Hong Kong Med J 2025;31:Epub 19 Sep 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Clinical and imaging patterns of child abuse in Hong Kong: a 10-year review from a tertiary centre
Catherine YM Young, MB, BS, FRCR1; CH Yiu1; Kathleen CH Tsoi, MB, ChB, MRCPCH2; Dorothy FY Chan, MB, ChB, FRCPCH2; Ki Wang, MB, BS, FRCR1; Winnie CW Chu, MB, ChB, MD1
1 Department of Imaging and Interventional Radiology, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong SAR, China
2 Department of Paediatrics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong SAR, China
Corresponding author: Dr Catherine YM Young (youngymc@connect.hku.hk)
Abstract
Introduction: Child abuse, a pressing medical and
social issue in Hong Kong, requires high vigilance
for prompt identification and early management.
The Mandatory Reporting of Child Abuse Ordinance
has recently been gazetted, establishing a mandatory
obligation for suspected injury reporting to protect
children’s rights. This study aimed to describe the
incidence and patterns of child abuse in Hong Kong
to draw attention to this key issue.
Methods: A retrospective review of all reported child
abuse cases admitted to Prince of Wales Hospital
over a 10-year period (2014-2023) was performed.
Results: In total, 503 cases of child abuse were
retrieved from the hospital’s electronic system,
revealing an increasing trend over the years. Of
these cases, 341 cases (67.8%) were attributed to
physical abuse. Most cases involved trivial soft
tissue injuries, apart from two limb fracture cases,
which represented 0.4% of all reported child abuse
cases (n=503) and 0.6% of all reported physical child
abuse cases (n=341). Abusive head trauma (n=3)
constituted 0.6% of all reported physical child abuse
cases and 0.9% of all reported child abuse cases.
Two cases of severe abusive head trauma required
paediatric intensive care, and one case warranting neurosurgical intervention subsequently exhibited
gross motor delay.
Conclusion: Most child abuse cases in Hong Kong
present with minor clinical manifestations. Imaging
evidence of skeletal or neurological injury is present
in a small proportion of patients. Abusive head injury
is uncommon but carries far-reaching consequences;
early recognition is essential to protect affected
children from further harm. Paediatric radiologists
play a pivotal role in making the diagnosis.
New knowledge added by this study
- Fractures resulting from non-accidental injury are less common in Hong Kong, which has a predominantly Chinese population, than in Western countries; the fracture patterns differ.
- The overall incidence of abusive head trauma is low; however, a substantial proportion of patients with non-accidental injury who undergo further neuroimaging display positive findings.
- Interpretation of plain radiographs in cases of non-accidental injury should not solely rely on classical textbook fracture patterns; correlations with a compatible clinical history are particularly important.
- Neuroimaging is essential for children under 1 year of age with clinical suspicion of non-accidental injury, particularly those showing abnormal neurological signs, to detect abusive head trauma.
Introduction
Child abuse is a prevalent yet frequently overlooked
condition in paediatric patients worldwide, affecting
between 4% and 16% of the paediatric population.1
It may manifest as physical abuse, neglect, sexual
abuse, or psychological abuse,2 all of which carry
substantial long-term medical and psychological
consequences. Clinical presentation is often vague,
requiring a high degree of clinical suspicion by both clinicians and radiologists to ensure early activation
of child protection services. Multidisciplinary input
is needed for timely intervention and prevention of
recurrence.
While clinical evaluation is crucial for
identifying apparent or superficial injuries,
radiological imaging also plays a vital role in detecting
old or clinically occult injuries. John Caffey, a
paediatric radiologist, was among the first to describe the association between long bone fractures and
chronic subdural haematoma in infants, introducing
the concept of non-accidental injury.3 Since then, a
growing body of literature has emerged concerning
the radiological features of non-accidental injury,
contributing to increased global awareness. Various
guidelines have also been developed, including
those by The Royal College of Radiologists4 and the
American College of Radiology,5 which recommend
appropriate imaging modalities in suspected cases to
protect children’s welfare while balancing the risks of
radiation exposure.
Various retrospective studies in Western
populations have examined the epidemiology, injury
patterns, and outcomes of non-accidental paediatric
injuries in their respective regions6 7 8 9; however,
limited research has been conducted in Asia,
particularly within Hong Kong. This study aimed to
describe the incidence, clinical presentation, imaging
features, and treatment outcomes of child abuse in
a tertiary regional hospital in Hong Kong, with the
goal of raising awareness towards this commonly
overlooked condition.
