Hong Kong Med J 2026;32:Epub 29 Jan 2026
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PERSPECTIVE
From workplace-based assessment to
programmatic assessment: continuing the
evolution of medical assessment to support
competency-based medical education
HY So, FHKAM (Anaesthesiology)1; Albert KM Chan, FHKAM (Anaesthesiology)2; Benny CP Cheng, FHKAM (Anaesthesiology)2
1 Hong Kong Academy of Medicine, Hong Kong SAR, China
2 The Jockey Club Institute for Medical Education and Development, Hong Kong Academy of Medicine, Hong Kong SAR, China
Corresponding author: Dr HY So (sohingyu@fellow.hkam.hk)
Introduction
In our article on workplace-based assessment (WBA),
we outlined how WBAs represent an important step
in the evolution of medical education assessment.1
By focusing on real-time evaluation and providing
formative feedback, WBAs allow learners to refine
their clinical performance in actual patient-care
settings. However, WBAs alone—similar to any
single assessment method—have limitations. As van
der Vleuten2 noted, no single assessment method
can comprehensively meet all quality criteria, such
as reliability, validity, educational impact, and cost.
Reliance on a single approach limits the breadth of
information that can be gathered about a learner’s
abilities, much like relying on a single laboratory test
to diagnose a complex medical condition.
Programmatic assessment overcomes these
limitations by combining multiple assessment
methods in a complementary fashion to provide
a more comprehensive and accurate evaluation of
learner competence.3 4 This approach—a cornerstone
of competency-based medical education (CBME)—offers a more holistic and continuous form of
assessment.5 In this article, we discuss the rationale
behind the shift from traditional assessments to
programmatic assessment, the principles that
underlie this model, and how it can be successfully
implemented in postgraduate medical training
programmes.
Limitations of traditional
assessment
Traditional assessments often rely heavily on
high-stakes examinations at the end of a course or
programme. Although these examinations serve a
purpose, they fail to fully support the development
of clinical competence as required in CBME.5
High-stakes examinations typically induce anxiety,
promote short-term memorisation, and do not
capture the complexities of real-world clinical
decision-making. When examinations are regarded as make-or-break moments, learners often shift
their focus from genuine understanding to mere
performance, which does not support long-term
mastery.6
Several specific limitations of traditional
assessments include:
Programmatic assessment is designed to
address these shortcomings. By incorporating
multiple data points and reducing reliance on any
single examination, it provides a more nuanced and
comprehensive evaluation of learners’ progression
and competencies.
Core principles of programmatic
assessment
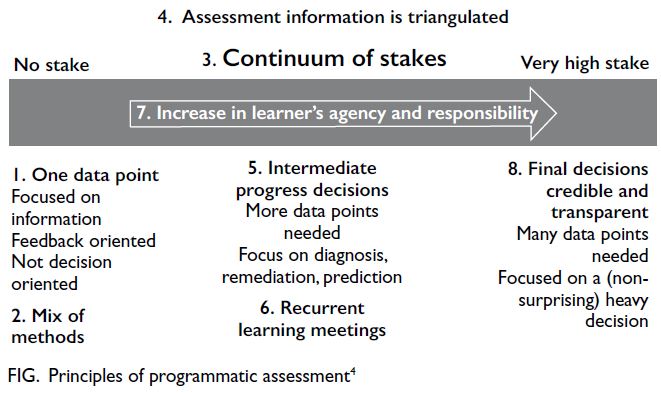
Programmatic assessment is based on a set of
principles derived from educational theories10 that
promote a comprehensive, learner-centred approach
to medical education (Fig4):
1. “Every assessment is but a data point, which
should be optimised for learning by giving
meaningful feedback to the learner. Pass/fail
decisions are not given on a single data-point.”4
No single assessment can reliably determine a learner’s progression. In programmatic assessment, each assessment—whether formative or summative—contributes to a cumulative understanding of the learner’s abilities. This is similar to using multiple diagnostic tools to form a complete clinical picture. Overall judgement of the learner’s competence is made by aggregating these data points over time. At this stage, the focus is on providing meaningful feedback to facilitate learning.4
2. “Use a mix of assessment methods; the choice of method depends on the educational justification for using that method.”4
Competence in medical practice is multidimensional, and different assessment methods capture distinct facets of a learner’s development. Programmatic assessment uses a mix of standardised tests (such as multiple-choice examinations or objective structured clinical examinations [OSCEs]) and non-standardised methods (such as narrative feedback or direct observation during WBAs). This approach mirrors clinical practice, where a combination of laboratory tests, imaging, and clinical examinations provides a comprehensive understanding of a patient’s condition.4
No single assessment can reliably determine a learner’s progression. In programmatic assessment, each assessment—whether formative or summative—contributes to a cumulative understanding of the learner’s abilities. This is similar to using multiple diagnostic tools to form a complete clinical picture. Overall judgement of the learner’s competence is made by aggregating these data points over time. At this stage, the focus is on providing meaningful feedback to facilitate learning.4
