© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
HEALTHCARE FOR SOCIETY
The Hong Kong Hospital Authority reform: a
historical perspective
Foreword
Fei-chau Pang, MB, ChB, FHKAM (Community Medicine)
President, Hong Kong College of Community Medicine, Hong Kong SAR, China
The Hong Kong College of Community Medicine
is pleased to present a special edition of a series of
articles written by Dr William Ho JP,1 our Honorary
Fellow and former Chief Executive of the Hong Kong
Hospital Authority (HA), on the HA’s early history
as well as his insightful reflections. More than three
decades have passed since the inception of the HA
in December 1990. At the time, the HA reform was
hailed as an unprecedented successful management
transformation exercise, galvanising the energy of
healthcare professionals to improve service quality
by leaps and bounds. Upon leaving the HA in 2005,
Dr Ho began writing about this part of Hong Kong’s
health system’s history, from the unique angle and
vantage point of a frontline clinician in the pre-HA
era, a doctors’ union leader involved in negotiations
with the Government during the transition period,
and subsequently as a medical administrator in
the newly formed HA, working all the way to the
top position of Chief Executive. His focus was not
so much on the detailed chronology of events,
but on the socio-economic, political, managerial
and philosophical underpinnings that shaped the
trajectory of the HA reform.
Today, the organisation is once again
approaching a critical point, facing challenges of
increasing demand, long waiting times, and staff
shortages. Last year, the Government called upon
the HA to conduct ‘a comprehensive review of
the systemic issues and the need for reform with
regard to the management of public hospitals.’2 It
is noteworthy that many of the problems currently
encountered are not dissimilar to those Dr Ho
described in the pre-HA era. Given the passage of
time and changes in the environment, many of the
original ideas and concepts should be reinstalled
in the organisation’s memory and laid down as
a foundation for future faculty development in
healthcare management. From the perspective of
our Administrative Medicine subspecialty, such
historical material is most valuable for sharing
and learning, particularly for Fellows in healthcare
leadership roles. We also believe it will have a wider impact on the medical community and even
the lay public. Hence, we have discussed with Dr
Ho, who has kindly reviewed and suitably revised
what he wrote back then, culminating in a trilogy
of articles for the Hong Kong Medical Journal. We
are also grateful to the journal’s Editorial Board for
facilitating the publication as a special series.
Part 1: From pre–Hospital
Authority era to establishment of the Hospital Authority
William SW Ho, FCSHK, FHKCCM
Hong Kong College of Community Medicine, Hong Kong SAR,
China
This article series, comprising three parts (Part 1 to
Part 3), attempts to describe and analyse the early
history of the Hong Kong Hospital Authority (HA)
reform, from its inception to around the year 2000.
The HA is a huge organisation, second only to
the Civil Service in staff size, shouldering the
lion’s share of healthcare services in Hong
Kong. The process of its establishment and the
extensive reforms of the public hospital system
were most transformational and quite unique in
the international scene. Apart from the dramatic
service improvements achieved, the underlying
management concepts, philosophy and methods
were exemplary. Yet, there appears to be little in-depth
study on this epic journey, either within or
outside the organisation. As time has passed and
circumstances have changed, there is a feeling of
‘lost organisational memory’ in how the HA came
about and the underlying spirit of its systems and
processes, as reflected to the author by executives
and clinicians.
Background to the reform
Public health services in the 1980s
Public health services in Hong Kong traditionally
were under the purview of the Health and Welfare
Branch of the Hong Kong Government Secretariat,
and provided through the Medical and Health
Department (M&HD). The Director of Medical
and Health Services was in charge of the public
health functions and operation of the Government hospitals. In 1985, 47% of all hospital beds were in
Government hospitals,3 while another 41% were in
Subvented hospitals4 run by charitable organisations
such as the Tung Wah Group of Hospitals,
Caritas Hong Kong, and so on. The remainder were
in private hospitals. While the parent organisations
of Subvented hospitals owned the land and buildings,
as well as managed these hospitals’ operations and
staff, the operating costs were increasingly subsidised
by the Government, hence the term ‘Subvented’. In
general, their hospital equipment, staff terms and
training opportunities were inferior compared with
Government hospitals. Public hospital services were
highly subsidised and fees were nominal compared
with the actual cost.
