of the hip, dislocation, and fractures. Patients with
diagnoses of bone malignancy, chronic osteomyelitis,
or complex primary THA—such as Crowe type III/IV hip dysplasia or post-traumatic osteoarthritis with retained hardware—were excluded. Patients
who had staged bilateral procedures were included
as separate cases. During the initial learning phase
in 2019, all surgeries were performed by a single
surgeon (corresponding author). From 2020 onwards, other surgeons
within the division began performing rTHA.
Statistical analysis
All analyses were conducted using SPSS (Windows
version 29.0; IBM Corp, Armonk [NY], US). A two-tailed
significance threshold was set at P<0.05. The
normality of continuous variables was assessed
using skewness and kurtosis, as well as the Shapiro–Wilk and Kolmogorov–Smirnov tests. Normally
distributed continuous variables, such as operating
time, were compared using independent samples
t tests. The non–parametric continuous variable,
LOS, was analysed using the Mann-Whitney U test.
Categorical data were compared via the Chi squared
test.
Results
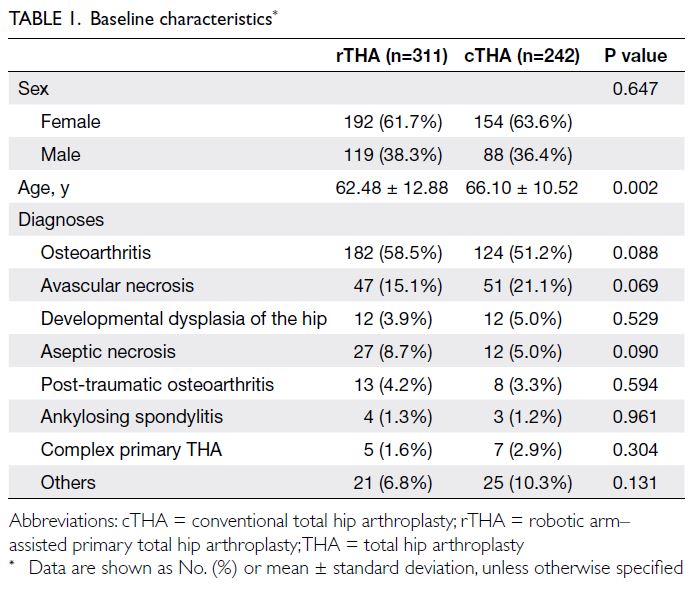
From 2019 to 2024, a total of 311 and 242 THAs
were performed in the rTHA and cTHA groups,
respectively. Patient demographics are summarised
in Table 1. In terms of sex distribution, 61.7% of
patients in the rTHA group and 63.6% of those in
the cTHA group were women. Patients undergoing
rTHA had a lower mean age at the time of surgery
compared with those receiving cTHA (62.48 ± 12.88 vs 66.10 ± 10.52 years; P=0.002). There was
a tendency for rTHA to be performed in younger
patients, although the distribution of diagnostic
categories was similar between groups.
Osteoarthritis was the most common diagnosis
in both groups, accounting for 58.5% of rTHA cases
and 51.2% of cTHA cases. The second most common
diagnosis was avascular necrosis, representing 15.1%
of rTHA cases and 21.1% of cTHA cases (Table 1).
Utilisation trends
The primary outcome was the utilisation rate
of rTHA in the HKWC. As shown in Table 2, a
steady increase in robotic cases was observed,
from 32.0% in 2019 to 62.2% in 2024. Notably, the
highest proportion was recorded in 2023, at 75.2%.
In contrast, the proportion of conventional cases
steadily declined, almost halving from 68.0% in 2019
to 37.8% in 2024. The substantial increase in rTHA
proportion illustrates a clear shift from cTHA to
rTHA as the predominant surgical approach over
the study period.
