Hong Kong Med J 2025;31:Epub 4 Aug 2025
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Primary cervical intradural extramedullary
malignant melanoma: a case report
Long Tang, MMed1 #; Huiyi Liu, MMed1 #; Jiazhuang Zheng, MMed1; Fandong Wang, MMed1; Miao Wang, MMed1; Yong Zhou, MMed1; Ming Chen, MMed2; Jiao He, MMed3; Yu Chen, MMed1
1 Department of Spine Surgery, Suining Central Hospital, Suining, China
2 Department of Radiology, Suining Traditional Chinese Medicine Hospital, Suining, China
3 Department of Pathology, Suining Central Hospital, Suining, China
# Equal contribution
Corresponding author: Prof Yu Chen (yuspine@126.com)
Case presentation
A 47-year-old Chinese man presented with a 6-month
history of neck pain, numbness and weakness in the
left limb. In January 2019, he was admitted to the
Department of Spine Surgery at our institution. His
medical and family histories were unremarkable,
with no prior interventions.
Neurological examination revealed deficits
involving three levels of the left upper limb. Magnetic
resonance imaging (MRI) revealed an extramedullary
lesion at the C2-C3 level (Fig 1a to c). Following
ophthalmological and dermatological assessments
(including oral mucosa, external genitalia, and
anus), a primary intradural extramedullary
malignant melanoma (MM) was suspected. Surgical
intervention was indicated to improve neurological
function.
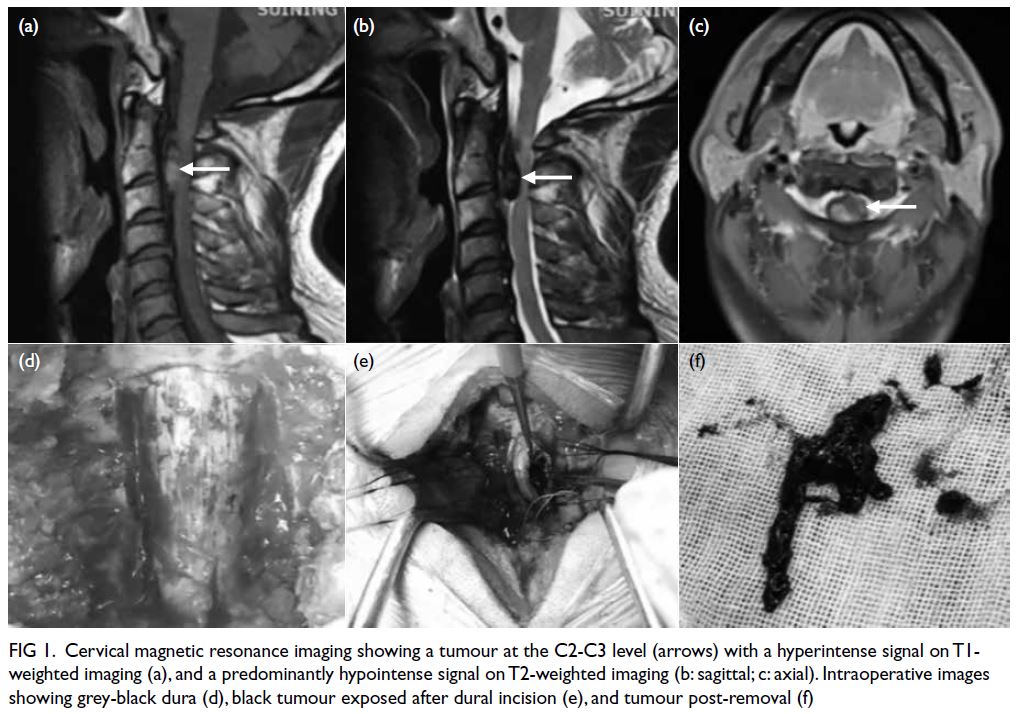
Figure 1. Cervical magnetic resonance imaging showing a tumour at the C2-C3 level (arrows) with a hyperintense signal on T1-weighted imaging (a), and a predominantly hypointense signal on T2-weighted imaging (b: sagittal; c: axial). Intraoperative images showing grey-black dura (d), black tumour exposed after dural incision (e), and tumour post-removal (f)
Although the tumour was in the left anterior
cervical cord, its position posterior to the C2-C3
vertebral body and spindle-shaped appearance
made anterior surgery less favourable, as resection
of the vertebral body to access the tumour and
reconstruction following removal would increase
surgical trauma and risk. After discussing the risks
and benefits with the patient and his family, informed
consent was obtained prior to surgery.
