Hong Kong Med J 2026;32:Epub 30 Jan 2026
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
A ten-year evaluation of the incidence of
obstetric anal sphincter injury with a reduced episiotomy rate
YY Lau, MB, ChB, MRCOG; TW Chau, MB, ChB; WC Tang, MB, BS; Rachel YK Cheung, MD, FHKAM (Obstetrics and Gynaecology); SM Ng, MSc; TM Tso, MSc, BN; Symphorosa SC Chan, MD, FHKAM (Obstetrics and Gynaecology)
Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr YY Lau (yanyanlau@cuhk.edu.hk)
Abstract
Introduction: The role of episiotomy in preventing
obstetric anal sphincter injury (OASIS) remains
controversial. Liberal use of episiotomy has been
reduced locally. This study aimed to review the
incidence of OASIS in our unit over the past decade
given the reduced episiotomy rate.
Methods: A retrospective study was conducted in a
single tertiary obstetrics and gynaecology unit. All
singleton vaginal deliveries, including normal and
instrumental deliveries, between 2012 and 2021
were included. Data were retrieved from the hospital
electronic delivery database between July 2022 and
June 2023. The degree of OASIS was assessed using
the Abdul Sultan classification.
Results: In total, 43 732 deliveries were included.
The episiotomy rate decreased from 62.8% in 2012
to 44.7% in 2021 (P<0.001), while the OASIS rate
increased from 0.3% to 1.4% over the same period
(P<0.001). Among nulliparous women, the OASIS
rate was significantly lower with episiotomy in both
normal vaginal deliveries (0.6% vs 1.7%; P<0.001) and
instrumental deliveries with episiotomy than without
(1.7% vs 42.9%; P<0.001). Among multiparous
women, the OASIS rate was significantly lower in
normal vaginal delivery without episiotomy than with (0.3% vs 0.5%; P=0.026), but significantly lower
in instrumental deliveries with episiotomy than
without (0.5% vs 23.5% P<0.001). Overall, episiotomy
was a protective factor for OASIS (odds ratio=0.273,
95% confidence interval= 0.208-0.358; P<0.001).
Conclusion: Episiotomy was protective against
OASIS among nulliparous women with singleton
normal vaginal delivery and instrumental delivery
in an Asian population. It also conferred protection
among multiparous women undergoing instrumental
delivery but not in those having normal vaginal
delivery.
New knowledge added by this study
- Episiotomy is a protective factor against obstetric anal sphincter injury (OASIS) among nulliparous women undergoing singleton normal vaginal delivery and instrumental delivery in an Asian population.
- Episiotomy also confers protection against OASIS among multiparous women undergoing instrumental delivery in an Asian population.
- Conversely, episiotomy may increase the risk of OASIS in multiparous women undergoing normal vaginal delivery.
- It is recommended that women should be informed of these findings to support informed decision-making regarding episiotomy.
- A more restrictive approach should be adopted in multiparous women undergoing normal vaginal delivery.
Introduction
Obstetric anal sphincter injury (OASIS) is a serious
complication of vaginal delivery that can result in
faecal incontinence, thereby impairing women’s
quality of life. Reported prevalence rates of OASIS
range from less than 1% to 11%.1 2 3 In the United
Kingdom, the incidence tripled from 1.8% to 5.9%
between 2000 and 2012, presumably due to improved detection techniques and increased awareness.4 In
Hong Kong, the incidence increased from 0.04% in
2004 to 0.1% in 2009, and to 0.3% in 2014 during
normal vaginal deliveries.5 Episiotomy, commonly
performed during the second stage of labour to
facilitate delivery and prevent excessive stretching
of the perineal muscles, may increase intrapartum
blood loss and perineal pain.6 The role of episiotomy in mitigating OASIS remains controversial.7 8
Consequently, the liberal use of episiotomy has
declined in Hong Kong, with rates falling from 81%
in 2004 to 66.2% in 2009 and 47.4% in 2014.5 Ethnic
differences in pelvic floor biometry and pelvic organ
mobility have been reported,8 9 and studies suggest
that Asian women are more prone to OASIS.10 11 This
study aimed to review the incidence of OASIS in our
unit over the past decade in the context of declining
episiotomy rates.