2. “Use a mix of assessment methods; the choice of method depends on the educational justification for using that method.”4
Competence in medical practice is multidimensional, and different assessment methods capture distinct facets of a learner’s development. Programmatic assessment uses a mix of standardised tests (such as multiple-choice examinations or objective structured clinical examinations [OSCEs]) and non-standardised methods (such as narrative feedback or direct observation during WBAs). This approach mirrors clinical practice, where a combination of laboratory tests, imaging, and clinical examinations provides a comprehensive understanding of a patient’s condition.4
For standardised assessments, it is
important to recognise that competence is
content-specific—a learner’s performance in one
scenario or question may not reliably predict
performance in another. Thus, standardised
assessments require large samples of data
to ensure reliability. This applies equally to
objective tests (eg, multiple-choice questions)
and more subjective assessments, such as oral
examinations. Broad sampling of questions
and examiners enhances validity. Additionally,
quality assurance measures must be established
to ensure fairness and relevance to intended
competencies.10
For non-standardised assessments, the
emphasis lies in real-life application and
expert judgement. Bias is inherent, but it can
be minimised by using multiple assessors and
multiple assessments over time. Feedback
should be narrative, offering deeper insights
into performance. Validity depends on adequate
preparation of both trainers and trainees.11
3. “Distinction between summative and formative is
replaced by a continuum of stakes, and decision-making
on learner progress is proportionally
related to the stakes.”4
In traditional assessments, the distinction between formative (low-stakes) and summative (high-stakes) is clear. In programmatic assessment, this becomes more fluid. Low-stakes assessments guide learning and improvement, while high-stakes assessments are used for certification or other key decisions. The amount of evidence required is proportional to the stakes involved, similar to monitoring a patient’s condition over time—minor issues are addressed early on, whereas major decisions (eg, surgery) are based on cumulative understanding of the patient’s health.4
4. “Assessment information is triangulated across data-points.”4
Information pertaining to the same content is triangulated, similar to synthesising laboratory results, imaging, and patient history in diagnosis. For example, history-taking skills can be assessed using an OSCE, a mini-clinical evaluation exercise, and patient feedback. This method of aggregating results is more meaningful than aggregating by test format.4
5. “Intermediate reviews are made to discuss and decide with the learner on their progress.”4
Learners meet regularly with mentors or supervisors to reflect on feedback and adjust learning plans, much like adjusting a treatment based on new laboratory results. These intermediate reviews prevent surprising high-stakes decisions at the end of the programme.4
6. “Learners have recurrent learning meetings with faculty using a self-analysis of all assessment data.”4
Self-assessment is critical for learners to become self-directed professionals. Learners are encouraged to review their portfolio data and discuss with mentors. Initially, guidance from trainers is required for self-assessment to foster deeper learning and professional development.4
7. “Learners are increasingly accountable for their learning.”4
Over time, learners are expected to take greater responsibility for their learning, similar to patients who assume greater ownership of their health as they become more informed about their condition. This shift in responsibility helps prepare learners for independent practice and fosters lifelong learning.4
8. “High-stakes decisions are made in a credible and transparent manner.”4
High-stakes decisions, such as those related to certification, are based on multiple assessments collected over time. This approach ensures that decisions are fair and reflect a holistic understanding of the learner’s competence. Much like the review of a complex clinical case by a multidisciplinary team, programmatic assessment enables thorough and transparent decision-making.4