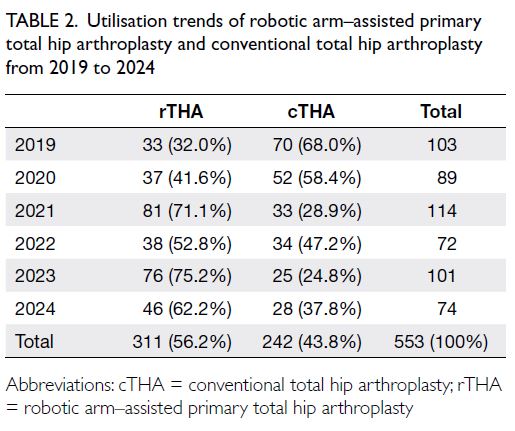
Table 2. Utilisation trends of robotic arm–assisted primary total hip arthroplasty and conventional total hip arthroplasty from 2019 to 2024
Operating time (skin-to-skin)
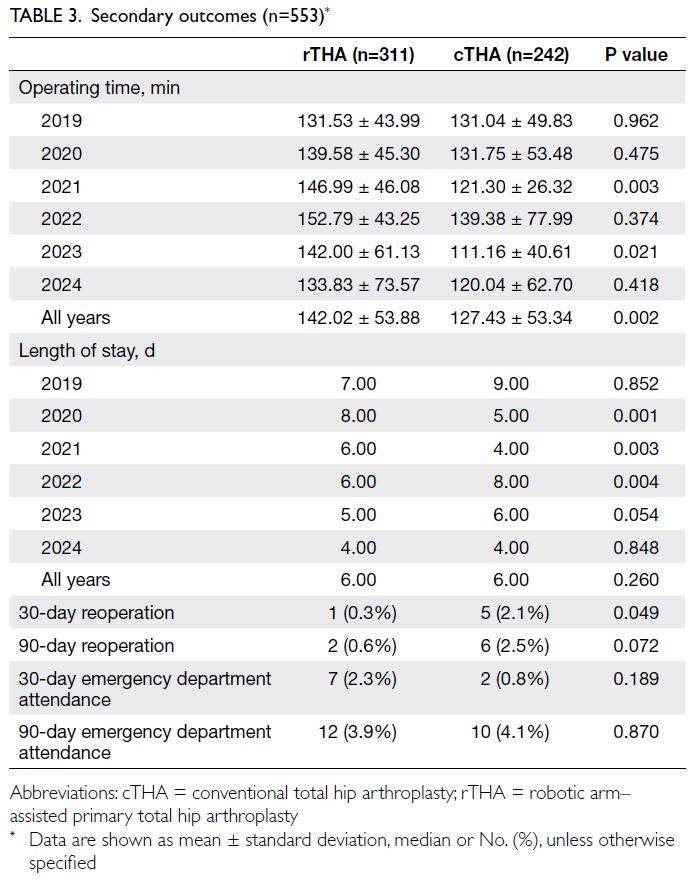
The secondary outcomes are presented in Table 3.
Robotic arm–assisted primary total hip arthroplasty had a mean operating time of 142.02 minutes, which was 14.59 minutes longer than that
of cTHA (127.43 minutes). For rTHA, the mean
operating time was 131.53 minutes in 2019, increased
to 139.58 minutes in 2020 with more surgeons
beginning their learning curve, and then reached a
plateau over the next 2 years (2021: 146.99 minutes;
2022: 152.79 minutes). In the final 2 years of the
study, operating time decreased to 142.00 minutes in
2023 and 133.83 minutes in 2024, reflecting passing
of learning curve by the whole surgical team. In
contrast, cTHA operating times ranged from 111
to 139 minutes, without a clear trend. In the first
2 years, operating times were similar (2019: 131.04
minutes; 2020: 131.75 minutes), followed by a slight
increase to 139.38 minutes in 2022, then dropped to
111.16 minutes in 2023, with a moderate increase to
120.04 minutes in 2024.
Length of stay
Discharge criteria remained consistent throughout
the study period and included the ability to ambulate
independently with a walking aid, effective pain
control, absence of immediate wound complications,
and no major medical issues. Most patients were
discharged directly under the enhanced recovery
after surgery protocol; only those undergoing
complex primary THA (<10% of the cohort) were
transferred to rehabilitation hospitals. The median
LOS was the same in both groups (6.00 vs 6.00 days;
P=0.260) [Table 3]. When rTHA was first introduced
in 2019, all procedures were performed by a single
surgeon, which may have influenced early outcomes.
In 2020 and 2021, more surgeons began performing
rTHA, which may partly explain the longer LOS
observed during this learning-curve period.
Reoperation and emergency department
attendance
Robotic arm–assisted primary total hip arthroplasty
was associated with a lower 30-day reoperation rate compared with cTHA (0.32% vs 2.07%; P=0.049).
Similarly, a trend towards a lower 90-day reoperation
rate was observed for rTHA (0.64% vs 2.48%;
P=0.072) [Table 3].