Health services provision in the late 1970s
and early 1980s generally followed the 1974 White
Paper of the Hong Kong Government entitled
The Further Development of Medical and Health
Services in Hong Kong. The main proposals included
organising services on a regional basis, building
new facilities to cater for the needs of the growing
population, particularly in new towns, to achieve a
target of 5.5 hospital beds per 1000 population, and
starting a new medical school, a new nursing school
and a dental school.5 By the mid-1980s, the system
was evidently not coping. One reason was the rapid
increase in the population, which grew by 24.18%
in the 10-year period after 1974, particularly due to
legal and illegal immigrants from Chinese Mainland,
and Vietnamese refugees.6 Serious overcrowding,
particularly in the Government hospitals, with the
infamous ‘camp beds’ lining hospital corridors, was a
public eye sore. Staff discontent, both in terms of the
poor working environment and low morale, resulted
not only in a brain drain to the lucrative private
sector, but also in waves of union actions.7
Vivid accounts of the public hospital scenes at
that time can be found in the book entitled Bedside
Manner: Hospitals and Health Care in Hong Kong by
Robin Hutcheon.8 Observations from people in the
system whom he interviewed could be summarised
as a severe lack of proper management in public
hospitals, poor quality of care, inefficiency in
using Subvented hospitals in the system, jealousy
over unequal staff terms, and hospital Medical
Superintendents being poorly trained for their jobs.8
Approach to the reform
International influence
It is to be noted that Hong Kong was not unique in
having a poorly run public healthcare service. In the
United Kingdom, the government-commissioned
Griffiths Report of 19839 severely criticised its
National Health Service (NHS), and recommended
wholesale management reform. This was quickly
embraced and implemented by the Thatcher government. The United Kingdom’s experience
then influenced other Commonwealth countries
such as Australia, New Zealand and Singapore,
where similar reforms were planned for their public
health systems. Indeed, managerial reform of public
entities to improve performance was the trend of the
period in many countries. This ranged from internal
management strengthening, corporatisation ‘hiving
off’ Civil Service functions to be run by corporate
entities, to outright privatisation. An example in
Hong Kong would be the formation of the Housing
