Hong Kong Med J 2026;32:Epub 29 Jan 2026
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Influenza and Epstein-Barr virus encephalitis in children: could we be missing them and why?
Julian WT Tang, MB, BS, FRCP1,2; KL Hon, MB, BS, MD3
1 Clinical Microbiology, University Hospitals of Leicester NHS Trust, Leicester, United Kingdom
2 Department of Respiratory Sciences, University of Leicester, Leicester, United Kingdom
3 Department of Paediatrics, CUHK Medical Centre, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Prof KL Hon (ehon@cuhk.edu.hk)
We note the case of influenza A encephalopathy
reported in the Hong Kong Medical Journal in 2020,
involving an unvaccinated 10-year-old child who
presented with high fever, convulsions, and altered
consciousness.1 The patient was successfully treated
with anticonvulsants, oseltamivir, and hypertonic
saline and mannitol to control cerebral oedema. The
electroencephalogram showed diffuse slow-wave
activity.1 Although Hong Kong offers a free seasonal
influenza vaccination programme for children aged
6 months to under 12 years (those attending primary
school), uptake remains relatively low (50%-60%),2
and several paediatric influenza-related deaths
are reported annually in the city, primarily among
unvaccinated children.3
A diagnosis of influenza encephalitis is
made after exclusion of all other possible causes,
following confirmed detection of influenza virus in a
respiratory sample, but only very rarely by detection
of influenza RNA in the cerebrospinal fluid (CSF).
Clinical presentation can be variable, including
fever, seizures, meningism, photophobia, excessive
sleepiness, disorientation, agitation, altered
personality, and leg paresis. Electroencephalogram
findings can show diffuse slowing or generalised
spike-wave activity, while magnetic resonance
imaging may be normal or show multiple focal
lesions.4
This form of ‘indirect’ diagnosis in viral
encephalitis is not unique to influenza. Among other
viral encephalitis—such as West Nile virus, Japanese
encephalitis virus, and tick-borne encephalitis
viruses—diagnosis is often confirmed by serology or
seroconversion as the virus may have already cleared
from the CSF by the time patients with neurological
symptoms present. Concerning influenza
encephalitis, virus detection in a respiratory
sample by polymerase chain reaction is a common
diagnostic approach. Treatment of influenza in
otherwise healthy children is often not required;
whether treated or not, the clinical outcomes of
presumed influenza encephalitis are generally good,
especially when oseltamivir and neurosupportive
treatment are promptly instituted.5
A practical diagnostic distinction has been made between acute influenza encephalitis—occurring within a few days of confirmed infection
and influenza encephalopathy, which occurs within
3 weeks after diagnosis, after respiratory symptoms
have resolved.4 6 Clinical treatment is essentially the
same.7 8
Another underrecognised cause of encephalitis
is Epstein-Barr virus (EBV), the usual cause of
glandular fever in teenagers and young adults. An
important differential diagnosis is streptococcal
pharyngitis or tonsillitis. We have encountered
unwell teenagers with tonsillitis, cervical
lymphadenitis, atypical lymphocytosis, and normal
inflammatory markers but negative rapid throat
streptococcal antigen test results. Prompt diagnosis
of EBV glandular fever can help avoid unnecessary
antibiotics (personal communication). Epstein-Barr virus is a herpesvirus that becomes latent in
B lymphocytes after primary infection, which is
often asymptomatic. Reviews of EBV encephalitis
suggest it is more common than previously thought,
particularly in children.9 10 11 12 13 As with influenza, most
cases resolve spontaneously with few sequelae, and
the diagnostic criteria remain poorly defined.
In EBV encephalitis, EBV DNA is more
frequently detected in CSF polymerase chain
reaction, particularly in cases that involve reactivated
EBV infection.9 However, such EBV DNA–positive
CSF results are often interpreted and dismissed as
benign ‘bystander’ EBV reactivations assumed to
play no role in the current illness.
Similar to influenza encephalitis, EBV
encephalitis presents with a wide range of
symptoms, including headache, fever, nausea,
vomiting, tonsillitis, myalgia, and neurological
manifestations such as cerebellar syndromes, tonic-clonic
seizures, meningism, hypotonia, myalgia,
psychiatric disorders, and cognitive, sensory or visual
impairments. Brain imaging may show white matter
changes in the cerebellum, basal ganglia, frontal
lobe, and cerebral cortex, and electroencephalogram
findings may be normal or indicate diffuse slowing.9
However, none of these features is specific to EBV
encephalitis and may also be found with other viral
causes.