Methods
This study was conducted in Prince of Wales
Hospital, a tertiary obstetrics and gynaecology unit
with an annual delivery volume of approximately
4500 to 6000. All singleton vaginal deliveries—including spontaneous vaginal, ventouse, or
forceps deliveries—between 1 January 2012 and 31
December 2021 were included. Breech and preterm
deliveries were excluded. Maternal demographics
were entered into the electronic record either
antenatally by midwives or obstetricians if women
had received antenatal care in our unit, or by
midwives immediately after delivery. Maternal
age and body mass index (BMI) were recorded at
delivery. Macrosomia was defined as a birth weight
of ≥4000 g. Most spontaneous vaginal deliveries
were conducted by trained midwives or student
midwives under supervision; instrumental deliveries
were performed by trained obstetricians or trainees
under senior supervision. When indicated, a left
mediolateral episiotomy and a hands-on approach
to protect the perineum were used by both midwives
and doctors. Per vaginal and per rectal examinations
were performed immediately after delivery. If
OASIS was suspected, assessment was conducted
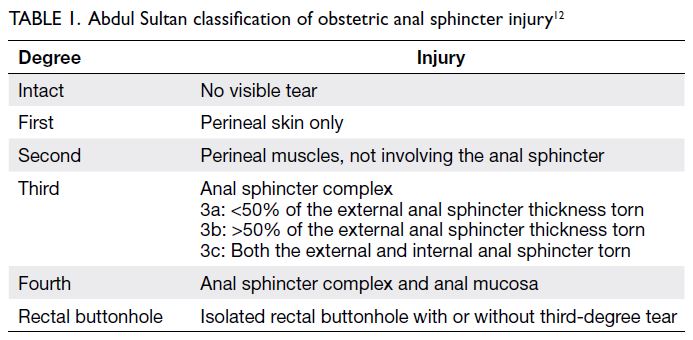
by an obstetric specialist. The degree of OASIS
was classified using the Abdul Sultan classification
(Table 1).12 Delivery details were documented by
midwives immediately after birth. Operative records
for instrumental deliveries and OASIS repair, where
applicable, were completed immediately after the
procedure. Data were extracted from the hospital’s
electronic delivery database between July 2022 and
June 2023. Statistical analyses were performed using
SPSS (Windows version 29.0; IBM Corp, Armonk
[NY], United States). Descriptive analyses were used
to examine demographics, mode of delivery, and the
prevalences of episiotomy and OASIS. Means were
compared between groups using the independent
samples t test. Frequencies were compared using
the Pearson Chi squared test or Fisher’s exact test,
as appropriate. Trends were analysed using the Chi
squared test for trend (Cochran–Armitage test). All
risk factors were included in multivariable logistic
regression analysis except epidural analgesia,
nulliparity, and neonatal birth weight (justification
provided in Results section). A P value of <0.05 was
considered statistically significant.
Results
A total of 43 732 deliveries were included in this
study. The mean ± standard deviation maternal
age at delivery was 31.5 ± 4.7 years and the median
parity was 0 (interquartile range, 1). Of these, 22 566
(51.6%) were nulliparous and 21 166 (48.4%) were
multiparous. Among the latter, 2268 (10.7%) had
only previously delivered by Caesarean section and were therefore vaginally nulliparous. Data
concerning previous delivery mode were missing
for 905 women (4.3%). In total, 39 603 women