Authority in 1973 to introduce professional housing
management.10
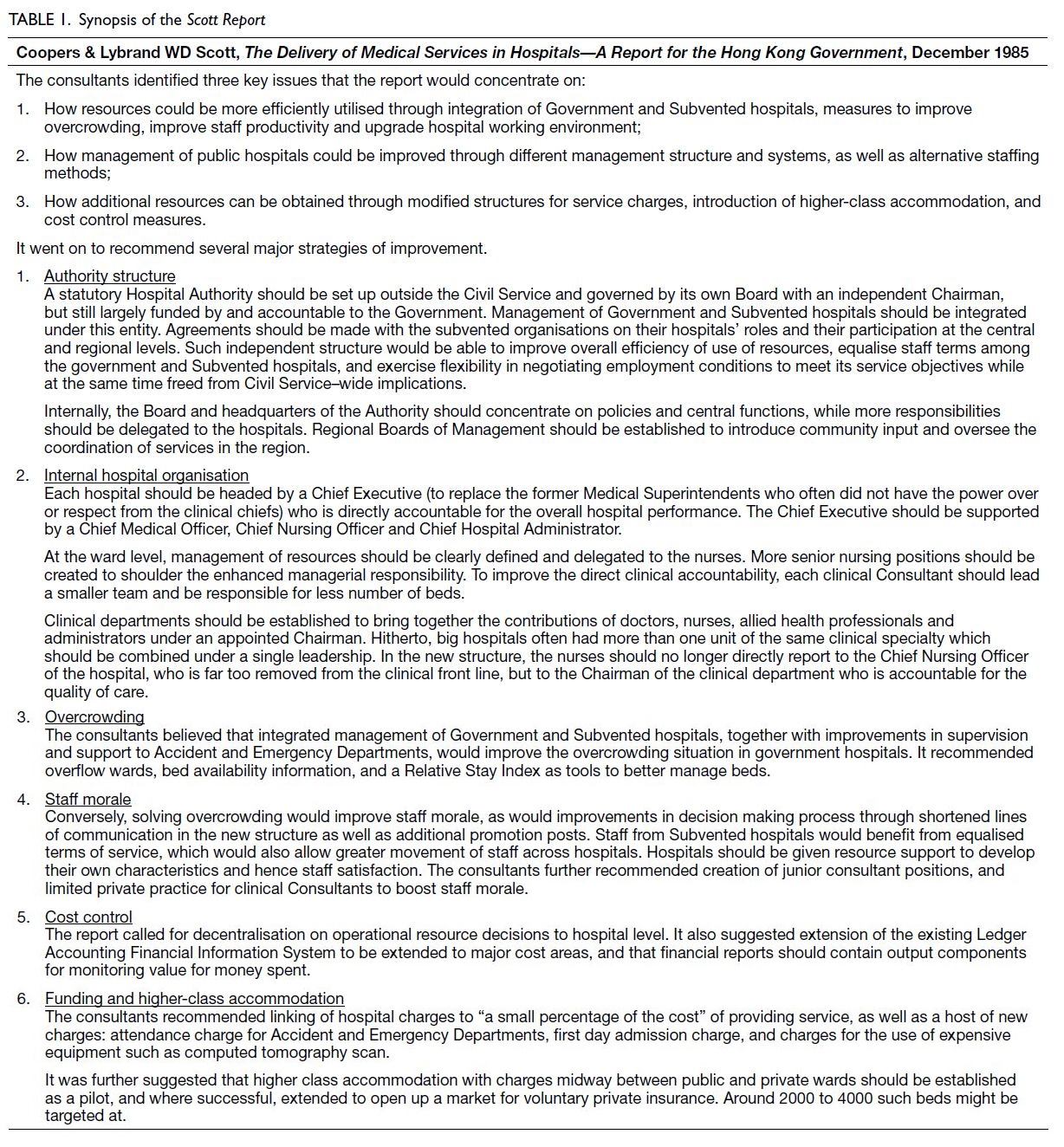
Consultancy study
Facing increasing public discontent over the quality
of the public hospital services, several legislators
pressed for change, including Dr Harry Fang 方心讓,
Dr Henrietta Ip 葉文慶, and Ms Lydia Dunn 鄧蓮如.
The Secretary for Health and Welfare Mr Henry
Ching 程慶禮 proposed calling in consultants to
conduct an overall review, which was approved by the
Executive Council. The job was eventually awarded
to Coopers & Lybrand, WD Scott from Australia,
who published their report in December 1985 (the
Scott Report) [Table 1]. A key recommendation
was to take the whole public hospital system away
from the M&HD, to be managed by an independent
Hospital Authority, free from the constraints of the
Civil Service.
At the outset, however, the consultancy study
was criticised for its limited scope, which even the
consultants themselves admitted in their report. As
the pressure at the time was over public hospital
services, the consultants’ brief was merely to look at
how the public hospital system could be improved.11
This approach of excluding the public health and
primary care sides of the healthcare system from the
reform proposal sowed the seed for eventual over-reliance
on hospital systems and fragmentation.
Such weakness was particularly felt much later
during the SARS (severe acute respiratory syndrome)
epidemic of 2003 when coordination between the
hospital and public health sides was most vital for
the success of control.
Political process
Public and stakeholder consultation
The Government conducted public consultation on
the Scott Report in 1986. Public opinion welcomed
proposals on enhancing community participation
and the overall objective of management reform
in public hospitals, but vehemently objected to the
suggestion of linking service fees to a percentage
of the cost. Staff working in Subvented hospitals
welcomed the proposals, as they expected better
pay and a more equitable allocation of resources to their hospitals, even though the directors of the
parent organisations feared a loss of autonomy. Civil
Servants working in Government hospitals, however,
opposed to the proposal, which threatened to cut
their existing benefits in order to equalise terms
with Subvented hospital staff, and possibly reduce job stability compared with Civil Servants. Nursing
unions also opposed the proposed change that would
place nurses under the doctors’ management in the
new clinical departmental structure.