Methods
This retrospective study included all reported cases
of child abuse involving paediatric patients (aged
0-18 years) admitted to Prince of Wales Hospital,
a tertiary regional hospital in Hong Kong, over a 10-year period (from January 2014 to December
2023). All suspected or confirmed cases of child
abuse were identified from the Clinical Data Analysis
and Reporting System, an electronic health registry
managed by the Hospital Authority of Hong Kong.
The search utilised key terms under the International
Classification of Diseases, Ninth Revision coding,
including “Child maltreatment syndrome”, “Child
and adult battering and other maltreatment”, “Child
abuse”, and “Child maltreatment syndrome, shaken
infant syndrome”. Clinical records of all reported
cases were reviewed. Cases were excluded if they
were inappropriately categorised (aged >18 years),
erroneously reported as unrelated to child abuse, or
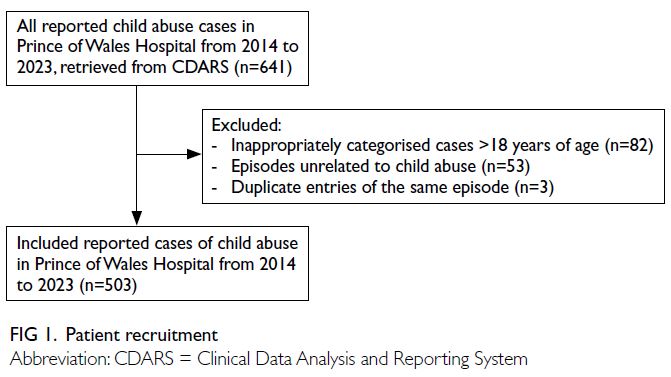
duplicate entries of the same episode (Fig 1).
Clinical data including patient demographics
(age at presentation and sex), clinical presentation,
type of abuse, imaging performed, multidisciplinary
case conferences (MDCCs) held, management
strategies, and any long-term adverse outcomes
were reviewed from electronic patient records and
case notes. Relevant imaging studies were reviewed
by the primary investigator (5 years of radiology
experience) and cross-checked against the original
reports. In cases of discrepancy, images were re-interpreted
through consensus reading with an
experienced paediatric radiologist (20 years of
radiology experience).
Results
Patient demographics and clinical
presentation
In total, 503 reported cases of child abuse were
included in the study. The number of reported cases
showed an upward trend over the 10-year period,
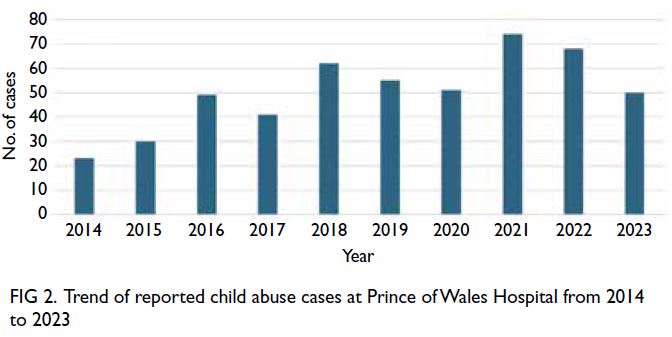
from 23 cases in 2014 to 50 cases in 2023 (Fig 2).
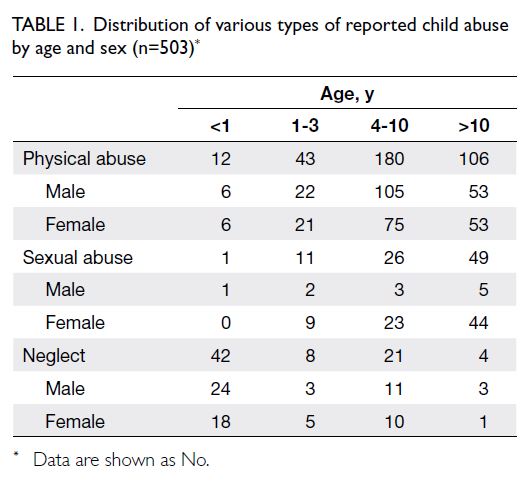
The case distribution is presented in Table 1.
The cohort comprised 265 (52.7%) girls and 238
(47.3%) boys. The mean age was 8.25 years (range,
0-17), with 55 cases (10.9%) involving infants
under 1 year of age. Physical abuse was the most
common type at presentation, accounting for 341
cases (67.8%). The vast majority (>99%) of patients
presented with erythematous marks, bruises, or
lacerations. Other presenting symptoms included
seizures, loss of consciousness, and vomiting. Sexual
abuse was the second most common type (n=87,
17.3%), followed by child neglect (n=75, 14.9%).