The patient underwent posterior surgery under
general anaesthesia with neuroelectrophysiological
monitoring. A C2-C4 laminectomy was performed
to expose the tumour, which was located on the left
anterior side of the cord. The lesion was compressing
and adherent to the spinal cord and dura. Using a
nerve retractor and with stable intraoperative
neuromonitoring, the tumour was carefully dissected
and completely excised (Fig 1d to f). The dura was
sutured and the laminae were re-implanted using
titanium mini-plates. A drainage tube was placed,
and the incision was carefully sutured.
Postoperative cervical MRI confirmed complete
tumour resection (Fig 2a to c). Histopathological
examination (Fig 2d to f) confirmed MM with
positive staining for HMB-45 (+), S-100 (+), and a Ki-67 index of 5%.
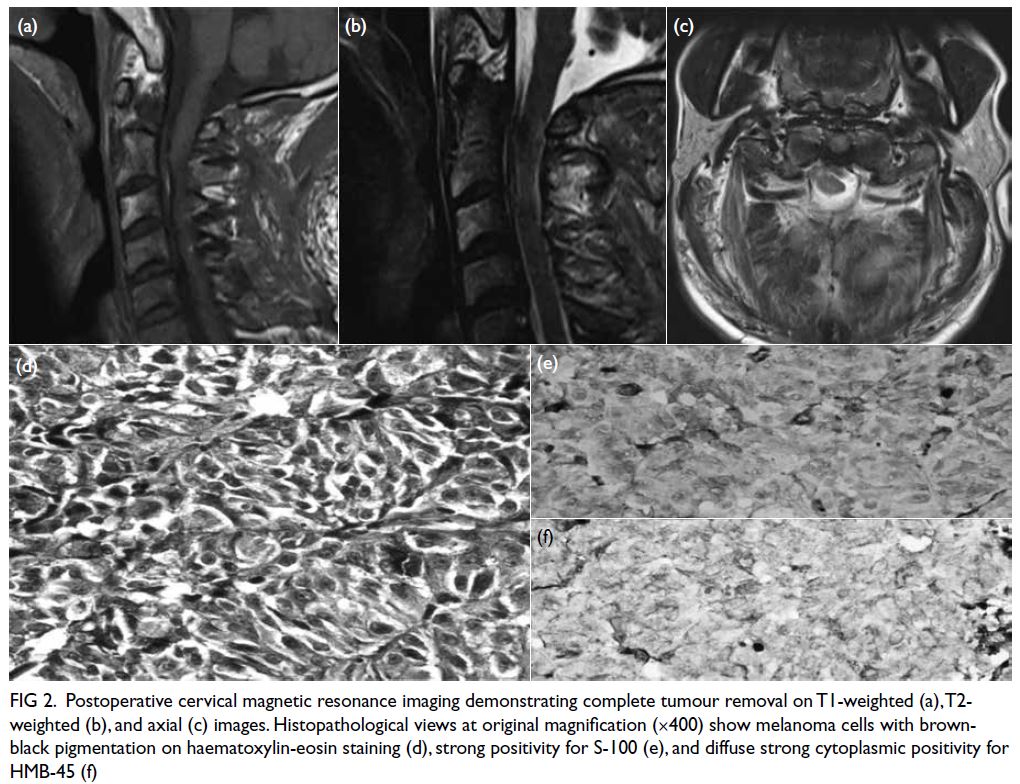
Figure 2. Postoperative cervical magnetic resonance imaging demonstrating complete tumour removal on T1-weighted (a), T2-weighted (b), and axial (c) images. Histopathological views at original magnification (×400) show melanoma cells with brownblack pigmentation on haematoxylin-eosin staining (d), strong positivity for S-100 (e), and diffuse strong cytoplasmic positivity for HMB-45 (f)
The patient underwent postoperative
rehabilitation and reported good neurological
recovery at the 5-year follow-up, with minimal
assistance required for certain left upper limb
movements. Given the favourable outcome, the
patient declined adjuvant radiochemotherapy as
recommended by our team. He continues to lead a
relatively active and independent life.