The OMELCO (Office of Members of the
Executive and Legislative Councils) Standing Panel on Health Services, as presented by the then medical
constituency representative Dr Hin-kwong Chiu
招顯洸 was generally in favour of the HA
proposal.12 The Governor-in-Council Sir David
Wilson 港督衛奕信 announced in his Policy Speech
on 7 October 1987 the decision to proceed with the
establishment of an HA to integrate the management
of all Government and Subvented hospitals into
a single system, and to introduce the necessary
management reform. To prepare for the change, the
original M&HD was to be split into a Department
of Health and a Hospital Services Department.
The latter would eventually be abolished upon the
management takeover by the HA. Meanwhile, a
Provisional Hospital Authority (PHA) was to be set
up to plan and prepare for the establishment of the
HA.
A historical twist
Meanwhile, the public hospital system continued
to deteriorate with severe overcrowding, poor
environment, long queues, and overworked staff with
low morale. The exodus of doctors into the private
sector reached a historical high of around 13% for
Government hospitals and exceeded 20% for some
Subvented hospitals in 1988. Sentiments among
members of the Government Doctors’ Association
(GDA)13 culminated in a call for industrial action,
which was echoed by the The Joint Council of
Subvented Hospitals of Hong Kong, and nursing
unions. The plight of overworked doctors gained
the support of some legislators, such as Dr Che-hung
Leong 梁智鴻 and Mr Martin Lee 李柱銘.14
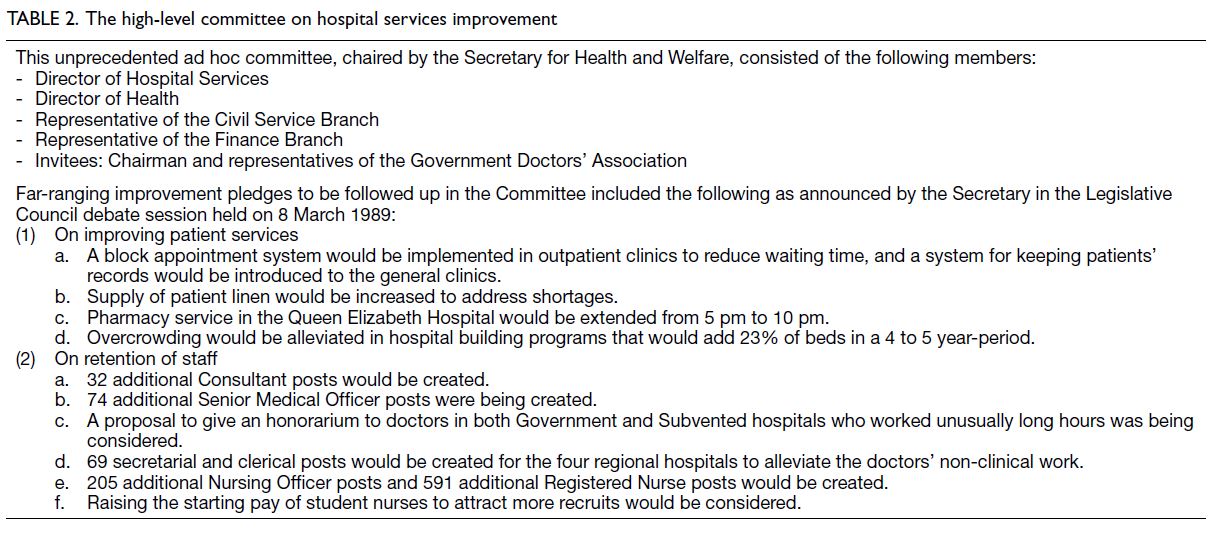
In a symbolic strike that lasted for 10 days from 1 March 1989,15 the GDA was able to win over
public sympathy and succeeded in pressing the
Government to agree to their demand for setting up
a high-level committee, comprising representatives
of relevant Government branches and departments,
as well as GDA representatives. Chaired by the then
Secretary for Health and Welfare Mr Brian Tak-hay
Chau 周德熙, the committee provided a platform for
negotiation and for monitoring progress on promised
improvements, without deferring to the yet-to-be-established
HA. These included plans to eliminate
camp beds, reduce patients’ waiting times in
specialist clinics, improve linen supply for patients,
as well as significantly enhance the salary structure
and promotion opportunities for both doctors and
nurses. The scale of these improvements within such
a short time was unprecedented in the history of the
M&HD (Table 2).