More than half of the cases (n=263, 52.3%)
were admitted via the Accident and Emergency
(A&E) Department. The vast majority of these
patients presented directly to our hospital, and only
two transferred from adjacent acute hospitals—one involving abusive head trauma requiring
neurosurgical intervention, and another with a
suspected vaginal tear necessitating input from
obstetricians and gynaecologists. Most of these patients (254 cases, 96.6%) were referred due to
clinical suspicion of abuse raised by non-offending
parents (n=137), social workers (n=78), the patients
themselves (n=22), or witnesses (n=17). In the
remaining nine cases (3.4%), suspicion was first
raised by medical staff either in the Emergency
Department/General Outpatient Clinic (n=4) or after
admission (n=5). Although medical staff identified a
relatively small proportion of these cases, many were
severe, including three abusive head trauma cases
initially presenting with seizures. In such cases,
abuse was only suspected after imaging.
The remaining 240 cases (47.7%) were admitted
through other channels, including referral by social
workers (n=203), neonatal admission (n=28),
abnormalities identified by medical staff during
follow-up or screening (n=8), and sibling screening
(n=1).
Imaging modalities and findings
Imaging was performed for 100 patients (19.9%),
including 86 cases with skeletal imaging, 24 with
neurological imaging, and one with abdominal
imaging. Among the 24 patients who underwent
neuroimaging, 10 also had skeletal imaging, while 14
received neuroimaging only.
Of the 86 patients who underwent skeletal
imaging, 77 had plain radiographs of the targeted
region as initial screening, and nine received a
complete skeletal survey. Most patients had minor
soft tissue injuries. Fractures were identified in
two patients: a supracondylar fracture in a 3-year-old
boy and a foot fracture in a 13-year-old girl,
representing 2.3% of all skeletal imaging cases
(Fig 3). Both fractures were detected on dedicated
radiographs directed at regions of pain, as indicated
by the patients. In another case, initial radiographs
in a 13-year-old boy showed no obvious fracture, but
magnetic resonance imaging (MRI) for persistent
wrist pain subsequently revealed a mild ligamentous
sprain.

Figure 3. (a) Anteroposterior plain radiograph of the right elbow showing a linear transverse supracondylar fracture of the right humerus (arrow). (b) Anteroposterior plain radiograph of the left fifth toe showing cortical buckling over the lateral aspect of the shaft of the left fifth metatarsal bone (arrow)
Computed tomography (CT) was the
initial imaging modality in 24 cases evaluated for
suspected intracranial injury; five cases (20.8%)
showed positive findings. Three cases (12.5%)
demonstrated alarming features suggestive of shaken
baby syndrome on initial brain CT scans, including
subdural haemorrhage (n=3) and cerebral oedema
(n=1), prompting further evaluation by MRI. Shaken
baby syndrome was confirmed in all three cases on
MRI, which showed subdural haemorrhage (n=3)
and brain parenchymal injuries, including diffuse
axonal injury (n=3) and hypoxic-ischaemic injury
(n=2) [Fig 4]. These patients, aged between 2 and
7 months, presented with non-specific symptoms
such as seizures (n=3), vomiting (n=2), and loss of
consciousness (n=1). Fundoscopic examination
confirmed multilayered retinal haemorrhages in all three cases, whereas skeletal surveys were
unremarkable (Table 2). The remaining two CT-positive
cases included one with a scalp haematoma
and another with a mildly depressed parietal skull
fracture; both lacked intracranial findings.