In traditional assessments, the distinction between formative (low-stakes) and summative (high-stakes) is clear. In programmatic assessment, this becomes more fluid. Low-stakes assessments guide learning and improvement, while high-stakes assessments are used for certification or other key decisions. The amount of evidence required is proportional to the stakes involved, similar to monitoring a patient’s condition over time—minor issues are addressed early on, whereas major decisions (eg, surgery) are based on cumulative understanding of the patient’s health.4
4. “Assessment information is triangulated across data-points.”4
Information pertaining to the same content is triangulated, similar to synthesising laboratory results, imaging, and patient history in diagnosis. For example, history-taking skills can be assessed using an OSCE, a mini-clinical evaluation exercise, and patient feedback. This method of aggregating results is more meaningful than aggregating by test format.4
5. “Intermediate reviews are made to discuss and decide with the learner on their progress.”4
Learners meet regularly with mentors or supervisors to reflect on feedback and adjust learning plans, much like adjusting a treatment based on new laboratory results. These intermediate reviews prevent surprising high-stakes decisions at the end of the programme.4
6. “Learners have recurrent learning meetings with faculty using a self-analysis of all assessment data.”4
Self-assessment is critical for learners to become self-directed professionals. Learners are encouraged to review their portfolio data and discuss with mentors. Initially, guidance from trainers is required for self-assessment to foster deeper learning and professional development.4
7. “Learners are increasingly accountable for their learning.”4
Over time, learners are expected to take greater responsibility for their learning, similar to patients who assume greater ownership of their health as they become more informed about their condition. This shift in responsibility helps prepare learners for independent practice and fosters lifelong learning.4
8. “High-stakes decisions are made in a credible and transparent manner.”4
High-stakes decisions, such as those related to certification, are based on multiple assessments collected over time. This approach ensures that decisions are fair and reflect a holistic understanding of the learner’s competence. Much like the review of a complex clinical case by a multidisciplinary team, programmatic assessment enables thorough and transparent decision-making.4
Implementing programmatic
assessment
The implementation of programmatic assessment
clearly requires transformative changes to our
assessment system. The Royal College of Physicians
and Surgeons of Canada has adopted a Competence
by Design approach to implement CBME, serving
as a ‘hybrid’ model that blends a competency-based
framework within the existing system.12 Similarly, the
transition in our assessment system can be guided by
applying the following principles of programmatic
assessment while building on the structure of the
current framework.
Provide meaningful feedback
A cornerstone of programmatic assessment is
detailed feedback. Traditional methods such as grades or pass/fail results offer limited insight, whereas
narrative feedback can help learners understand
the nuances of their performance. While we have
highlighted the value of feedback in WBA, it should
also be incorporated into other forms of assessment.
For example, detailed feedback after an OSCE could
break down performance in communication, clinical
reasoning, and technical skills, helping learners
target areas for improvement.13
Establish a reliable system for collecting
information
All assessment data, including feedback, reflective
reports, and performance outcomes, must be
systematically collected to enable learners and
educators to monitor progress over time. e-Portfolios
play a crucial role in programmatic assessment,
serving as essential tools for tracking these data.
An effective e-portfolio should be user-friendly,
facilitating seamless access and integration across
various platforms.13 14
Organise intermediate assessments
Portfolios are only valuable if they are actively used to
promote learning. Regular intermediate assessments
play a key role by offering diagnostic, therapeutic,
and prognostic insights. These assessments ensure
that learners receive timely feedback on their
current performance, understand areas requiring
improvement, and have a clear sense of their future
trajectory. By providing of ongoing guidance, they
help prevent unexpected outcomes at the end of
programmes and enable timely interventions when
needed.13 14
Adapt high-stakes examinations for
competency-based medical education
Although CBME relies heavily on frequent low-stakes
assessments, high-stakes examinations
continue to hold value. However, these examinations
must be adapted to align with the CBME framework.