From Provisional Hospital Authority to
Hospital Authority
The PHA was established on 1 October 1988,
chaired by Sir Sze-yuen Chung 鍾士元爵士, a
veteran Executive and Legislative Councillor. The
PHA adopted most of the recommendations of
the Scott Report and developed detailed plans.
The Government published the PHA Report on
1 April 1990. Legislative processes ensued, and
the HA Ordinance was enacted on 1 December
1990, when the HA was formally established, with
Sir Sze-yuen Chung at the helm. Most proposed
changes were planned for phased implementation,
except the proposal to link fees and charges to costs.
Indeed, it was written into the HA Ordinance: “the principle that no person should be prevented, through lack of means, from obtaining adequate medical treatment”.16
Negotiations with the Government on funding
and administrative arrangements turned out to
be complex, as more than 20 other Government
departments had previously served the public
hospitals as part and parcel of their work. Examples
included the Architectural Services Department
looking after hospital buildings and capital projects;
the Electrical and Mechanical Services Department
overseeing building services and hospital equipment;
the Government Supplies Department handling
procurement and inventories; and the Department
of Health with its intricate involvement in hospital
operations. Once the HA was established, however,
it was envisaged that either the HA would have to
take over the work or be cross-charged.
Another dimension was the additional resources
incurred simply because the HA became a separate
legal entity. In the past, Government departments
were deemed exempt from many pieces of legislation.
However, the HA would not enjoy such exemptions
and would incur additional resources to comply with
the myriad requirements of various ordinances. The
Government agreed to allocate additional resources
for the HA to purchase necessary insurance policies,
licences and registration fees. Nevertheless, the full
implications of these requirements could not be
easily appreciated from day one.17
There were also negotiations with staff unions
on new HA terms of employment and ‘bridging-over
terms’, as well as with the boards of directors
of Subvented hospitals, which proceeded in earnest.
For the latter, it was agreed that ownership of land,
properties, and equipment would continue to
belong to the parent organisations, including any
subsequent Government investment in hardware
upgrades. It was also agreed that nominations from
the parent bodies would constitute the majority in
future Hospital Governing Committees.18 Formal
contract signing with all 15 Subvented organisations
that governed 23 hospitals in the system took place
on 24 May 1991.19 In a ‘big bang’ approach, the HA
took over the management of all 38 public hospitals
and 37 000 staff overnight on 1 December 1991.20
Thus, it took merely around 6 years from the
conception of an independent HA, to 1 December
1990, when the HA was formally established,
and another 12 months for the HA to take over
all operations of public hospitals. Given the scale
of public hospital services and the enormity of
major changes to be implemented, this was a most
successful feat, even by international standards.
Such a result could be attributed to congruence with
prevailing societal values and concerns, as well as
major stakeholders’ interests. An attempt to explain
these factors is made below.
Analysis
Societal value system
Hong Kong as a predominantly Chinese society
first and foremost embodied the traditional values
of communitarianism and the Confucian care-based
ideology of good government, particularly
in healthcare.21 At the same time, Hong Kong, as a
British colony for more than a century, had inherited
much of the British system in its social structure.
The public healthcare system was similar to the
British NHS, with centralised bureaucratic control,
funded entirely through general taxation, and with
all doctors employed as salaried staff. The ideology
was similarly one of egalitarianism, where the
stated Government policy was that every citizen
had the right to appropriate public healthcare when
sick. This spirit was eventually written into law, as
mentioned above, namely “no person should be
prevented, through lack of means, from obtaining
adequate medical treatment”.16
However, unlike the NHS with its framework
of General Practitioner gatekeeping, Hong Kong
did not have a well-developed public primary care
system. Instead, there existed a large private sector
in which patients typically paid out of pocket for
treatment. Under such a ‘dual system’, people could
afford private care for minor illnesses, while most
depended on the public system for hospital services.
Such a value system explains:
a. The vehement community opposition to even
a hint of linking public hospital charges to a
percentage of the cost.
b. The relative tolerance of the Government’s
decision to focus reform efforts solely on public
hospitals, rather than clinics, even though no
one would consider the services in Government
General Out-Patient Clinics to be any better.
c. The general sympathy for overworked hospital
staff, given that patients’ lives were at stake.