(90.6%) had a normal vaginal delivery, 3528 (8.1%)
had ventouse delivery, and 601 (1.4%) had a forceps
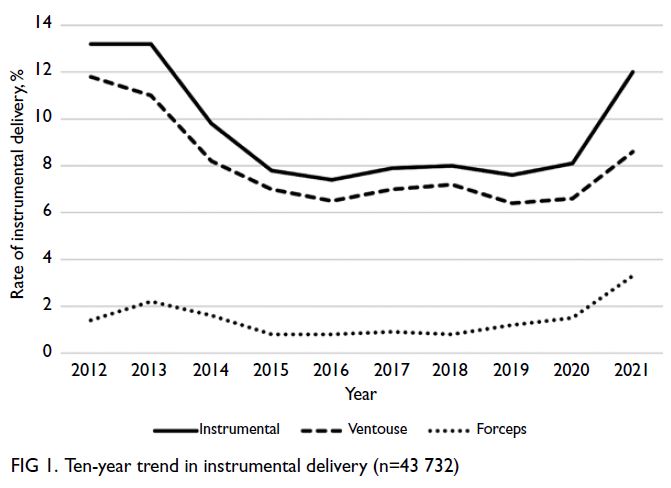
delivery. Over the 10-year period from 2012 to 2021,
the overall instrumental delivery rate and ventouse
delivery rate declined significantly, from 13.2% to
12.0% (P<0.001) and from 11.8% to 8.6%, respectively
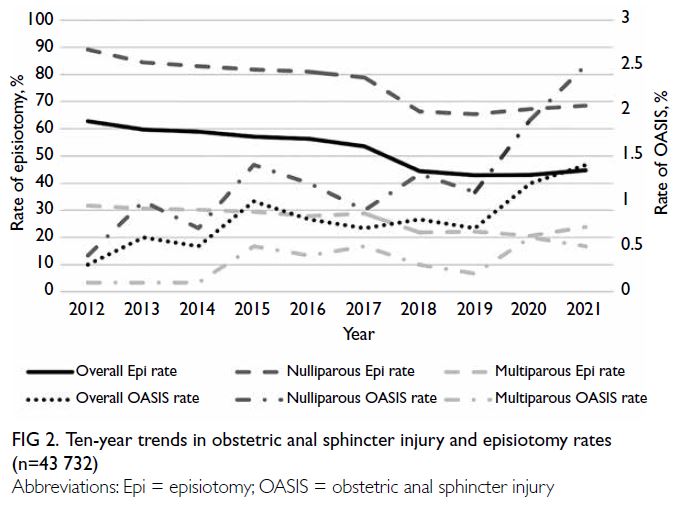
(P<0.001) [Fig 1]. Overall, 23 325 women (53.3%)
underwent episiotomy, whereas 20 407 (46.7%) did
not; 326 women (0.7%) sustained OASIS, whereas
43 406 (99.3%) did not. The overall episiotomy rate
decreased from 62.8% to 44.7% (P<0.001), with
reductions observed in both nulliparous (from 89.2%
to 68.5%; P<0.001) and multiparous women (from
31.7% to 23.8%; P<0.001). Conversely, the overall
OASIS rate increased from 0.3% to 1.4% (P<0.001),
with higher rates in nulliparous (from 0.4% to 2.5%;
P<0.001) and multiparous women (0.1%-0.5%;
P<0.001) [Fig 2].
The characteristics of the study population
are summarised in Table 2. Episiotomy rates among
women with and without OASIS were 51.8% and
53.3%, respectively (P=0.587). A higher proportion
of women in the OASIS group were nulliparous
(79.1% vs 51.4%; P<0.001) and vaginally nulliparous
(85.9% vs 56.5%; P<0.001). Instrumental delivery
was also more common in the OASIS group
compared with the non-OASIS group (29.1% vs
9.3%; P<0.001). No statistically significant difference
was observed between the type of instrumental
vaginal delivery and the occurrence of OASIS
(P=0.128). Women with OASIS had a lower BMI,
a longer duration of labour, and delivered heavier
neonates. No significant differences were observed
in mean maternal age, ethnicity, gestational age,
onset of labour, epidural analgesia, episiotomy, or
macrosomia. All risk factors were included in the
multivariable logistic regression analysis except
epidural analgesia, nulliparity, and neonatal birth
weight. Epidural analgesia was excluded because
only one delivery with OASIS involved epidural
analgesia, while nulliparity and neonatal birth weight
were excluded due to their strong correlation with
vaginal nulliparity and macrosomia, respectively.
Macrosomia was considered to have greater clinical
relevance than neonatal birth weight because a
standard cut-off value exists. Multivariable logistic
regression analysis revealed that vaginal nulliparity
and instrumental delivery remained independent risk
factors for OASIS, whereas BMI and labour duration
did not. Induced labour (odds ratio [OR]=0.734,
95% confidence interval [CI]=0.577-0.934; P=0.012)
and episiotomy (OR=0.273, 95% CI=0.208-0.358;
P<0.001) were identified as protective factors,
while macrosomia (OR=2.754, 95% CI=1.435-5.284;
P<0.001) was identified as a risk factor for OASIS (Table 3). Missing data were noted for BMI in 543 cases (1.2%) and for onset of labour in 82 cases
(0.2%).