Diagnosis of EBV encephalitis is therefore
often made by exclusion when no other pathogen
is identified. Where treatment has been initiated,
intravenous acyclovir or ganciclovir (although
neither is licensed for EBV treatment) has been used,
with or without corticosteroids—or corticosteroids
alone, often with good outcomes.9 Although the
direct efficacy of acyclovir and ganciclovir against
EBV encephalitis is doubtful, they may help suppress
concurrent reactivation of herpes simplex virus
(HSV)–1, which could otherwise lead to more severe
HSV-1 encephalitis.
Acute encephalitis due to dual or simultaneous
coinfections by EBV and influenza is theoretically
possible and may cause diagnostic dilemma.
However, a PubMed review of literature does not
identify any report. In any case, treatment will
essentially be the same by using specific antiviral
medications for both viruses.
Viral encephalitis is inflammation of the brain
caused by a virus.14 Diagnosis is based on symptoms,
travel history, and investigations such as histology,
imaging, and lumbar puncture. Many viruses can cause
encephalitis.15 These viruses often replicate outside
the central nervous system before triggering diverse
forms of viral encephalitis. Differential diagnosis
helps rule out non-infectious encephalitis.14 Some
viruses have characteristic symptoms of infection
that may aid diagnosis.16 A broad differential
diagnosis should be considered, including infectious
and non-infectious aetiologies (eg, malignancy,
autoimmune or paraneoplastic encephalitis, abscess, tuberculosis, drug reactions, vascular or
metabolic disease).15 16 17 It may not always be possible
to distinguish viral encephalitis from immune-mediated
inflammatory central nervous system
diseases (eg, acute disseminated encephalomyelitis
and immune-mediated encephalitis) in children.18
Symptoms usually occur acutely, with fever, stiff
neck, headache, altered mental status, photophobia,
vomiting, confusion, and, in severe cases, seizures,
paralysis, or coma.16 18 Most cases are mild.15
Neuroimaging and lumbar puncture are essential14;
computed tomography or magnetic resonance
imaging can identify increased intracranial pressure
and the risk of uncal herniation. Cerebrospinal
fluid should be analysed for opening pressure, cell
counts, glucose, protein, and immunoglobulin G and
immunoglobulin M antibodies. Polymerase chain
reaction testing for HSV-1, HSV-2, and enteroviruses
is also recommended. Where indicated, brain
biopsy and body fluid specimen cultures may assist.
Electroencephalogram findings are abnormal in
over 80% of viral encephalitis cases, and continuous
monitoring may be needed to identify nonconvulsive
status epilepticus.15 18
Thus, if clinical outcomes are generally good
with current non-specific supportive management
protocols, even in the absence of a specific cause,
there may be little additional value in defining
a precise diagnosis. Brain biopsy to confirm the
exact cause is usually unnecessary. Treatment is
usually supportive, with antivirals such as acyclovir
for herpes simplex encephalitis. Where specific
treatment (eg, oseltamivir for influenza) is available,
it should be used because it may alleviate encephalitic
symptoms. Furthermore, once a diagnosis of
encephalitis is made, the clinical team can avoid
extensive investigation for other causes, reassured
that most cases resolve with appropriate supportive
care and good outcomes.
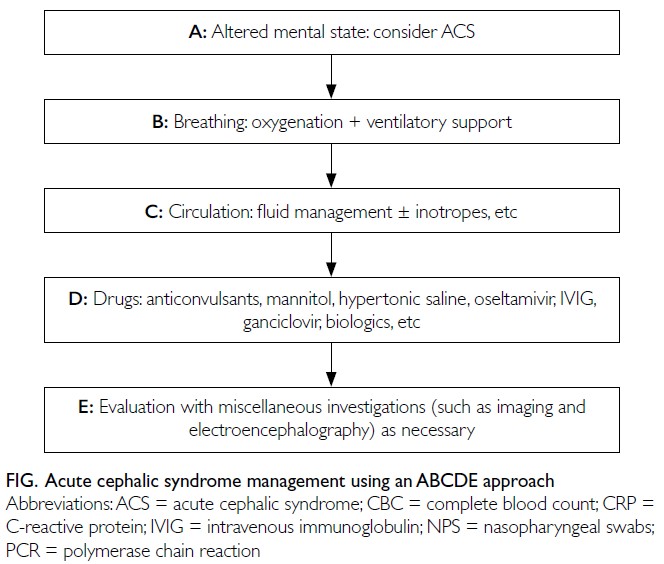
In conclusion, infection or infectionassociated
encephalitis and encephalopathy can
often be managed empirically. A definitive diagnosis
can support targeted antiviral therapy and reduce
unnecessary investigations, provided the diagnosis
is robust. We propose a flowchart to guide frontline
physicians and paediatricians in the diagnosis and
management of these conditions (Fig). Because it
is often impractical or impossible to confirm the
presence of the causative infectious agent in the brain
parenchyma, there is limited relevance in labelling
the condition as encephalitis or encephalopathy. The
term acute cephalic syndrome (ACS) may be more
appropriate. The cardinal symptom of ACS is an
altered or fluctuating mental state. Irrespective of
whether the aetiology is infectious, para-infectious,
or non-infectious, the ABCDE approach should aid
physicians during initial management of patients
with ACS.