Stakeholders' interests
Any major reform has to address the interests of key
societal stakeholders. The state of affairs at the time
can be summarised as follows:
a. Public: While the majority of patients with severe
illnesses depended on the public sector for the
highly subsidised care, there was widespread
discontent over the poor state of public hospitals
in the early 1980s. Change for the better was, in
fact, long overdue.
b. Staff: Doctors and nurses in the system were
increasingly frustrated by overcrowding and
poor working environment. They deeply felt
the constraints of stifling bureaucracies, where
obvious problems were left unaddressed.
Manpower shortages worsened as experienced
staff left for the private sector in growing numbers.
c. Government: There was evidence that the
Government was equally concerned about
system-wide inefficiencies and the limited
management capabilities in the M&HD. At
the same time, while the Government was
increasingly funding the Subvented hospitals,
it felt it lacked a commensurate level of control
over their operations.
d. Subvented organisations: There was a strong
sense of second-class treatment among
Subvented hospitals, particularly in terms of staff
conditions, equipment, and funding compared
to Government hospitals. Any reform aimed at
levelling these disparities would be welcomed.
Although the respective boards of directors
feared losing autonomy under the new HA, such
concerns were outweighed by overwhelming staff
support for change.
e. Politicians: The interests of Legislative
Councillors largely coincided with those of
the public. Moreover, there were ‘functional
constituency’ legislators at the time, including
one seat for the Medical constituency (elected
by registered medical practitioners) and another
for the Health constituency (elected by other
healthcare professionals). There were also
appointed members with medical backgrounds.
Their expertise in the healthcare field often gave
them considerable influence in related debates.
f. Professional bodies: The Hong Kong Medical
Association was all along supportive of public
hospital reform, in light of the plight of public
doctors who formed a considerable part of its
membership.22 The same applied to nurses’
unions, particularly The Hong Kong Association
of Nursing Staff and the Nurses Branch of the
Hong Kong Chinese Civil Servants’ Association,
as well as other bodies such as the Association of
Hospital Administrators, Hong Kong.
g. Business sector: The business sector generally
welcomed any Government initiative to improve
public hospital services, viewing it as beneficial
for societal stability, economic development and
the health of the workforce. Moreover, a high-quality,
heavily subsidised public hospital service
would also indirectly benefit private businesses
by helping lower the premium of health insurance
they needed to provide for employees.
h. Private hospitals: Private hospitals only
constituted a small portion of the market share
for hospital services, as most people could not
afford private care and fewer than half of the
population had any meaningful private health
insurance cover at the time. These hospitals also
operated as separate entities without a united
front and thus did not exert much political
influence.23
Epilogue
As described above, the 6 years from the initial
conception to the formal establishment of the HA
were by no means straightforward and guaranteed.
Political determination by the Government was
paramount, while leadership from legislators,
community organisations and staff bodies was
also instrumental. Equally important, the buoyant
economy of Hong Kong at the time helped support
such bold reform, which predictably had major
resource implications. Be that as it may, this was only
the first step in the journey. Part 2 will describe how
the HA undertook the mammoth task of reforming
the public hospital system in its initial years, based
on the blueprint established thus far.
Declaration
The author declares full responsibility for the accuracy of the
content, which does not represent the views of the Hospital
Authority. Given the scale of the reform, not all aspects can
be covered in detail. Interested readers and scholars are
encouraged to consult the Hospital Authority’s publications
for further information.
Acknowledgement
This article series is based on an unfinished project from
the author’s time as a visiting fellow at the Harvard School
of Public Health, aiming to document both the history
and philosophy of the reform. The author is grateful to
two successive Presidents of the Hong Kong College of
Community Medicine, Dr Libby Lee and Dr Fei-chau Pang,
for encouraging its revival.
Notes
- The author was Chief Executive of the HA from 1999 to 2005. He was initially trained as a specialist in general surgery and worked in the former M&HD. Upon the establishment of the HA in 1991, he joined the HA Head Office to assist in the management transformation process, and thereafter worked in the operations team in various positions. He was appointed Hospital Chief Executive of Kwong Wah Hospital from 1995 to 1999, before being further promoted to head the entire organisation as Chief Executive.