The optimal approach is still evolving. The Royal
College of Physicians and Surgeons of Canada
has implemented several changes that are worth
considering.15
Earlier timing
Scheduling examinations earlier in training allows
learners to demonstrate competence sooner, freeing
up time in later stages to focus on clinical practice.
Integration with other assessments
Examinations should complement WBAs by
focusing on competencies that are more difficult to
assess in clinical settings, such as the management of
rare conditions.
Sequencing
Written examinations should precede practical
or oral examinations, ensuring learners have
the necessary foundational knowledge before
progressing to more complex skills.
Global rating scales
In practical examinations, transitioning from
checklists to global ratings encourages the
assessment of higher-order clinical decision-making,
rather than rote memorisation of facts.
Updated psychometrics
New psychometric approaches focus on decision
consistency, ensuring that examinations measure
true competence rather than simply comparing
learners with their peers.
Promote faculty development
As assessment methods and tools are only as
effective as the faculty who utilise them, it is essential
that faculty develop the competencies required for
accurate assessment and effective feedback. Strong
leadership, supported by a committed faculty, has
been identified as the most important factor enabling
implementation of programmatic assessment.16 17
The Hong Kong Academy of Medicine has developed
a comprehensive faculty development framework
for trainers, examiners, supervisors of training, and
collegial leads.18 Additionally, it is crucial to prepare
trainees for this new assessment model. Training
programmes are either currently in place or will
soon be introduced to support and facilitate this
transition.
Ensure reliable decision-making
For high-stakes decisions, such as passing or
promoting a learner, it is essential to consider a
comprehensive range of data gathered from diverse
settings, methods, and assessors. These data should
include both quantitative measures and qualitative
feedback, such as written or verbal evaluations.
Professional judgement is required to effectively
interpret and synthesise this information. Given
the significant consequences of these decisions,
it is critical to ensure that the process is fair and
trustworthy.12 To support the integrity of this
decision-making process, recommendations have
been established for procedural measures and
quality assurance frameworks.8 19
Evaluate and adapt the programme
Like any curriculum, an assessment programme
must undergo regular evaluation to identify potential
issues and areas for improvement. Continuous
monitoring ensures the programme remains aligned with its goals and is responsive to learner and faculty
feedback. This process is essential to maintain
the relevance and effectiveness of programmatic
assessment.13
Conclusion
Programmatic assessment represents a major
advancement in medical education by integrating
diverse assessment methods, providing continuous
feedback, and using multiple data points to make
informed decisions. This learner-centred approach
helps ensure that future clinicians are equipped to
meet the challenges of modern healthcare, much like
a comprehensive, multidisciplinary treatment plan
supports better outcomes for patients.
As articulated in our Position Paper on
Postgraduate Medical Education,9 we are progressing
along the journey towards CBME, within which
programmatic assessment is a key component. In
this context, there is a clear need to review Hong
Kong’s assessment systems to ensure alignment
with CBME principles. However, such progression
does not imply the complete replacement of high-stakes
examinations. Even in countries that have
advanced further along the CBME journey, high-stakes
examinations continue to serve important
roles in maintaining standards and ensuring public
accountability.15 The priority, therefore, is not to
abolish such examinations but to integrate them
within a programmatic framework that values
multiple sources of evidence, meaningful feedback,
and longitudinal decision-making. The evolution
towards programmatic assessment should be
viewed as a gradual and deliberate process requiring
sustained faculty development, structural support,
and system-level coordination.
Author contributions
Concept or design: All authors.
Acquisition of data: HY So.
Analysis or interpretation of data: HY So, AKM Chan.
Drafting of the manuscript: HY So.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: HY So.
Analysis or interpretation of data: HY So, AKM Chan.