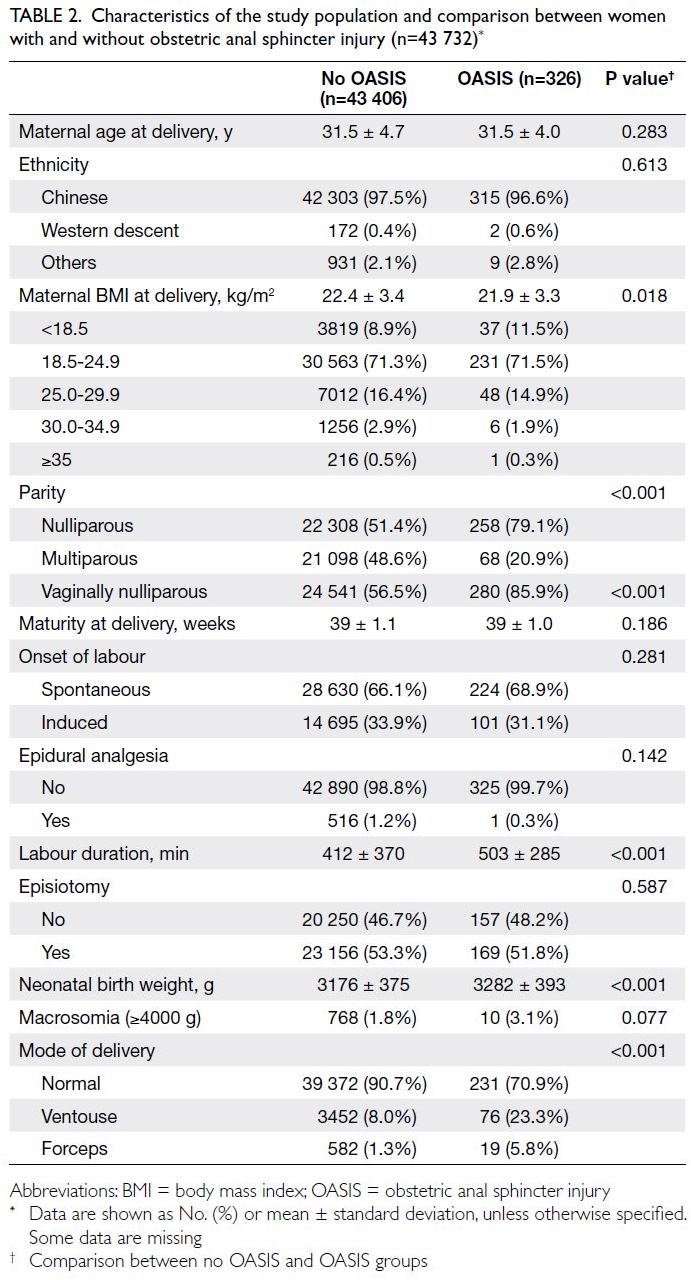
Table 2. Characteristics of the study population and comparison between women with and without obstetric anal sphincter injury (n=43 732)
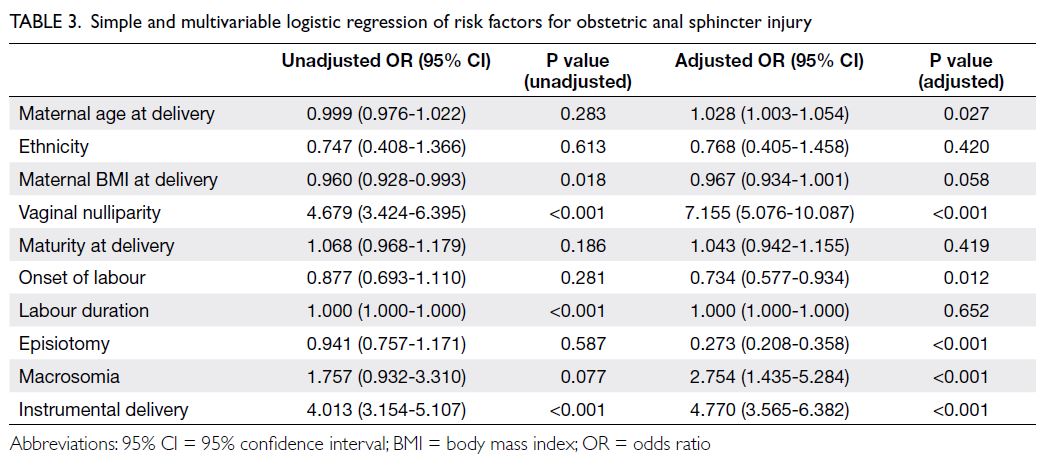
Table 3. Simple and multivariable logistic regression of risk factors for obstetric anal sphincter injury
In the subgroup analysis of nulliparous women,
the OASIS rate was significantly lower among those
undergoing normal vaginal delivery with episiotomy
compared to those without (0.6% vs 1.7%; P<0.001)
and those undergoing instrumental delivery with
episiotomy (1.7% vs 42.9%; P<0.001). Among
multiparous women, the OASIS rate was significantly
lower in those undergoing normal vaginal delivery
without episiotomy (0.3% vs 0.5%; P=0.026) and those
undergoing instrumental delivery with episiotomy (0.5% vs 23.5% without episiotomy; P<0.001). Among
vaginally nulliparous women within the multiparous
group, no statistically significant difference in
OASIS rates was observed between normal vaginal