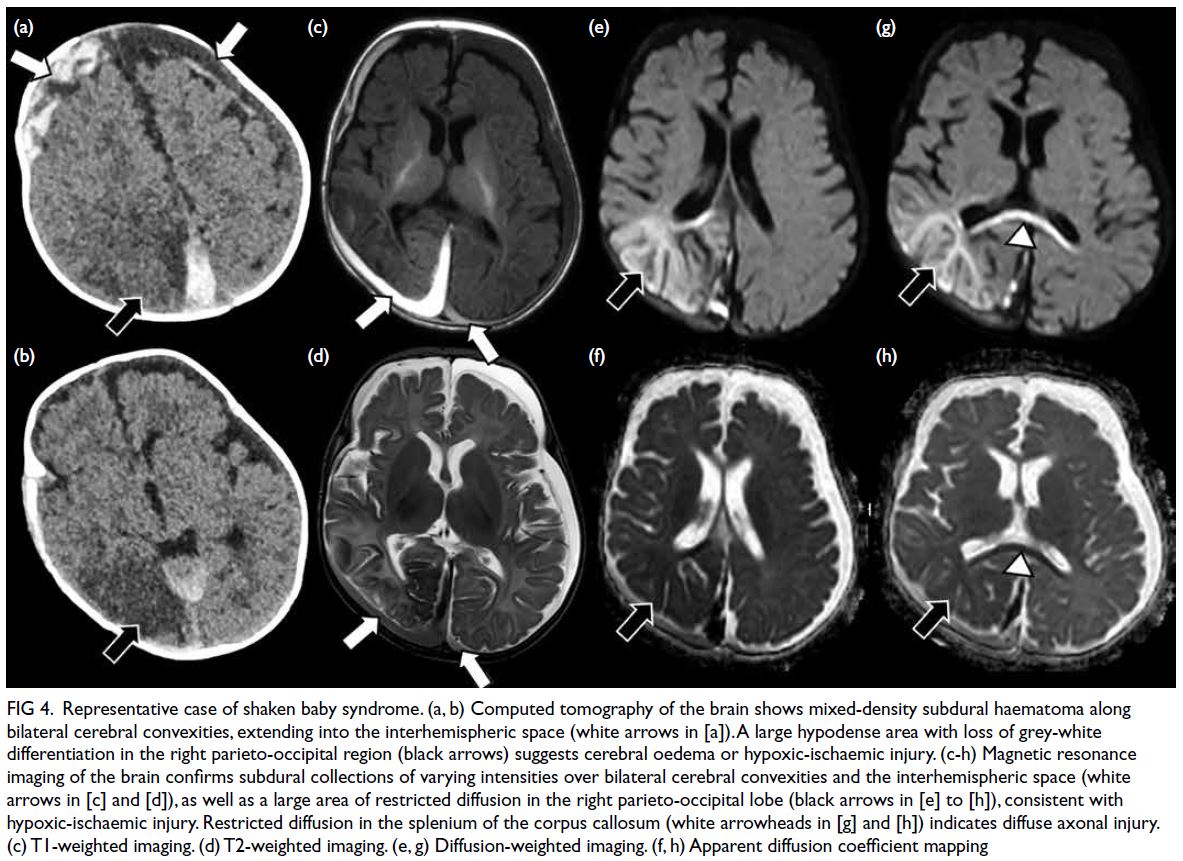
Figure 4. Representative case of shaken baby syndrome. (a, b) Computed tomography of the brain shows mixed-density subdural haematoma along bilateral cerebral convexities, extending into the interhemispheric space (white arrows in [a]). A large hypodense area with loss of grey-white differentiation in the right parieto-occipital region (black arrows) suggests cerebral oedema or hypoxic-ischaemic injury. (c-h) Magnetic resonance imaging of the brain confirms subdural collections of varying intensities over bilateral cerebral convexities and the interhemispheric space (white arrows in [c] and [d]), as well as a large area of restricted diffusion in the right parieto-occipital lobe (black arrows in [e] to [h]), consistent with hypoxic-ischaemic injury. Restricted diffusion in the splenium of the corpus callosum (white arrowheads in [g] and [h]) indicates diffuse axonal injury. (c) T1-weighted imaging. (d) T2-weighted imaging. (e, g) Diffusion-weighted imaging. (f, h) Apparent diffusion coefficient mapping
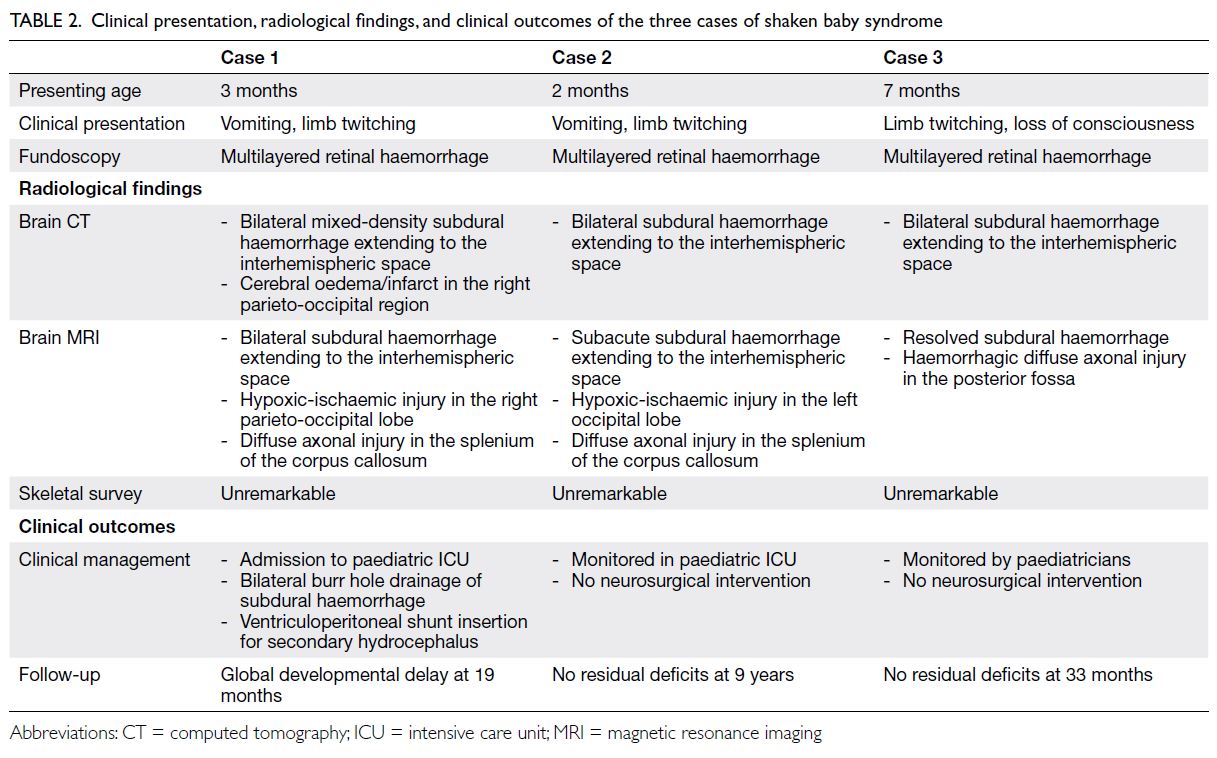
Table 2. Clinical presentation, radiological findings, and clinical outcomes of the three cases of shaken baby syndrome
Ultrasound of the abdomen and pelvis was
performed in one patient with persistent abdominal
pain; no clinically significant solid organ injury was
identified.
Multidisciplinary case conference assessment
and long-term adverse outcomes
Overall, 44 cases (8.7%) were dismissed for various
reasons, such as cross-border status, family
refusal, or discharge against medical advice. Of the
remaining 459 cases (91.3%) evaluated by MDCC,
documentation was not retrievable from clinical
records in 45 cases (8.9%).
Among the 414 cases with available MDCC
documentation or conclusions, child abuse was
confirmed in 199 cases (48.1%), comprising physical
abuse (n=95), child neglect (n=63), and sexual abuse
(n=41). Another 84 cases (20.3%) were categorised
as high-risk, involving suspected physical abuse
(n=81) or sexual abuse (n=3). Child abuse was not
established in the remaining 131 cases (31.6%); these
were considered to have low or moderate risk of
recurrence.
Of the 89 cases in which MDCC was dismissed
or notes were unavailable, more than half (n=63,