Author contributions
Both authors contributed equally to the concept or design,
acquisition of data, analysis or interpretation of data, drafting
of the manuscript, and critical revision of the manuscript for
important intellectual content. Both authors had full access to
the data, contributed to the study, approved the final version
for publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in
the peer review process. The other author has declared no
conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Hon KL. Successful treatment of influenza A
encephalopathy. Hong Kong Med J 2020;26:154. Crossref
2. Centre for Health Protection, Department of Health, Hong
Kong SAR Government. Seasonal influenza vaccination
& pneumococcal vaccination arrangement for 2020/21.
Available from: https://www.chp.gov.hk/files/pdf/sivpv_vaccination_arrangement_for_2020_2021.pdf . Accessed 31 Jan 2025.
3. Hon KL, Tang JW. Low mortality and severe complications
despite high influenza burden among Hong Kong children.
Hong Kong Med J 2019;25:497-8. Crossref
4. Steininger C, Popow-Kraupp T, Laferl H, et al. Acute
encephalopathy associated with influenza A virus infection.
Clin Infect Dis 2003;36:567-74. Crossref
5. Hui WF, Leung KK, Au CC, et al. Clinical characteristics
and outcomes of acute childhood encephalopathy in a
tertiary pediatric intensive care unit. Pediatr Emerg Care
2022;38:115-20. Crossref
6. Edet A, Ku K, Guzman I, Dargham HA. Acute
influenza encephalitis/encephalopathy associated with
influenza a in an incompetent adult. Case Rep Crit Care 2020;2020:6616805. Crossref
7. Ochi N, Takahashi K, Yamane H, Takigawa N. Acute
necrotizing encephalopathy in an adult with influenza A
infection. Ther Clin Risk Manag 2018;14:753-6. Crossref
8. Au CC, Hon KL, Leung AK, Torres AR. Childhood
infectious encephalitis: an overview of clinical features,
investigations, treatment, and recent patents. Recent Pat
Inflamm Allergy Drug Discov 2020;14:156-65. Crossref
9. Peuchmaur M, Voisin J, Vaillant M, et al. Epstein-Barr virus
encephalitis: a review of case reports from the last 25 years.
Microorganisms 2023;11:2825. Crossref
10. Hashemian S, Ashrafzadeh F, Akhondian J, Beiraghi Toosi M.
Epstein-Barr virus encephalitis: a case report. Iran J Child
Neurol 2015;9:107-10.
11. Akkoc G, Kadayifci EK, Karaaslan A, et al. Epstein-Barr
virus encephalitis in an immunocompetent child: a case
report and management of Epstein-Barr virus encephalitis.
Case Rep Infect Dis 2016;2016:7549252. Crossref
12. Cheng H, Chen D, Peng X, Wu P, Jiang L, Hu Y. Clinical
characteristics of Epstein-Barr virus infection in the
pediatric nervous system. BMC Infect Dis 2020;20:886. Crossref
13. Rzhevska OO, Khodak LA, Butenko AI, et al. EBV-encephalitis in children: diagnostic criteria. Wiad Lek
2023;76:2263-8.Crossref
14. Venkatesan A, Tunkel AR, Bloch KC, et al. Case definitions,
diagnostic algorithms, and priorities in encephalitis:
consensus statement of the international encephalitis
consortium. Clin Infect Dis 2013;57:1114-28. Crossref
15. Said S, Kang M. Viral encephalitis. StatPearls. 8 August
2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470162/. Accessed 28 Mar 2025.
16. Schibler M, Eperon G, Kenfak A, Lascano A, Vargas MI,
Stahl JP. Diagnostic tools to tackle infectious
causes of encephalitis and meningoencephalitis in
immunocompetent adults in Europe. Clin Microbiol Infect
2019;25:408-14. Crossref
17. Bradshaw MJ, Venkatesan A. Herpes simplex virus–1
encephalitis in adults: pathophysiology, diagnosis, and
management. Neurotherapeutics 2016;13:493-508. Crossref
18. Costa BK, Sato DK. Viral encephalitis: a practical review
on diagnostic approach and treatment. J Pediatr (Rio J)
2020;96 Suppl 1:12-9. Crossref