deliveries with and without episiotomy; however,
the OASIS rate was significantly lower among those
undergoing instrumental deliveries with episiotomy
compared with those without (0% vs 37.5%; P<0.001)
[Table 4].
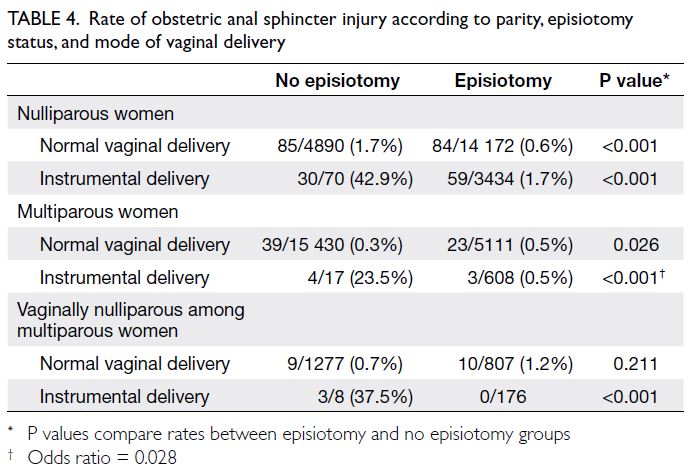
Table 4. Rate of obstetric anal sphincter injury according to parity, episiotomy status, and mode of vaginal delivery
Discussion
In recent years, many obstetric units in Hong
Kong have promoted a reduction in episiotomy
use in recent years. Our unit achieved substantial
reductions in episiotomy rates among nulliparous
and multiparous women between 2012 and 2021.
Although the overall rate of OASIS remained low,
considerable increases were observed in both
groups during the study period. Vaginal nulliparity
and operative vaginal delivery were identified as
independent risk factors for OASIS, consistent with
previous findings.7 11 Furthermore, episiotomy was
identified as a protective factor against OASIS in
multivariable logistic regression analysis (OR=0.273,
95% CI=0.208-0.358) [Table 3].