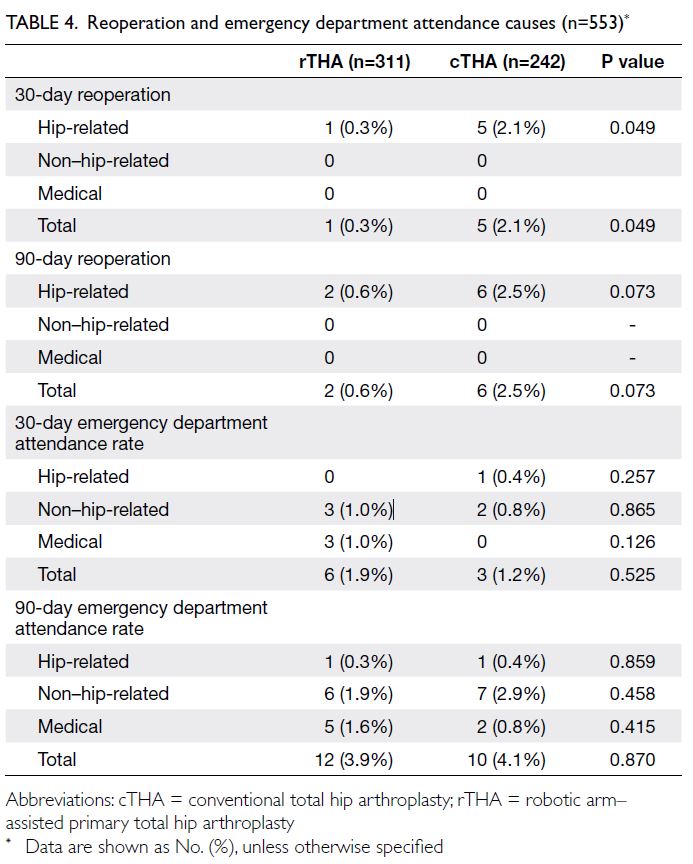
All 30-day reoperations were hip-related. As
shown in Table 4, one reoperation was performed
in the rTHA group and five in the cTHA group.
In the rTHA group, reoperation was required for
a hip dislocation, which was managed by closed
reduction. In the cTHA group, two periprosthetic
fractures of the proximal femur were treated with
open reduction and internal fixation. Two additional
reoperations were performed for wound infections,
and one hip dislocation was managed by closed
reduction.
All 90-day reoperations were also hip-related.
In the rTHA group, one additional case of dislocation
was noted. In the cTHA group, one new case of
periprosthetic fracture was identified (Table 4).
Discussion
The number of THAs utilising robotic assistance
increased over the study period. The proportion of
robotic cases relative to cTHA also rose, with rTHA
accounting for 56.2% of all THAs when all years
were combined. These findings indicate a shift in the
primary surgical approach within the HKWC from
conventional to robotic techniques. At present, four
public hospitals in Hong Kong have acquired robotic
systems, with several additional systems available on
loan. Brinkman et al11 reported that public interest
in rTHA substantially increased between 2011
and 2020. Compared with online search volumes
for conventional arthroplasty, this growth was
statistically significant.
Clement et al12 reported that, despite the higher
costs associated with robotics, rTHA was a cost-effective
intervention compared with cTHA owing
to greater gains in health-related quality of life, as
measured by the EuroQol 5-Dimension. In addition,
the rising popularity of rTHA may be attributed to
its favourable clinical, functional, and radiological
outcomes, which are discussed further below.
Robotic THA was associated with an increase
in operating time of approximately 15 minutes, which
is slightly less than the 20-minute increase reported
by Han et al (20.72 minutes; P=0.002).13 This
difference may be attributable to the need for system
registration or placement of positioning pins, as well
as the effects of the learning curve. When rTHA
was first introduced in Hong Kong in 2019, only
one experienced surgeon was using the procedure,
with an average operating time of 131 minutes. As
more surgeons began using the robotic system, a
learning-curve effect was suggested by an increase
in operating time over the next 3 years (139.6, 147.0,
and 152.8 minutes, respectively). Notably, robotic
operating time then decreased by 11 minutes from 2022 to 2023, and by a further 8 minutes to 133.83
minutes, suggesting increased familiarity with the
system and the possible completion of the learning
curve. Kayani et al14 similarly reported that robot-assisted
acetabular cup positioning during THA was
associated with a learning curve of 12 cases.
There were no statistically significant
differences in LOS between the rTHA and cTHA
groups; both had a median LOS of 6.00 days. In a
retrospective study, Remily et al15 matched patients
in a 1:1 ratio between robotic and conventional
groups (4630 patients per group) and reported
a significantly shorter mean LOS in the rTHA
group (3.4 vs 3.7 days; P=0.001). These findings
may reflect the ability of robotic technology to
execute preoperative plans tailored to each patient’s
unique anatomy. The results may also be related to
reduced iatrogenic trauma and faster postoperative
rehabilitation. Similarly, Heng et al16 found that the
mean LOS in the robotic group was approximately
1 day shorter. Nevertheless, differences in data
distribution and reporting methods should be noted.