Drafting of the manuscript: HY So.
Critical revision of the manuscript for important intellectual content: All authors.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency
in the public, commercial, or not-for-profit sectors.
References
1. So HY, Choi YF, Chan PT, Chan AK, Ng GW, Wong GK.
Workplace-based assessments: what, why, and how to
implement? Hong Kong Med J 2024;30:250-4. Crossref
2. van der Vleuten CP. The assessment of professional
competence: developments, research and practical implications. Adv Health Sci Educ Theory Pract 1996;1:41-67. Crossref
3. Schuwirth LW, van der Vleuten CP. Programmatic
assessment: from assessment of learning to assessment for
learning. Med Teach 2011;33:478-85. Crossref
4. Henneman EA, Cunningham H. Ottawa 2020 consensus
statement for programmatic assessment—1. Agreement
on the principles. Med Teach 2021;43:1139-48. Crossref
5. Van Melle E, Frank JR, Holmboe ES, et al. A core
components framework for evaluating implementation
of competency-based medical education programs. Acad
Med 2019;94:1002-9. Crossref
6. Bok HG, Teunissen PW, Favier RP, et al. Programmatic
assessment of competency-based workplace learning:
when theory meets practice. BMC Med Educ 2013;13:123. Crossref
7. Cilliers FJ, Schuwirth LW, Herman N, Adendorff HJ, van
der Vleuten CP. A model of the pre-assessment learning
effects of summative assessment in medical education. Adv
Health Sci Educ Theory Pract 2012;17:39-53. Crossref
8. van der Vleuten C, Heeneman S, Schuwirth LW.
Programmatic assessment. In: Dent J, Harden RM, Hunt D,
editors. A Practical Guide for Medical Teachers. 6th ed.
Elsevier; 2021: 295-303.
9. So HY, Li PK, Lai PB, et al. Hong Kong Academy of Medicine
position paper on postgraduate medical education 2023.
Hong Kong Med J 2023;29:448-52. Crossref
10. Torre DM, Schuwirth LW, van der Vleuten CP. Theoretical
considerations on programmatic assessment. Med Teach
2020;42:213-20. Crossref
11. van der Vleuten CP, Schuwirth LW, Scheele F, Driessen EW,
Hodges B. The assessment of professional competence: building blocks for theory development. Best Pract Res
Clin Obstet Gynaecol 2010;24:703-19. Crossref
12. Frank JR, Karpinski J, Sherbino J, et al. Competence by
Design: a transformational national model of time-variable
competency-based postgraduate medical education.
Perspect Med Educ 2024;13:201-23. Crossref
13. van der Vleuten CP, Schuwirth LW, Driessen EW,
Govaerts MJ, Heeneman S. Twelve tips for programmatic
assessment. Med Teach 2015;37:641-6. Crossref
14. van Tartwijk J, Driessen E. Portfolios for assessment and
learning: AMEE Guide No. 45. Med Teach 2009;31:790-801. Crossref
15. Bhanji F, Naik V, Skoll A, et al. Competence by Design: the
role of high-stakes examinations in a competence based
medical education system. Perspect Med Educ 2024;13:68-74. Crossref
16. Iobst WF, Holmboe ES. Programmatic assessment: the
secret sauce of effective CBME implementation. J Grad
Med Educ 2020;12:518-21. Crossref
17. Torre D, Rice NE, Ryan A, et al. Ottawa 2020 consensus
statements for programmatic assessment—2.
Implementation and practice. Med Teach 2021;43:1149-60. Crossref
18. So HY, Li PK, Cheng BC; Faculty Development
Workgroup, Hong Kong Jockey Club Innovative Learning
Centre for Medicine; Leung GK. Faculty development
for postgraduate medical education in Hong Kong. Hong
Kong Med J 2024;30:428-30. Crossref
19. Uijtdehaage S, Schuwirth LW. Assuring the quality of
programmatic assessment: moving beyond psychometrics.
Perspect Med Educ 2018;7:350-1. Crossref