70.8%) had presented with suspected physical abuse,
followed by sexual abuse (n=22, 24.7%) and neglect
(n=4, 4.5%). All cases were deemed minor, with
no clinically or radiologically significant findings.
No specific treatment or long-term follow-up was
required.
The majority of cases exhibited minor severity
and were managed conservatively without long-term
adverse outcomes.
A long arm cast was applied for one patient
with a supracondylar fracture, whereas a resting
splint was prescribed for another patient with a
ligamentous wrist sprain. Both patients recovered
uneventfully after short-term follow-up (1 year) by
the orthopaedics team, with no residual impact on
daily functioning.
Two patients with severe abusive head
trauma required admission to the paediatric
intensive care unit. One of these patients warranted
multiple neurosurgical interventions, including
bilateral burr hole drainage and placement of a
ventriculoperitoneal shunt. The remaining two cases
of abusive head trauma were managed conservatively.
At the most recent follow-up, one patient—the most severely affected—demonstrated gross motor delay
at 19 months of age. All other patients showed no
neurological deficits or developmental delay to date.
No mortality was recorded in this cohort.
Repeated admissions for suspected child
abuse were identified in 22 cases. Of these, 16 were
recurrent, established cases of child abuse. In 14 of
these 16 cases, the type of abuse remained consistent
across episodes, whereas two cases involved different
types of abuse in separate incidents. Four cases
were initially classified as established child abuse,
but subsequent admissions were considered non-established,
with recurrence risk ranging from low to
high. Two cases were categorised as non-established
child abuse on both occasions but were considered
to have moderate or high risk of recurrence.
Discussion
This retrospective 10-year study documented a
significant rise in reported child maltreatment cases,
emphasising that child abuse remains an ongoing
medical and social concern. This issue persists
despite concerted efforts by the government and
various organisations to provide social support
to new mothers and at-risk families in an effort to
prevent child maltreatment.