- Hong Kong SAR Government. Secretary for Health deeply concerned about management of public healthcare system [press release]. 21 Jun 2024. Available from: https://www.info.gov.hk/gia/general/202406/21/P2024062100808.htm. Accessed 1 Sep 2025.
- Coopers & Lybrand WD Scott. The Delivery of Medical Services in Hospitals—A Report for the Hong Kong Government. Hong Kong: Hong Kong Government Printer; December 1985. Section 3.1.
- These hospitals, originally established as private institutions, became increasingly dependent on Government subvention for financial sustainability over time, hence the term ‘Subvented hospitals’.
- Coopers & Lybrand WD Scott. The Delivery of Medical Services in Hospitals—A Report for the Hong Kong Government. Hong Kong: Hong Kong Government Printer; December 1985. Appendix 3A.
- Coopers & Lybrand WD Scott. The Delivery of Medical Services in Hospitals—A Report for the Hong Kong Government. Hong Kong: Hong Kong Government Printer; December 1985. Appendix 3B.
- Ng A. Medical and health. In: Tsim TL, Luk BH, editors. The Other Hong Kong Report. Hong Kong: The Chinese University of Hong Kong Press; 1989.
- Hutcheon R. Bedside Manner: Hospital and Health Care in Hong Kong. Hong Kong: The Chinese University of Hong Kong Press; 1999: 34-42.
- National Health Service Management Inquiry. Griffiths Report. London: Department of Health and Social Security; 1983.
- Hutcheon R. Bedside Manner: Hospital and Health Care in Hong Kong. Hong Kong: The Chinese University of Hong Kong Press; 1999.
- Coopers & Lybrand WD Scott. The Delivery of Medical Services in Hospitals—A Report for the Hong Kong Government. Hong Kong: Hong Kong Government Printer; December 1985. Section 1.1.
- Official Report of Proceedings of the Hong Kong Legislative Council. Session held on 15 October 1986. Hong Kong: Legislative Council; 1986.
- The author was Vice Chairman of the Government Doctors’ Association in 1989 and actively took part in negotiations with the Government. He became Chairman in 1990-1991.
- Official Report of Proceedings of the Hong Kong Legislative Council. Session held on 8 March 1989. Hong Kong: Legislative Council; 1989.
- The main action that achieved the aim of embarrassing the Government without adversely affecting patient care was the refusal of public doctors to sign the payment slips for discharged patients, who were discharged anyway but without the need to pay up. The other actions—refusing to teach nursing students, attend non-urgent medical boards, and write non-urgent medical reports “because the doctors were too busy”—were essentially cosmetic, with little real impact during the short period.
- Hong Kong SAR Government. Hospital Authority Ordinance (Cap 113), Section 4(d). Hong Kong: Hong Kong Government Printer; 1990.
- Indeed, the HA was haunted years later by stipulations in the Employment Ordinance that certain staff unions claimed the organisation had violated, due to the long working hours of doctors—the subject of a lawsuit that lingered until 2006 over matters dating back to before 2000.
- The HA also promised to honour the traditions and philosophies of the parent organisations. Examples included service restrictions (such as abortion) in some religious hospitals, and the traditional Free Medical Service provided by the Tung Wah Group of Hospitals (TWGHs) for out-patients. With these concessions, the HA was able to reach agreement first with the TWGHs, which owned five hospitals. Once this was accomplished, the other subvented organisations soon followed suit.
- Following enactment of the HA Ordinance, these hospitals became known as Schedule 2 hospitals. Schedule 1 hospitals comprised all former Government hospitals previously under M&HD.
- Such a feat was rarely seen elsewhere. Singapore, for example, reformed its public hospitals one at a time.
- Tao J. Confucian care-based philosophical foundation of health care, In: Leung GM, Bacon-Shone J, editors. Hong Kong’s Health System: Reflections, Perspectives and Visions. Hong Kong: Hong Kong University Press; 2006: 41-60.
- The Association’s stance changed considerably a few years later, due to concerns that a “too successful” HA posed a threat to the business of its private sector members. It complained of an “unequal playing field” as the HA was able to offer services that were equal to, if not better than, those of the private sector, while being heavily subsidised by the Government. However, this was not foreseen at the time.
- The Hong Kong Private Hospitals Association was not established until as late as 2000.