Discussion
Malignant melanoma of the spinal region is rare
and may present as either a primary or metastatic
lesion, with primary cases being exceptionally
uncommon.1 Primary spinal MM most frequently
affects the middle and lower thoracic spine, with
rare involvement of the cervical region.2 This is the
first case of primary intradural extramedullary MM
treated in our department in recent decades. Despite
the tumour being located in the upper cervical
region, satisfactory clinical outcomes were achieved.
Although MRI is the recommended and
effective preoperative imaging modality to
diagnose spinal MM, distinguishing it from
other pigmented central nervous system
tumours, such as leptomeningeal melanoma or
melanocytoma,3 can be challenging. A definitive
diagnosis relies on histopathological confirmation.
Immunohistochemical staining using antimelanoma
markers such as HMB-45 and S-100 can help confirm
the diagnosis.2 In our case, positive staining for both
HMB-45 and S-100 was conclusively confirmed.
There are currently no established guidelines for
the treatment of spinal MM, but complete surgical
removal is typically recommended.4 In our case, the
chief surgeon carefully removed the tumour starting
on the left side and gradually accessed the anterior
spinal cord. Complete resection was successfully
achieved without damage to the spinal cord or nerve
roots. It has been reported that patients may achieve
better outcomes and prognosis with postoperative
adjuvant radiotherapy and chemotherapy.5 In our case, the patient was enjoying a relatively good life
at the 5-year follow-up without adjuvant therapy,
indicating the importance of complete resection
and consistent with the literature. However, the
importance of radiotherapy or chemotherapy should
not be ruled out as further follow-up is necessary to
assess the final prognosis. Our team still recommends
that postoperative radiotherapy or chemotherapy be
routinely performed to improve patient outcomes.
Our research team reports a rare case of
primary intradural extramedullary MM at the C2-C3
level with successful surgery. First, complete tumour
resection is crucial for improving patient prognosis
and survival, emphasising the need for careful
consideration during treatment planning. Second,
proper handling of the anatomical relationship
between the tumour and the spinal cord or nerve roots
is essential to remove the tumour as completely as
possible while minimising neurological injury. Third,
although our patient declined adjuvant therapy and
achieved a favourable outcome at the 5-year follow-up,
we continue to recommend routine postoperative
radiotherapy or chemotherapy to improve prognosis.
A key limitation of this case is the absence of
radiological imaging at final follow-up, as the patient
declined hospital visits due to perceived symptom
improvement, which limits our ability to definitively
exclude indolent recurrence. Our case provides
valuable clinical insights, and long-term follow-up
remains essential for monitoring outcomes.
Author contributions
Concept or design: L Tang, Y Chen.
Acquisition of data: L Tang, H Liu, M Wang, Y Zhou.
Analysis or interpretation of data: L Tang, Y Chen, J He, M Chen.
Drafting of the manuscript: L Tang, H Liu.
Critical revision of the manuscript for important intellectual content: Y Chen, J Zheng, F Wang.
Acquisition of data: L Tang, H Liu, M Wang, Y Zhou.
Analysis or interpretation of data: L Tang, Y Chen, J He, M Chen.
Drafting of the manuscript: L Tang, H Liu.
Critical revision of the manuscript for important intellectual content: Y Chen, J Zheng, F Wang.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors are grateful to the clinical staff of the Department
of Spine Surgery at Suining Central Hospital for their
assistance in completing this article. The authors also thank
Bullet Edits Limited for providing language editing and
proofreading services.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study was approved by Suining Central Hospital's Ethics
Committee for Biomedical Research Involving Human Beings,
China (Ref No.: KYLLMC20240019). Written informed
consent was obtained from the patient for the publication of
this case report.
References
1. Hastings-James R. Melanoma of the central nervous system. Radiology 1973;109:357-60. Crossref
2. Lee CH, Moon KY, Chung CK, et al. Primary intradural
extramedullary melanoma of the cervical spinal cord: case
report. Spine (Phila Pa 1976) 2010;35:E303-7. Crossref
3. Smith AB, Rushing EJ, Smirniotopoulos JG. Pigmented
lesions of the central nervous system: radiologic-pathologic
correlation. Radiographics 2009;29:1503-24. Crossref
4. Nakamae T, Kamei N, Tanaka N, et al. Primary spinal cord
melanoma: a two-case report and literature review. Spine
Surg Relat Res 2022;6:717-20. Crossref
5. Kim MS, Yoon DH, Shin DA. Primary spinal cord
melanoma. J Korean Neurosurg Soc 2010;48:157-61. Crossref