Types of child abuse
Physical abuse was the most common type of
presentation in our study, consistent with data
from the Child Protection Registry10 and similar
findings from Singapore.11 The high prevalence of
physical abuse in Hong Kong may reflect cultural
differences in parenting practices, such that corporal
punishment remains more commonly accepted in
Chinese households than in Western contexts.12
Over 50% of families in Hong Kong use physical
punishment as part of child-rearing.13 In moments of
anger or impulsiveness, the line between ineffective
parenting and child abuse may easily be crossed.
Pattern of injury and imaging findings
The majority of cases in our study were considered mild in nature, with no serious long-term
consequences after clinical evaluation and
appropriate imaging. Fractures were infrequent,
comprising 0.4% of all reported child abuse cases
and 0.6% of all reported physical child abuse cases.
These rates are slightly lower than those reported in
previous Asian studies, which revealed fractures in
1% of all reported physical child abuse cases11 and
3.6% to 7% of all reported child abuse cases.14 15 The
present rates are substantially lower than the 28%
observed in a Western population.6 The fracture
detection rate among patients who underwent
imaging in our study (2.3%) was also considerably
lower than that in Western populations (24%-32%).7 8 Compared with a previous Hong Kong
study in 2005,15 our findings suggest a decline in
the overall fracture rate despite an overall increase
in reported child maltreatment cases, implying a
trend towards milder injuries in recent years. This
trend may reflect increased societal awareness of
the consequences of severe child abuse, potentially
leading parents to move away from traditional
forms of physical punishment (eg, caning) and
towards less injurious methods, such as striking
with the hand. Greater awareness may also facilitate
earlier detection and reporting, thereby preventing
escalation.
No fractures were identified on skeletal surveys
in the few cases of confirmed shaken baby syndrome
in our cohort. One case of parietal bone fracture
was documented—the parietal bone is among the
most commonly fractured skull bones, according
to current literature.14 16 The other identified
fractures—supracondylar and foot fractures—do
not reflect the classical abuse-specific fracture types
described in the literature, such as posteromedial
rib fractures or metaphyseal corner fractures.16
However, these findings align with previous studies
in Singapore, where the humerus was the most
frequently fractured bone.11 14 Our results also differ
from the findings of Fong et al,15 who reported that
forearm and rib fractures were most common in Hong Kong. With the exception of rib fractures, the
sites noted in our study are not typically associated
with non-accidental injury. This highlights potential
differences in injury severity and fracture patterns
between Asian and Western populations and
underscores the importance of maintaining clinical
suspicion for non-accidental injury, even in the
absence of classical fracture sites or textbook
imaging findings.16
Abusive head trauma is the leading cause of
morbidity and mortality among children subjected
to abuse, with an estimated morbidity rate of up to
80% and a mortality rate ranging from 15% to 30%.17 18
Despite the deceptively low overall occurrence
of abusive head trauma in our study (0.6% of all
reported physical child abuse cases and 0.9% of all
reported child abuse cases), compared with Western
counterparts (up to 40%-50%),6 9 it is notable that
20.8% of our imaged cases showed positive findings,
and shaken baby syndrome was confirmed in 12.5%
via MRI. All confirmed cases involved infants under
1 year of age, whose relatively oedematous brains,
immature intracranial vasculature, and poor neck
muscle control render them more susceptible to
the effects of abusive head trauma.19 It is therefore
imperative that neuroimaging be performed for all
children under 1 year of age with suspected non-accidental
injury, particularly those with abnormal
neurological signs, such as seizures or coma.4 Bilateral
subdural haemorrhages of varying densities, focal and
diffuse brain parenchymal injuries (eg, diffuse axonal
injury or cerebral oedema), and multilayered retinal
haemorrhages on fundoscopy, as demonstrated in
our study, are consistent with cardinal features of
abusive head trauma described in the literature.17 20
Our study also revealed more favourable morbidity
(33%) and mortality (0%) outcomes compared with
current literature reports,2 17 possibly due to the
relatively small number of cases.
Current practice in the management of cases
of suspected child abuse
At present, suspected child maltreatment presents
to our hospital via two main pathways: attendance
at the A&E Department for suspicious injuries,
and referral by social workers who observe unusual
behaviour or injuries.21 For cases requiring inpatient
care, the paediatric team conducts history taking and
physical examination, documents findings (including
clinical photographs), and manages the injuries.21
Relevant parties—such as social workers, clinical
psychologists, and police officers—are informed
as necessary.21 Minor cases may be assessed and
discharged directly from the A&E Department.21
An MDCC is typically convened within 10 days of
presentation, involving doctors, social workers,
school personnel, clinical psychologists, and police
officers to determine the nature of the incident, assess the risk of future maltreatment, and recommend
preventive measures.21
Radiologists play an active role in the
multidisciplinary management of child abuse—not
only in assessing the full extent of injuries but also
in detecting subtle, suspicious findings, alerting the
clinical team, and proactively contributing to early
intervention and the reduction of long-term adverse
outcomes. The reporting of suspicious injuries is
currently conducted on a voluntary basis, guided
by recommendations from the Social Welfare
Department.22 However, the recently gazetted
Mandatory Reporting of Child Abuse Ordinance,23
which becomes effective in January 2026, will
impose a legal obligation on professionals to report
suspected injuries, thereby strengthening safeguards
for children.