While previous authors reported mean LOS, we
reported the median LOS due to the non-parametric
distribution of our data.
Social and cultural factors may also influence
LOS. Western patients often have access to more
spacious home environments, whereas patients
in Hong Kong may reside in more confined living
spaces, potentially reducing their willingness or
readiness for early discharge. Furthermore, patients
and their families in Hong Kong often adopt a more
conservative approach to discharge, preferring
extended care under medical supervision and a self-perceived
burden to their family members if they
return home early.17 These factors may contribute to
a prolonged LOS.
It was evident that rTHA was associated
with a lower 30-day reoperation rate, with a trend
towards a lower 90-day reoperation rate. Our
findings are consistent with those of Shaw et al18
who reported significantly lower dislocation rates
with rTHA compared with cTHA (0.6% vs 2.5%;
P<0.046). Notably, all cases of unstable rTHA were
successfully managed conservatively in the absence
of component malposition, whereas 46% of unstable
cTHA cases required revision surgery for recurrent
instability due to malalignment.18 A previous
postoperative analysis in Hong Kong19 showed that
96% of robotically positioned acetabular cups fell
within the Lewinnek safe zone (inclination 30°-50°,
anteversion 5°-25°).
Although rTHA improves the accuracy
of implant positioning and reduces outliers in
acetabular cup placement,20 21 there remains a lack
of data concerning how these improved radiological
outcomes translate into differences in long-term
clinical recovery, functional outcomes, implant survivorship, and complication rates when compared with cTHA.22
Limitations
To our knowledge, this is the first territory-wide
study in Asia comparing cTHA and rTHA. However,
several limitations should be acknowledged. First,
the use of big data analysis through the CDARS
precluded adjustment for certain confounding
factors, such as surgeon- and hospital-related
variables. Second, the dataset was confined to the
HKWC as ethics approval could not be obtained
for multi-cluster or private hospital data. Although
other public-sector clusters are also managed by
the Hospital Authority, caution should be exercised
when comparing our findings to other settings.
Nevertheless, the inclusion of multiple surgeons
reflects real-world clinical practice. Finally,
functional outcomes and patient-reported outcome
measures were not assessed; as such, the impact of
rTHA from the patient’s perspective could not be
evaluated.
Evaluation of longer-term outcomes and
registry data from additional clusters will be essential to develop optimal THA strategies, those that
achieve key technical objectives, enhance patient
outcomes, and reduce complications.
Conclusion
The use of rTHA nearly doubled between 2019
and 2024 and was associated with a lower 30-day
reoperation rate compared with cTHA. However, as
this study focused solely on early patient outcomes,
further research is warranted to determine whether
these findings translate into improved long-term
functional outcomes.
Author contributions
Concept or design: KL Fong, H Fu.
Acquisition of data: KL Fong, H Fu.
Analysis or interpretation of data: KL Fong, H Fu.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: KL Fong, H Fu.
Analysis or interpretation of data: KL Fong, H Fu.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Declaration
The results of this study were presented as an oral presentation
at the 44th Annual Congress of Hong Kong Orthopaedic
Association, Hong Kong, 2-3 November 2024.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was approved by the Institutional Review Board
of The University of Hong Kong/Hospital Authority Hong
Kong West Cluster, Hong Kong (Ref No.: UW 24-128). The
requirement for informed patient consent was waived by the
Board due to the retrospective nature of the study.
References
1. Ng AT, Tam PC. Current status of robot-assisted surgery.
Hong Kong Med J 2014;20:241-50. Crossref
2. Smith A, Picheca L, Mahood Q. Robotic Surgical Systems
for Orthopedics. Ottawa: Canadian Agency for Drugs
and Technologies in Health; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK602663/. Accessed 12
Mar 2025.