In nulliparous women, episiotomy was
protective against OASIS in both normal and
instrumental vaginal deliveries. These findings
differ from those of previous large-scale studies.7 11
In a large retrospective study in the Netherlands
involving over 281 000 vaginal deliveries,13 and in
another study including more than 10 000 women
in Australia,14 mediolateral episiotomy was shown to reduce the risk of OASIS in nulliparous women
(OR=0.2113 and 0.54,14 respectively). However,
Mahgoub et al11 in France reported no association
between episiotomy and OASIS. In their cohort of
42 626 women, the overall OASIS rate was 1.2% and
the overall episiotomy rate was only 10%.11 Perrin et al7
reported an episiotomy rate of 63.2% in nulliparous
women and an OASIS rate of 0.7%, regardless of
episiotomy use. In their analysis, episiotomy was not
associated with OASIS in normal vaginal delivery
but appeared to be protective in nulliparous women
undergoing operative vaginal delivery at term.7
The above studies mainly involved women in
Western populations. Several studies have indicated
that Asian women have a two- to nine-fold increased
risk of sustaining OASIS.15 16 17 18 19 In a study conducted
in Israel involving over 80 000 women, including
997 of Asian origin, the OASIS rate among Asian
women was 9 times higher than that among women
of Western descent (3.5% vs 0.4%; P=0.001).16 Asian
women also had a higher proportion of fourth-degree
tears (17.1% vs 6.6%; P=0.039), despite smaller
newborns (mean birth weight: 3318 g vs 3501 g;
P=0.004).16 Anatomical differences between ethnic
groups may contribute to this disparity. Cheung et al9
reported that pregnant women of East Asian origin
had a thicker pubovisceral muscle, a smaller levator
hiatus, and reduced pelvic organ mobility compared
with pregnant women of Western descent. These
factors may contribute to the higher risk of OASIS.9
Moreover, Bates et al20 found that a shorter perineal
length measured during the second stage of labour
prior to pushing was significantly associated with
OASIS. Although a study conducted in Hawaii
found no significant difference in perineal body length between Western and Chinese women,
measurements were taken during the first stage of
labour rather than before pushing.21 Further studies
are needed to determine whether perineal body
length differs during the second stage of labour. The
reasons for the higher OASIS rates among Asian
women remain unclear but are likely to be complex
and multifactorial.
Another notable point is the higher rate of
epidural analgesia use among Western women
compared with Asian women (50%-90% vs 0%-2.2%),
even within the same hospital setting where epidural
analgesia is offered free of charge to all women.7 11 16 20
In the present study, the rate of epidural analgesia
was low throughout the study period. In this cohort,
epidural analgesia was not associated with OASIS.
A meta-analysis examining risk factors for OASIS
found no association with epidural analgesia;
however, it included only two studies.22 In contrast,
Mahgoub et al11 identified epidural analgesia as a
protective factor for OASIS, whereas another meta-analysis
reported it as a risk factor.19 These conflicting
findings suggest that the role of epidural analgesia in
OASIS remains unclear.
There is limited literature on the role of
episiotomy in normal vaginal delivery among
multiparous women. In the present study, episiotomy
did not protect multiparous women from OASIS,
except in the context of instrumental vaginal delivery.
Indeed, episiotomy may increase the risk of OASIS
in this group.23 However, we noted that episiotomy
was protective against OASIS among multiparous
women undergoing instrumental vaginal delivery
(OR=0.028). This finding is supported by a Dutch
study which reported five-fold and ten-fold
reductions in OASIS during vacuum and forceps
deliveries, respectively.24 In light of these findings, we recommend a more restrictive approach to episiotomy among multiparous women undergoing normal vaginal delivery.
The rising trend of OASIS over the past
decade may also be attributable to improvements
in clinical detection following the promotion of
more thorough post-delivery assessments by both
midwives and obstetricians. Kwok et al25 reported
that the prevalence of occult OASIS—detected by
endoanal ultrasound but not identified by clinical
examination after delivery—was as high as 7.8% after
normal vaginal delivery and 3.8% after instrumental
delivery. Subsequently, regular OASIS workshops
were introduced to train midwives and doctors
in performing standardised vaginal and rectal
examinations after vaginal delivery. When a major
perineal tear is suspected, immediate reassessment
by an obstetric specialist is conducted. This practice has been shown to improve the detection rate of
OASIS.26 We also analysed trends in instrumental
vaginal delivery over the 10-year period. Overall,
decreasing trends were observed for both
instrumental and ventouse deliveries. The rate of
forceps delivery remained similar or showed a slight
decrease, except in 2021. Therefore, the rising trend
in OASIS is unlikely to be explained by changes in
instrumental delivery rates.
Strengths and limitations
The strengths of this study include its large sample size,
10-year study period, and the documented reduction
in episiotomy rates, which allowed evaluation of the
role of episiotomy in OASIS. Our unit is a tertiary
centre with the highest delivery volume in Hong
Kong, and this represents the largest retrospective
study to date focusing on an Asian population.
However, as a retrospective study, missing data were
noted during data collection and entry. In addition,
several risk factors previously identified in meta-analyses—such as the duration of the second stage
of labour, fetal head position at delivery, history of
previous OASIS, and shoulder dystocia—were not
analysed in the present study,19 27 representing a key
limitation. Furthermore, some cases of OASIS may
have been missed on clinical examination. High-quality
research is needed to further investigate
OASIS, given its substantial impact on women’s
quality of life.