Strengths and limitations
To the best of our knowledge, this is the largest
retrospective study to investigate the clinical and
radiological features of child abuse in a regional
hospital in Hong Kong over the past decade. It
provides an updated local overview while drawing
comparisons with Western data to highlight
distinguishing features and emphasise the need for
greater attention to this critical issue.
This study had several limitations. First, it
was a retrospective analysis based on voluntarily
reported cases, and some instances of child abuse
may have been under-recognised or underreported
by attending clinicians. A small number of cases
also lacked accessible MDCC notes or conclusions
due to record loss over time. Second, our dataset
includes only admitted cases from a single regional
hospital, which may have introduced selection bias
because minor cases discharged directly from A&E
were excluded. The generalisability of our findings
is limited, given that the distribution of child
maltreatment cases varies substantially across Hong
Kong districts. Sha Tin accounted for approximately
6.2% of all reported child maltreatment cases from
2014 to 2023, whereas Yuen Long accounted of 12%.24
Variations in demographic and socio-economic
backgrounds across districts may also influence
clinical presentation and severity of injuries; further
investigation is warranted. Third, despite the large
cohort of child abuse cases included in our series,
the proportion of positive imaging findings remains
relatively small. Larger-scale studies are needed
to better characterise local injury patterns. Finally,
due to the extended retrospective recruitment
period, follow-up durations varied widely—from 15 months in recent cases to 9 years in earlier cases.
Consequently, the long-term effects of abusive head
trauma may not yet be evident in patients with
shorter follow-up, highlighting the need for further
longitudinal assessment into later childhood.
Conclusion
This study provides an updated overview of the
clinical and radiological features of child abuse
in Hong Kong, revealing patterns that differ
from those described in Western literature.
Although most cases involved only minor clinical
manifestations, a small proportion of patients
exhibited positive imaging findings of skeletal or
neurological injury, which may carry serious long-term
consequences. Radiologists play a critical role
in the multidisciplinary management of child abuse,
both in flagging suspicious injuries to alert clinicians
and in evaluating the full extent of trauma to protect
children from further harm.
Author contributions
Concept or design: CYM Young, WCW Chu.
Acquisition of data: All authors.
Analysis or interpretation of data: CYM Young, WCW Chu.
Drafting of the manuscript: CYM Young.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: CYM Young, WCW Chu.
Drafting of the manuscript: CYM Young.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research was conducted in accordance with the
Declaration of Helsinki. Ethics approval was obtained from
the Joint Chinese University of Hong Kong–New Territories
East Cluster Clinical Research Ethics Committee, Hong Kong
(Ref No.: 2024.071). The requirement for informed patient
consent was waived by the Committee due to the retrospective
design of the research.
References
1. Gilbert R, Widom CS, Browne K, Fergusson D, Webb E,
Janson S. Burden and consequences of child maltreatment
in high-income countries. Lancet 2009;373:68-81. Crossref
2. Guastaferro K, Shipe SL. Child maltreatment types by
age: implications for prevention. Int J Environ Res Public
Health 2023;21:20. Crossref
3. Caffey J. Multiple fractures in the long bones of infants
suffering from chronic subdural hematoma. Am J
Roentgenol Radium Ther 1946;56:163-73.
4. The Society and College of Radiographers; The Royal
College of Radiologists. The Radiological Investigation
of Suspected Physical Abuse in Children (Revised First
Edition). London: The Royal College of Radiologists; 2018.
Available from: https://www.rcr.ac.uk/media/nznl1mv4/rcr-publications_the-radiological-investigation-of-suspected-physical-abuse-in-children-revised-first-edition_november-2018.pdf. Accessed 1 Oct 2024.