3. Stryker. Available from: https://www.stryker.com. Accessed 12 Mar 2025.
4. Inabathula A, Semerdzhiev DI, Srinivasan A, Amirouche F,
Puri L, Piponov H. Robots on the stage: a snapshot of the
American robotic total knee arthroplasty market. JB JS
Open Access 2024;9:e24.00063. Crossref
5. Jahng KH, Kamara E, Hepinstall MS. Haptic robotics in total hip arthroplasty. In: Minim Invasive Surg
Orthopaedics. New York: Springer; 2015: 1-15. Crossref
6. Salášek M, Pavelka T, Rezek J, et al. Mid-term functional
and radiological outcomes after total hip replacement
performed for complications of acetabular fractures. Injury
2023;54:110916. Crossref
7. De Santis V, Bonfiglio N, Basilico M, et al. Clinical and
radiographic outcomes after total hip arthroplasty with the
NANOS neck preserving hip stem: a 10 to 16-year followup
study. BMC Musculoskelet Disord 2022;22(Suppl
2):1061. Crossref
8. Perets I, Walsh JP, Close MR, Mu BH, Yuen LC, Domb BG.
Robot-assisted total hip arthroplasty: clinical outcomes
and complication rate. Int J Med Robot 2018;14:e1912. Crossref
9. Fontalis A, Kayani B, Plastow R, et al. A prospective
randomized controlled trial comparing CT-based planning
with conventional total hip arthroplasty versus robotic
arm-assisted total hip arthroplasty. Bone Joint J 2024;106-B:324-35. Crossref
10. Domb BG, El Bitar YF, Sadik AY, Stake CE, Botser IB.
Comparison of robotic-assisted and conventional
acetabular cup placement in THA: a matched-pair
controlled study. Clin Orthop Relat Res 2014;472:329-36. Crossref
11. Brinkman JC, Christopher ZK, Moore ML, Pollock JR,
Haglin JM, Bingham JS. Patient interest in robotic total
joint arthroplasty is exponential: a 10-year Google trends
analysis. Arthroplast Today 2022;15:13-8. Crossref
12. Clement ND, Gaston P, Hamilton DF, et al. A cost-utility
analysis of robotic arm-assisted total hip arthroplasty:
using robotic data from the private sector and manual
data from the National Health Service. Adv Orthop
2022:2022:5962260. Crossref
13. Han PF, Chen CL, Zhang ZL, et al. Robotics-assisted versus
conventional manual approaches for total hip arthroplasty:
a systematic review and meta-analysis of comparative
studies. Int J Med Robot 2019;15:e1990. Crossref
14. Kayani B, Konan S, Huq SS, Ibrahim MS, Ayuob A, Haddad
FS. The learning curve of robotic-arm assisted acetabular
cup positioning during total hip arthroplasty. Hip Int
2021;31:311-9. Crossref
15. Remily EA, Nabet A, Sax OC, Douglas SJ, Pervaiz SS,
Delanois RE. Impact of robotic assisted surgery on
outcomes in total hip arthroplasty. Arthroplast Today
2021;9:46-9. Crossref
16. Heng YY, Gunaratne R, Ironside C, Taheri A. Conventional
vs robotic arm assisted total hip arthroplasty (THA) surgical
time, transfusion rates, length of stay, complications and
learning curve. J Arthritis 2018;7:1000272. Crossref
17. Bayer-Oglesby L, Zumbrunn A, Bachmann N; SIHOS
Team. Social inequalities, length of hospital stay for
chronic conditions and the mediating role of comorbidity
and discharge destination: a multilevel analysis of hospital
administrative data linked to the population census in
Switzerland. PLoS One 2022;17:e0272265. Crossref
18. Shaw JH, Rahman TM, Wesemann LD, Jiang CZ,
G Lindsay-Rivera K, Davis JJ. Comparison of postoperative
instability and acetabular cup positioning in robotic-assisted
versus traditional total hip arthroplasty. J
Arthroplasty 2022;37(8S):S881-9. Crossref
19. Fu CH, Cheung YL, Cheung MH, et al. Robotic arm-assisted
total hip replacement: early experience in Hong
Kong. In: Proceedings of the 40th Annual Congress of the
Hong Kong Orthopaedic Association; 2020 Oct 31-Nov 1; Hong Kong. Hong Kong: Hong Kong Academy of
Medicine Press; 2020: 71. Available from: https://hub.hku.hk/handle/10722/305989. Accessed 12 Mar 2025.
20. Beverland DE, O’Neill CK, Rutherford M, Molloy D,
Hill JC. Placement of the acetabular component. Bone
Joint J 2016;98-B(1 Suppl A):37-43. Crossref
21. Kayani B, Konan S, Thakrar RR, Huq SS, Haddad FS.
Assuring the long-term total joint arthroplasty: a triad of
variables. Bone Joint J 2019;101-B(1_Supple_A):11-8. Crossref
22. Kayani B, Konan S, Ayuob A, Ayyad S, Haddad FS. The
current role of robotics in total hip arthroplasty. EFORT
Open Rev 2019;4:618-25. Crossref