Conclusion
With a substantial reduction in episiotomy rates,
a corresponding increase in the rate of OASIS
was observed. Episiotomy was protective against
OASIS among nulliparous women undergoing
singleton normal vaginal delivery and instrumental
delivery. It also conferred protection in multiparous
women undergoing instrumental delivery but not
in those having normal vaginal delivery. Among
vaginally nulliparous women within the multiparous
group, the OASIS rate was significantly higher in
those undergoing instrumental deliveries without
episiotomy, similar to the rate observed in nulliparous
women. Conversely, the OASIS rate was higher
in the episiotomy group during normal vaginal
delivery, although this difference was not statistically
significant and may have been influenced by the
small sample size. Further high-quality research
is warranted, and women should be informed of
these findings to enable informed decision-making
regarding episiotomy.
Author contributions
Concept or design: SSC Chan, RYK Cheung.
Acquisition of data: SSC Chan, RYK Cheung, TW Chau, YY Lau, SM Ng, TM Tso.
Analysis or interpretation of data: SSC Chan, YY Lau.
Drafting of the manuscript: YY Lau.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: SSC Chan, RYK Cheung, TW Chau, YY Lau, SM Ng, TM Tso.
Analysis or interpretation of data: SSC Chan, YY Lau.
Drafting of the manuscript: YY Lau.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Ms LL Lee, our research assistant, for her assistance with data acquisition, analysis, and interpretation.
Declaration
Findings from this study were partially presented as an e-poster
at the Royal College of Obstetricians and Gynaecologists
World Congress 2024, Muscat, Oman, 15-17 October 2024.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was obtained from the Joint Chinese University of Hong Kong–New Territories East Cluster Clinical
Research Ethics Committee, Hong Kong (Ref No.: 2022.259).
The requirement for patient consent was waived by the
Committee due to the retrospective nature of the research.
The study complied with the Declaration of Helsinki and the
International Council for Harmonization Guideline for Good
Clinical Practice.
References
1. Tung CW, Cheon WC, Tong WM, Leung HY. Incidence
and risk factors of obstetric anal sphincter injuries after
various modes of vaginal deliveries in Chinese women.
Chin Med J (Engl) 2015;128:2420-5. Crossref
2. Jangö H, Langhoff-Roos J, Rosthøj S, Sakse A. Modifiable
risk factors of obstetric anal sphincter injury in primiparous
women: a population-based cohort study. Am J Obst
Gynecol 2014;210:59.e1-6. Crossref
3. Hsieh WC, Liang CC, Wu D, Chang SD, Chueh HY,
Chao AS. Prevalence and contributing factors of severe
perineal damage following episiotomy-assisted vaginal
delivery. Taiwan J Obstet Gynecol 2014;53:481-5. Crossref
4. Gurol-Urganci I, Cromwell DA, Edozien LC, et al. Third- and
fourth-degree perineal tears among primiparous
women in England between 2000 and 2012: time trends
and risk factors. BJOG 2013;120:1516-25. Crossref
5. Hong Kong College of Obstetricians and Gynaecologists.
Territory-wide Audit in Obstetrics & Gynaecology.
2014. Available from: https://www.hkcog.org.hk/hkcog/Download/Territory-wide_Audit_in_Obstetrics_Gynaecology_2014.pdf. Accessed 1 May 2020.