5. Wootton-Gorges SL, Soares BP, Alazraki AL, et al. ACR
Appropriateness Criteria® suspected physical abuse—child. J Am Coll Radiol 2017;14:S338-49. Crossref
6. Ward A, Iocono JA, Brown S, Ashley P, Draus JM Jr. Non-accidental
trauma injury patterns and outcomes: a single
institutional experience. Am Surg 2015;81:835-8. Crossref
7. Day F, Clegg S, McPhillips M, Mok J. A retrospective case
series of skeletal surveys in children with suspected non-accidental
injury. J Clin Forensic Med 2006;13:55-9. Crossref
8. Loos MH, Ahmed T, Bakx R, van Rijn RR. Prevalence
and distribution of occult fractures on skeletal surveys in
children with suspected non-accidental trauma imaged
or reviewed in a tertiary Dutch hospital. Pediatr Surg Int
2020;36:1009-17. Crossref
9. Rosenfeld EH, Johnson B, Wesson DE, Shah SR, Vogel AM,
Naik-Mathuria B. Understanding non-accidental trauma
in the United States: a national trauma databank study. J
Pediatr Surg 2020;55:693-7. Crossref
10. Social Welfare Department, Hong Kong SAR Government.
Child Protection Registry Statistical Report 2023. 2024.
Available from: https://www.swd.gov.hk/storage/asset/section/654/Annual%20CPR%20Report%202023_Biligual_Final.pdf . Accessed 1 Oct 2024.
11. Chew YR, Cheng MH, Goh MC, Shen L, Wong PC,
Ganapathy S. Five-year review of patients presenting with
non-accidental injury to a children’s emergency unit in
Singapore. Ann Acad Med Singap 2018;47:413-9. Crossref
12. Liu W, Guo S, Qiu G, Zhang SX. Corporal punishment
and adolescent aggression: an examination of multiple
intervening mechanisms and the moderating effects of
parental responsiveness and demandingness. Child Abuse
Negl 2021;115:105027. Crossref
13. Tang CS. Corporal punishment and physical maltreatment
against children: a community study on Chinese parents in
Hong Kong. Child Abuse Negl 2006;30:893-907. Crossref
14. Gera SK, Raveendran R, Mahadev A. Pattern of fractures
in non-accidental injuries in the pediatric population in
Singapore. Clin Orthop Surg 2014;6:432-8. Crossref
15. Fong CM, Cheung HM, Lau PY. Fractures associated with
non-accidental injury—an orthopaedic perspective in a local regional hospital. Hong Kong Med J 2005;11:445-51.
16. Offiah A, van Rijn RR, Perez-Rossello JM, Kleinman PK.
Skeletal imaging of child abuse (non-accidental injury).
Pediatr Radiol 2009;39:461-70. Crossref
17. Sidpra J, Chhabda S, Oates AJ, Bhatia A, Blaser SI, Mankad K.
Abusive head trauma: neuroimaging mimics and diagnostic
complexities. Pediatr Radiol 2021;51:947-65. Crossref
18. Karibe H, Kameyama M, Hayashi T, Narisawa A, Tominaga T.
Acute subdural hematoma in infants with abusive head
trauma: a literature review. Neurol Med Chir (Tokyo)
2016;56:264-73. Crossref
19. Hung KL. Pediatric abusive head trauma. Biomed J
2020;43:240-50. Crossref
20. Sun DT, Zhu XL, Poon WS. Non-accidental subdural
haemorrhage in Hong Kong: incidence, clinical features,
management and outcome. Childs Nerv Syst 2006;22:593-8. Crossref
21. So EC, Chan D. Management of Child Maltreatment
(Abuse). Hong Kong: Hospital Authority New Territories
East Cluster Prince of Wales Hospital Department of
Paediatrics; 2024.
22. Social Welfare Department, Hong Kong SAR Government.
Protecting Children from Maltreatment Procedural
Guide for Multi-disciplinary Co-operation (Revised
2020). Jan 2020. Available from: https://www.swd.gov.hk/storage/asset/section/652/en/Procedural_Guide_Core_Procedures_(Revised_2020)_Eng_2Nov2021.pdf . Accessed 1 Oct 2024.
23. Legislative Council, Hong Kong SAR Government.
Mandatory Reporting of Child Abuse Ordinance. 2024.
Available from: https://www.legco.gov.hk/yr2024/english/ord/2024ord023-e.pdf. Accessed 29 Oct 2024.
24. Social Welfare Department, Hong Kong SAR Government.
Statistics on child protection, spouse/cohabitant battering
and sexual violence cases captured by the Child Protection
Registry (CPR) and the Central Information System on
Spouse/Cohabitant Battering Cases and Sexual Violence
Cases (CISSCBSV). Social Welfare Department; 2025.
Available from: https://data.gov.hk/en-data/dataset/hk-swd-fcw-ca-scb-sv-stat/resource/6229e2b4-73d0-4285-a892-838c683c9966. Accessed 8 Aug 2025.