6. Woolley RJ. Benefits and risks of episiotomy: a review of
the English-language literature since 1980. Part II. Obstet
Gynecol Surv 1995;50:821-35. Crossref
7. Perrin A, Korb D, Morgan R, Sibony O. Effectiveness of episiotomy to prevent OASIS in nulliparous women at
term. Int J Gynaecol Obstet 2023;162:632-8. Crossref
8. Abdool Z, Dietz HP, Lindeque BG. Ethnic differences in
the levator hiatus and pelvic organ descent: a prospective
observational study. Ultrasound Obstet Gynecol
2017;50:242-6. Crossref
9. Cheung RY, Shek KL, Chan SS, Chung TK, Dietz HP.
Pelvic floor muscle biometry and pelvic organ mobility in
East Asian and Caucasian nulliparae. Ultrasound Obstet
Gynecol 2015;45:599-604. Crossref
10. Brown J, Kapurubandara S, Gibbs E, King J. The great
divide: country of birth as a risk factor for obstetric anal
sphincter injuries. Aust N Z J Obstet Gynaecol 2018;58:79-85. Crossref
11. Mahgoub S, Piant H, Gaudineau A, Lefebvre F, Langer B,
Koch A. Risk factors for obstetric anal sphincter injuries
(OASIS) and the role of episiotomy: a retrospective series
of 496 cases. J Gynecol Obstet Hum Reprod 2019;48:657-62. Crossref
12. de Leeuw JW, Struijk PC, Vierhout ME, Wallenburg HC.
Risk factors for third degree perineal ruptures during
delivery. BJOG 2001;108:383-7. Crossref
13. Okeahialam NA, Taithongchai A, Thakar R, Sultan AH.
The incidence of anal incontinence following obstetric anal
sphincter injury graded using the Sultan classification: a
network meta-analysis. Am J Obstet Gynecol 2023;228:675-88.e13. Crossref
14. Hauck YL, Lewis L, Nathan EA, White C, Doherty DA.
Risk factors for severe perineal trauma during vaginal
childbirth: a Western Australian retrospective cohort
study. Women Birth 2015;28:16-20. Crossref
15. Grobman WA, Bailit JL, Rice MM, et al. Racial and ethnic
disparities in maternal morbidity and obstetric care. Obst
Gynecol 2015;125:1460-7. Crossref
16. Baruch Y, Gold R, Eisenberg H, et al. High incidence of
obstetric anal sphincter injuries among immigrant women
of Asian ethnicity. J Clin Med 2023;12:1044. Crossref
17. D’Souza JC, Monga A, Tincello DG. Risk factors for
perineal trauma in the primiparous population during non-operative
vaginal delivery. Int Urogynecol J 2020;31:621-5. Crossref
18. Yeaton-Massey A, Wong L, Sparks TN, et al. Racial/ethnic
variations in perineal length and association with perineal
lacerations: a prospective cohort study. J Matern Fetal
Neonatal Med 2015;28:320-3. Crossref
19. Hu Y, Lu H, Huang Q, et al. Risk factors for severe perineal
lacerations during childbirth: a systematic review and
meta-analysis of cohort studies. J Clin Nurs 2023;32:3248-65. Crossref
20. Bates LJ, Melon J, Turner R, Chan SS, Karantanis E.
Prospective comparison of obstetric anal sphincter injury
incidence between an Asian and Western hospital. Int
Urogynecol J 2019;30:429-37. Crossref
21. Tsai PJ, Oyama IA, Hiraoka M, Minaglia S, Thomas J,
Kaneshiro B. Perineal body length among different racial
groups in the first stage of labor. Female Pelvic Med
Reconstr Surg 2012;18:165-7. Crossref
22. Barba M, Bernasconi DP, Manodoro S, Frigerio M. Risk
factors for obstetric anal sphincter injury recurrence: a
systematic review and meta-analysis. Int J Gynaecol Obstet
2022;158:27-34. Crossref
23. Eggebø TM, Rygh AB, von Brandis P, Skjeldestad FE.
Prevention of obstetric anal sphincter injuries with
perineal support and lateral episiotomy: a historical cohort
study. Acta Obstet Gynecol Scand 2024;103:488-97. Crossref
24. van Bavel J, Hukkelhoven CW, de Vries C, et al. The
effectiveness of mediolateral episiotomy in preventing
obstetric anal sphincter injuries during operative vaginal
delivery: a ten-year analysis of a national registry. Int
Urogynecol J 2018;29:407-13. Crossref
25. Kwok SP, Wan OY, Cheung RY, Lee LL, Chung JP, Chan SS.
Prevalence of obstetric anal sphincter injury following
vaginal delivery in primiparous women: a retrospective
analysis. Hong Kong Med J 2019;25:271-8. Crossref
26. Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal
sphincter injuries—myth or reality? BJOG 2006;113:195-200. Crossref
27. Pergialiotis V, Bellos I, Fanaki M, Vrachnis N,
Doumouchtsis SK. Risk factors for severe perineal trauma
during childbirth: an updated meta-analysis. Eur J Obstet
Gynecol Reprod Biol 2020;247:94-100. Crossref